Scopolamine
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Transderm Scop, others |
| Other names | Hyoscine,[1] Devil's Breath |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682509 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth, transdermal, ophthalmic, subcutaneous, intravenous, sublingual, rectal, buccal, transmucosal, intramuscular |
| Drug class | |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 20-40%[7] |
| Metabolism | Liver (CYP3A4)[8] |
| Elimination half-life | 5 hours[7] |
| Excretion | Kidney |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII |
|
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.083 |
| Chemical and physical data | |
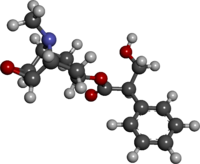
| Formula | C17H21NO4 |
| Molar mass | 303.358 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Scopolamine, also known as hyoscine,[9] or Devil's Breath,[10] is a natural or synthetically produced tropane alkaloid and anticholinergic drug that is used as a medication to treat motion sickness[11] and postoperative nausea and vomiting.[12][1] It is also sometimes used before surgery to decrease saliva.[1] When used by injection, effects begin after about 20 minutes and last for up to 8 hours.[1] It may also be used orally and as a transdermal patch since it has been long known to have transdermal bioavailability.[1][13]
Scopolamine is in the antimuscarinic family of drugs and works by blocking some of the effects of acetylcholine within the nervous system.[1]
Scopolamine was first written about in 1881 and started to be used for anesthesia around 1900.[14][15] Scopolamine is also the main active component produced by certain plants of the nightshade family, which historically have been used as psychoactive drugs, known as deliriants, due to their antimuscarinic-induced hallucinogenic effects in higher doses.[12] In these contexts, its mind-altering effects have been utilized for recreational and occult purposes.[16][17][18] The name "scopolamine" is derived from one type of nightshade known as Scopolia, while the name "hyoscine" is derived from another type known as Hyoscyamus niger, or black henbane.[19][20] It is on the World Health Organization's List of Essential Medicines.[21]
Medical uses
[edit]Scopolamine has a number of formal uses in modern medicine where it is used in its isolated form and in low doses to treat:[22][23]
- Postoperative nausea and vomiting
- Motion sickness, including sea sickness, leading to its use by scuba divers (where it is often applied as a transdermal patch behind the ear)[24][25][26][27]
- Gastrointestinal spasms
- Renal or biliary spasms
- Aid in gastrointestinal radiology and endoscopy
- Irritable bowel syndrome
- Clozapine-induced drooling
- Bowel colic
- Eye inflammation[28]
It is sometimes used as a premedication, especially to reduce respiratory tract secretions in surgery, most commonly by injection.[22][23] Common side effects include sleepiness, blurred vision, dilated pupils, and dry mouth.[1] It is not recommended in people with angle-closure glaucoma or bowel obstruction.[1] Whether its use during pregnancy is safe remains unclear, and use during breastfeeding is still cautioned by health professionals and manufacturers of the drug.[29]
Breastfeeding
[edit]Scopolamine enters breast milk by secretion. Although no human studies exist to document the safety of scopolamine while nursing, the manufacturer recommends that caution be taken if scopolamine is administered to a breastfeeding woman.[29]
Adverse effects
[edit]Adverse effect incidence:[6][30][31][32]
Uncommon (0.1–1% incidence) adverse effects include:
- Dry mouth
- Anhidrosis (reduced ability to sweat to cool off)
- Tachycardia (usually occurs at higher doses and is succeeded by bradycardia)
- Bradycardia
- Urticaria (hives)
- Pruritus (itching)
Rare (<0.1% incidence) adverse effects include:
- Constipation
- Urinary retention
- Hallucinations
- Agitation
- Confusion
- Restlessness
- Seizures
Unknown frequency adverse effects include:
- Anaphylactic shock or reactions
- Dyspnea (shortness of breath)
- Rash
- Erythema
- Other hypersensitivity reactions
- Blurred vision
- Mydriasis (dilated pupils)
- Drowsiness
- Dizziness
- Somnolence
Overdose
[edit]Physostigmine, a cholinergic drug that readily crosses the blood–brain barrier, has been used as an antidote to treat the central nervous system depression symptoms of a scopolamine overdose.[33] Other than this supportive treatment, gastric lavage and induced emesis (vomiting) are usually recommended as treatments for oral overdoses.[32] The symptoms of overdose include:[31][32]
- Tachycardia
- Arrhythmia
- Blurred vision
- Photophobia
- Urinary retention
- Drowsiness or paradoxical reaction, which can present with hallucinations
- Cheyne–Stokes respiration
- Dry mouth
- Skin reddening
- Inhibition of gastrointestinal motility
Route of administration
[edit]Scopolamine can be taken by mouth, subcutaneously, in the eye, and intravenously, as well as via a transdermal patch.[34]
Pharmacology
[edit]Pharmacodynamics
[edit]The pharmacological effects of scopolamine are mediated through the drug's competitive antagonism of the peripheral and central muscarinic acetylcholine receptors. Scopolamine acts as a nonspecific muscarinic antagonist at all four (M1, M2, M3, and M4) receptor sites.[35][36]
In doses higher than intended for medicinal use, the hallucinogenic alteration of consciousness, as well as the deliriousness in particular, are tied to the compound's activity at the M1 muscarinic receptor. M1 receptors are located primarily in the central nervous system and are involved in perception, attention and cognitive functioning. Delirium is only associated with the antagonism of postsynaptic M1 receptors and currently other receptor subtypes have not been implicated.[37]
Peripheral muscarinic receptors are part of the autonomic nervous system. M2 receptors are located in the brain and heart, M3 receptors are in salivary glands and M4 receptors are in the brain and lungs.[37] Due to the drug's inhibition of various signal transduction pathways, the decrease in acetylcholine signaling is what leads to many of the cognitive deficits, mental impairments and delirium associated with psychoactive doses. Medicinal effects appear to mostly be tied to activation of the peripheral receptors and only from marginal decreases in acetylcholine signaling.[38]
Although often broadly referred to as simply being 'anticholinergic', antimuscarinic would be more specific and accurate terminology to use for scopolamine, as, for example, it is not known to block nicotinic receptors.[37]
Pharmacokinetics
[edit]Scopolamine undergoes first-pass metabolism and about 2.6% is excreted unchanged in urine. It has a bioavailability of 20-40%, reaches peak plasma concentration in about 45 minutes, and in healthy subjects has an average half-life of 5 hours (observed range 2 - 10 hours).[7] Scopolamine is primarily metabolized by the CYP3A4 enzyme, and Grapefruit juice decreases metabolism of scopolamine, consequently increasing plasma concentration.[8]
Chemistry
[edit]Biosynthesis in plants
[edit]Scopolamine is among the secondary metabolites of plants from Solanaceae (nightshade) family of plants, such as henbane (Hyoscyamus niger), jimson weed (Datura), angel's trumpets (Brugmansia), deadly nightshade (Belladonna), mandrake (Mandragora officinarum), and corkwood (Duboisia).[39][19]

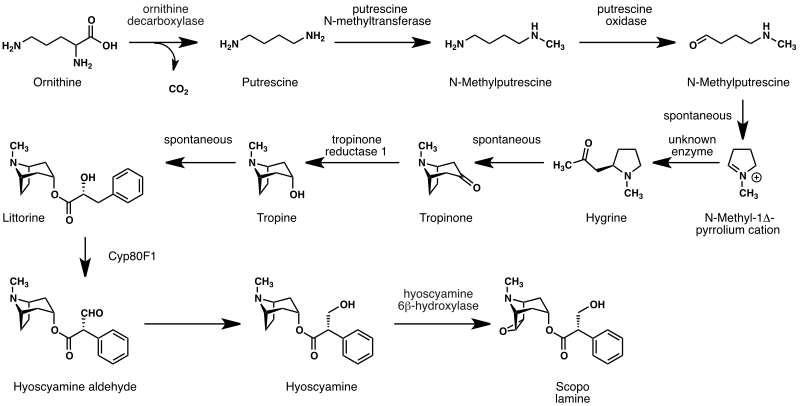
The biosynthesis of scopolamine begins with the decarboxylation of L-ornithine to putrescine by ornithine decarboxylase. Putrescine is methylated to N-methylputrescine by putrescine N-methyltransferase.[40]
A putrescine oxidase that specifically recognizes methylated putrescine catalyzes the deamination of this compound to 4-methylaminobutanal, which then undergoes a spontaneous ring formation to N-methyl-pyrrolium cation. In the next step, the pyrrolium cation condenses with acetoacetic acid yielding hygrine. No enzymatic activity could be demonstrated to catalyze this reaction. Hygrine further rearranges to tropinone.[40]
Subsequently, tropinone reductase I converts tropinone to tropine, which condenses with phenylalanine-derived phenyllactate to littorine. A cytochrome P450 classified as Cyp80F1[41] oxidizes and rearranges littorine to hyoscyamine aldehyde. In the final step, hyoscyamine undergoes epoxidation catalyzed by 6beta-hydroxyhyoscyamine epoxidase yielding scopolamine.[40]
History
[edit]Plants naturally containing scopolamine such as Atropa belladonna (deadly nightshade), Brugmansia (angels trumpet), Datura (Jimson weed), Hyoscyamus niger, Mandragora officinarum, Scopolia carniolica, Latua and Duboisia myoporoides have been known about and used for various purposes in both the New and Old Worlds since ancient times.[42][43][44] Being one of the earlier alkaloids isolated from plant sources, scopolamine has been in use in its purified forms, such as various salts, including hydrochloride, hydrobromide, hydroiodide, and sulfate, since its official isolation by the German scientist Albert Ladenburg in 1880,[45] and as various preparations from its plant-based form since antiquity and perhaps prehistoric times.
In 1899, a Dr. Schneiderlin recommended the use of scopolamine and morphine for surgical anaesthesia, and it started to be used sporadically for that purpose.[14][46] The use of this combination in obstetric anesthesiology (childbirth) was first proposed by Richard von Steinbuchel in 1902 and was picked up and further developed by Carl Gauss in Freiburg, Germany, starting in 1903.[47] The method, which was based on a drug synergy between both scopolamine and morphine came to be known as Dämmerschlaf ("twilight sleep") or the "Freiburg method".[46][47] It spread rather slowly, and different clinics experimented with different dosages and ingredients. In 1915, the Canadian Medical Association Journal reported, "the method [was] really still in a state of development".[46] It remained widely used in the US until the 1960s, when growing chemophobia and a desire for more natural childbirth led to its abandonment.[48]
Society and culture
[edit]Names
[edit]Hyoscine hydrobromide is the international nonproprietary name, and scopolamine hydrobromide is the United States Adopted Name. Other names include levo-duboisine, devil's breath, and burundanga.[17][49]
Australian bush medicine
[edit]A bush medicine developed by Aboriginal peoples of the eastern states of Australia from the soft corkwood tree (Duboisia myoporoides) was used by the Allies in World War II to stop soldiers from getting seasick when they sailed across the English Channel on their way to France during the Invasion of Normandy. Later, the same substance was found to be usable in the production of scopolamine and hyoscyamine, which are used in eye surgery, and a multimillion-dollar industry was built in Queensland based on this substance.[50]
Recreational and religious use
[edit]While it has been occasionally used recreationally for its hallucinogenic properties, the experiences are often unpleasant, mentally and physically. It is also physically dangerous and officially classified as a deliriant drug, so repeated recreational use is rare.[51] In June 2008, more than 20 people were hospitalized with psychosis in Norway after ingesting counterfeit rohypnol tablets containing scopolamine.[52] In January 2018, 9 individuals were hospitalized in Perth, Western Australia, after reportedly ingesting scopolamine.[53]
The alkaloid scopolamine, when taken recreationally for its psychoactive effect, is usually taken in the form of preparations from plants of the genera Datura or Brugmansia, often by adolescents or young adults in order to achieve hallucinations and an altered state of consciousness induced by muscarinic antagonism.[54][55] In circumstances such as these, the intoxication is usually built on a synergistic, but even more toxic mixture of the additional alkaloids in the plants which includes atropine and hyoscyamine.
Historically, the various plants that produce scopolamine have been used psychoactively for spiritual and magical purposes, particularly by witches in western culture and indigenous groups throughout the Americas, such as Native American tribes like the Chumash.[18][56][57][58] When entheogenic preparations of these plants were used, scopolamine was considered to be the main psychoactive compound and was largely responsible for the hallucinogenic effects, particularly when the preparation was made into a topical ointment, most notably flying ointment.[59]
Scopolamine is reported to be the only active alkaloid within these plants that can effectively be absorbed through the skin to cause effects.[13] Different recipes for these ointments were explored in European witchcraft at least as far back as the Early Modern period and included multiple ingredients to help with the transdermal absorption of scopolamine, such as animal fat, as well as other possible ingredients to counteract its noxious and dysphoric effects.[59]
In the Bible, there are multiple mentions of Mandrake, a psychoactive and hallucinogenic plant root that contains scopolamine. It was associated with fertility and (sexual) desire where it was yearned for by Rachel, who apparently was "barren" (infertile) but trying to conceive.[60][61]
Interrogation
[edit]The effects of scopolamine were studied for use as a truth serum in interrogations in the early 20th century,[62] but because of the side effects, investigations were dropped.[63] In 2009, the Czechoslovak state security secret police were proven to have used scopolamine at least three times to obtain confessions from alleged antistate dissidents.[64]
Use in crime
[edit]This article may need to be rewritten to comply with Wikipedia's quality standards. (August 2024) |
Ingestion of scopolamine can render a victim unconscious for 24 hours or more. In large doses, it can cause respiratory failure and death. The most common seems to be recorded in Colombia, where unofficial estimates put the number of annual scopolamine incidents at approximately 50,000. A travel advisory published by the U.S. Overseas Security Advisory Council (OSAC) in 2012 stated:
One common and particularly dangerous method that criminals use in order to rob a victim is through the use of drugs. Scopolamine is most often administered in liquid or powder form in foods and beverages. The majority of these incidents occur in night clubs and bars, and usually men, perceived to be wealthy, are targeted by young, attractive women. It is recommended that, to avoid becoming a victim of scopolamine, a person should never accept food or beverages offered by strangers or new acquaintances, nor leave food or beverages unattended in their presence. Victims of scopolamine or other drugs should seek immediate medical attention.[65]
Between 1998 and 2004, 13% of emergency-room admissions for "poisoning with criminal intentions" in a clinic of Bogotá have been attributed to scopolamine, and 44% to benzodiazepines.[17] Most commonly, the person has been poisoned by a robber who gave the victim a scopolamine-laced beverage, in the hope that the victim would become unconscious or unable to effectively resist the robbery.[17]
Beside robberies, it is also allegedly involved in express kidnappings and sexual assault.[66] In 2008, the Hospital Clínic in Barcelona introduced a protocol to help medical workers identify cases. In February 2015, Madrid hospitals adopted a similar working document.[66] Hospital Clínic has found little scientific evidence to support this use and relies on the victims' stories to reach any conclusion.[66]
Although poisoning by scopolamine appears quite often in the media as an aid for raping, kidnapping, killing, or robbery, the effects of this drug and the way it is applied by criminals (transdermal injection, on playing cards and papers, etc.) are often exaggerated,[67][68][69] especially skin exposure, as the dose that can be absorbed by the skin is too low to have any effect.[66] Scopolamine transdermal patches must be used for hours to days.[34]
There are certain other aspects of the usage of scopolamine in crimes. Powdered scopolamine is referred to as "devil's breath". In popular media and television, it is portrayed as a method to brainwash or control people into being defrauded by their attackers.[70] There is debate whether these claims are true.[71][72][73]
Research
[edit]Scopolamine is used as a research tool to study memory encoding. Initially, in human trials, relatively low doses of the muscarinic receptor antagonist scopolamine were found to induce temporary cognitive defects.[74] Since then, scopolamine has become a standard drug for experimentally inducing cognitive defects in animals.[75][76] Results in primates suggest that acetylcholine is involved in the encoding of new information into long-term memory.[77] Scopolamine has been shown to exert a greater impairment on episodic memory, event-related potentials, memory retention and free recall compared to diphenhydramine (an anticholinergic and antihistamine).[78]
Scopolamine produces detrimental effects on short-term memory, memory acquisition, learning, visual recognition memory, visuospatial praxis, visuospatial memory, visuoperceptual function, verbal recall, and psychomotor speed.[79][75][76] It does not seem to impair recognition and memory retrieval, though.[76] Acetylcholine projections in hippocampal neurons, which are vital in mediating long-term potentiation, are inhibited by scopolamine.[76][80] Scopolamine inhibits cholinergic-mediated glutamate release in hippocampal neurons, which assist in depolarization, potentiation of action potential, and synaptic suppression. Scopolamine's effects on acetylcholine and glutamate release in the hippocampus favor retrieval-dominant cognitive functioning.[76] Scopolamine has been used to model the defects in cholinergic function for models of Alzheimer's, dementia, fragile X syndrome, and Down syndrome.[76][81][82][83]
Scopolamine has been identified as a psychoplastogen, which refers to a compound capable of promoting rapid and sustained neuroplasticity in a single dose.[84] It has been, and continues to be investigated as a rapid-onset antidepressant, with a number of small studies finding positive results, particularly in female subjects.[85][86][87][88]
NASA agreed to develop a nasal administration method. With a precise dosage, the NASA spray formulation has been shown to work faster and more reliably than the oral form to treat motion sickness.[89]
Although a fair amount of research has been applied to scopolamine in the field of medicine, its hallucinogenic (psychoactive) effects as well as the psychoactive effects of other antimuscarinic deliriants haven't been extensively researched or as well understood compared to other types of hallucinogens such as psychedelic and dissociative compounds, despite the alkaloid's long history of usage in mind-altering plant preparations.[90]
References
[edit]- ^ a b c d e f g h "Scopolamine". The American Society of Health-System Pharmacists. Archived from the original on 7 October 2016. Retrieved 8 December 2016.
- ^ "Scopolamine Use During Pregnancy". Drugs.com. 6 September 2023. Archived from the original on 21 December 2016. Retrieved 21 June 2024.
- ^ "Poisons Standard October 2020". Federal Register of Legislation. 30 September 2020. Archived from the original on 25 January 2021. Retrieved 23 October 2020.
- ^ "Hyoscine 400 micrograms/ml Solution for Injection". (emc). 18 September 2017. Archived from the original on 8 November 2023. Retrieved 21 June 2024.
- ^ "Kwells 300 microgram tablets Summary of Product Characteristics (SmPC)". (emc). 2 September 2020. Archived from the original on 2 March 2024. Retrieved 21 June 2024.
- ^ a b "Transderm Scop - scopolamine patch, extended release". DailyMed. 14 March 2024. Archived from the original on 30 November 2023. Retrieved 21 June 2024.
- ^ a b c Putcha L, Cintrón NM, Tsui J, Vanderploeg JM, Kramer WG (June 1989). "Pharmacokinetics and oral bioavailability of scopolamine in normal subjects". Pharmaceutical Research. 06 (6): 481–485. doi:10.1023/A:1015916423156. PMID 2762223. S2CID 27507555.
- ^ a b Renner UD, Oertel R, Kirch W (October 2005). "Pharmacokinetics and pharmacodynamics in clinical use of scopolamine". Therapeutic Drug Monitoring. 27 (5): 655–665. doi:10.1097/01.ftd.0000168293.48226.57. PMID 16175141. S2CID 32720769.
- ^ Juo PS (2001). Concise Dictionary of Biomedicine and Molecular Biology (2nd ed.). Hoboken: CRC Press. p. 570. ISBN 978-1-4200-4130-9. Archived from the original on 10 September 2017.
- ^ Duffy R (23 July 2007). "Colombian Devil's Breath". Vice. Archived from the original on 18 April 2022. Retrieved 3 February 2022.
- ^ "About hyoscine hydrobromide". nhs.uk. 24 October 2022. Archived from the original on 14 March 2023. Retrieved 14 March 2023.
- ^ a b Osbourn AE, Lanzotti V (2009). Plant-derived Natural Products: Synthesis, Function, and Application. Springer Science & Business Media. p. 5. ISBN 978-0-387-85498-4. Archived from the original on 10 September 2017.
- ^ a b Sollmann T (1957). A Manual of Pharmacology and Its Applications to Therapeutics and Toxicology (8th ed.). Philadelphia and London: W.B. Saunders.
- ^ a b Keys TE (1996). The history of surgical anesthesia (PDF) (Reprint ed.). Park Ridge, Ill.: Wood Library, Museum of Anesthesiology. p. 48ff. ISBN 978-0-9614932-7-1. Archived (PDF) from the original on 19 April 2022. Retrieved 26 July 2022.
- ^ Fischer J, Ganellin CR (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 551. ISBN 978-3-527-60749-5.
- ^ Kennedy DO (2014). "The Deliriants - The Nightshade (Solanaceae) Family". Plants and the Human Brain. New York: Oxford University Press. pp. 131–137. ISBN 978-0-19-991401-2. LCCN 2013031617. Archived from the original on 17 September 2021. Retrieved 17 September 2021.
- ^ a b c d Uribe-Granja MG, Moreno-López CL, Zamora-Suárez A, Acosta PJ (September 2005). "Perfil epidemiológico de la intoxicación con burundanga en la clínica Uribe Cualla S. A. de Bogotá, D. C." [Epidemiological profile of burundanga poisoning at the Uribe Cualla SA clinic in Bogotá, D. C.] (PDF). Acta Neurológica Colombiana (in Spanish). 21 (3): 197–201. Archived from the original on 3 July 2024. Retrieved 1 July 2024.
- ^ a b Raetsch C (2005). The encyclopedia of psychoactive plants: ethnopharmacology and its applications. US: Park Street Press. pp. 277–282.
- ^ a b The Chambers Dictionary. Allied Publishers. 1998. pp. 788, 1480. ISBN 978-81-86062-25-8.
- ^ Cattell HW (1910). Lippincott's new medical dictionary: a vocabulary of the terms used in medicine, and the allied sciences, with their pronunciation, etymology, and signification, including much collateral information of a descriptive and encyclopedic character. Lippincott. p. 435. Archived from the original on 10 September 2017. Retrieved 25 February 2012.
- ^ World Health Organization (2023). The selection and use of essential medicines 2023: web annex A: World Health Organization model list of essential medicines: 23rd list (2023). Geneva: World Health Organization. hdl:10665/371090. WHO/MHP/HPS/EML/2023.02.
- ^ a b Joint Formulary Committee (2013). British National Formulary (BNF) (65 ed.). London, UK: Pharmaceutical Press. pp. 49, 266, 822, 823. ISBN 978-0-85711-084-8.
- ^ a b Rossi S, ed. (2013). Australian Medicines Handbook (2013 ed.). Adelaide: The Australian Medicines Handbook Unit Trust. ISBN 978-0-9805790-9-3.
- ^ Bitterman N, Eilender E, Melamed Y (May 1991). "Hyperbaric oxygen and scopolamine". Undersea Biomedical Research. 18 (3): 167–174. PMID 1853467. Archived from the original on 20 August 2008. Retrieved 13 August 2008.
{{cite journal}}: CS1 maint: unfit URL (link) - ^ Williams TH, Wilkinson AR, Davis FM, Frampton CM (March 1988). "Effects of transcutaneous scopolamine and depth on diver performance". Undersea Biomedical Research. 15 (2): 89–98. PMID 3363755. Archived from the original on 20 August 2008.
{{cite journal}}: CS1 maint: unfit URL (link) - ^ Williams TH, Wilkinson AR, Davis FM, Frampton CM (March 1988). "Effects of transcutaneous scopolamine and depth on diver performance". Undersea Biomedical Research. 15 (2): 89–98. PMID 3363755.
- ^ "Motion Sickness". Divers Alert Network. Archived from the original on 6 November 2022. Retrieved 6 November 2022.
- ^ "scopolamine solution - ophthalmic, Isopto". MedicineNet.com. Archived from the original on 31 March 2019. Retrieved 12 February 2019.
- ^ a b Briggs GG, Freeman RK, Yaffe SJ (1994). "Scopolamine". Drugs in Pregnancy and Lactation. Baltimore, Maryland: Williams and Wilkins. pp. 777–778. ISBN 978-0-683-01060-2.
- ^ "DBL HYOSCINE INJECTION BP". TGA eBusiness Services. Hospira Australia Pty Ltd. 30 January 2012. Archived from the original on 30 March 2017. Retrieved 22 October 2013.
- ^ a b "Buscopan Tablets - Summary of Product Characteristics (SPC)". electronic Medicines Compendium. Boehringer Ingelheim Limited. 11 September 2013. Archived from the original on 23 October 2013. Retrieved 22 October 2013.
- ^ a b c "Kwells 300 microgram tablets - Summary of Product Characteristics". electronic Medicines Compendium. Bayer plc. 7 January 2008. Archived from the original on 23 October 2013. Retrieved 22 October 2013.
- ^ Barash PG, Cahalan M, Cullen BF, Stock MC, Stoelting RK, eds. (2009). Clinical anesthesia (6th ed.). Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins. p. 346. ISBN 978-0-7817-8763-5.
- ^ a b White PF, Tang J, Song D, Coleman JE, Wender RH, Ogunnaike B, et al. (January 2007). "Transdermal scopolamine: an alternative to ondansetron and droperidol for the prevention of postoperative and postdischarge emetic symptoms". Anesthesia and Analgesia. 104 (1): 92–96. doi:10.1213/01.ane.0000250364.91567.72. PMID 17179250. S2CID 44784425.
- ^ "Google Scholar". scholar.google.com. Archived from the original on 30 October 2020. Retrieved 16 December 2017.[ambiguous]
- ^ "PDSP Ki Database". Archived from the original on 23 July 2020. Retrieved 23 July 2020.
- ^ a b c Dawson AH, Buckley NA (March 2016). "Pharmacological management of anticholinergic delirium - theory, evidence and practice". British Journal of Clinical Pharmacology. 81 (3): 516–524. doi:10.1111/bcp.12839. PMC 4767198. PMID 26589572.
Delirium is only associated with the antagonism of post‐synaptic M1 receptors and to date other receptor subtypes have not been implicated
- ^ Lessenger JE, Feinberg SD (2008). "Abuse of prescription and over-the-counter medications". Journal of the American Board of Family Medicine. 21 (1): 45–54. doi:10.3122/jabfm.2008.01.070071. PMID 18178702.
- ^ Muranaka T, Ohkawa H, Yamada Y (1993). "Continuous Production of Scopolamine by a Culture of Duboisia leichhardtii Hairy Root Clone in a Bioreactor System". Applied Microbiology and Biotechnology. 40 (2–3): 219–223. doi:10.1007/BF00170370. S2CID 45125074.
- ^ a b c Ziegler J, Facchini PJ (2008). "Alkaloid biosynthesis: metabolism and trafficking". Annual Review of Plant Biology. 59 (1): 735–769. doi:10.1146/annurev.arplant.59.032607.092730. PMID 18251710.
- ^ Li R, Reed DW, Liu E, Nowak J, Pelcher LE, Page JE, et al. (May 2006). "Functional genomic analysis of alkaloid biosynthesis in Hyoscyamus niger reveals a cytochrome P450 involved in littorine rearrangement". Chemistry & Biology. 13 (5): 513–520. doi:10.1016/j.chembiol.2006.03.005. PMID 16720272.
- ^ Armando T. Hunziker: The Genera of Solanaceae. A.R.G. Gantner Verlag K.G., Ruggell, Liechtenstein 2001. ISBN 3-904144-77-4
- ^ Rätsch, Christian, The Encyclopedia of Psychoactive Plants: Ethnopharmacology and Its Applications pub. Park Street Press 2005
- ^ "Pharmacognosy and Phytochemistry : Drugs Containing Alkaloids". Archived from the original on 20 December 2022. Retrieved 16 December 2022.
- ^ Ladenburg A (January 1881). "Die natürlich vorkommenden mydriatisch wirkenden Alkaloïde" [The naturally occurring mydriatic alkaloids]. Justus Liebigs Annalen der Chemie (in German). 206 (3): 274–307. doi:10.1002/jlac.18812060303.
- ^ a b c "Twilight Sleep: the Dammerschlaf of the Germans". Canadian Medical Association Journal. 5 (9): 805–808. September 1915. PMC 1584452. PMID 20310688.
- ^ a b "TWILIGHT SLEEP; Is Subject of a New Investigation". The New York Times. 31 January 1915. Archived from the original on 22 April 2023. Retrieved 27 June 2024.
- ^ Finkbeiner A (31 October 1999). "Labor Dispute. Book review: What a Blessing She Had Chloroform: The Medical and Social Response to the Pain of Childbirth from 1800 to the Present". The New York Times. Archived from the original on 30 October 2020. Retrieved 17 June 2018.
- ^ Bell V (3 March 2011). "Mind controller: What is the 'burundanga' drug?". Wired UK (published April 2011). Archived from the original on 11 August 2017.
- ^ "Visitors to Art of Healing exhibition told how Australian Indigenous bush medicine was given to every allied soldier landing at Normandy on D-Day". King's College London. 7 June 2019. Archived from the original on 2 June 2020. Retrieved 2 June 2020.
- ^ Freye E (2010). "Toxicity of Datura Stramonium". Pharmacology and Abuse of Cocaine, Amphetamines, Ecstasy and Related Designer Drugs. Netherlands: Springer. pp. 217–218. doi:10.1007/978-90-481-2448-0_34. ISBN 978-90-481-2447-3.
- ^ "Bilsykemedisin i falske rohypnol-tabletter". Aftenposten.no. Archived from the original on 27 June 2008.
- ^ "Perth backpacker overdose linked to common anti-nausea drug". ABC News. 4 January 2018. Archived from the original on 7 November 2020. Retrieved 4 January 2018.
- ^ Fatur K, Kreft S (April 2020). "Common anticholinergic solanaceaous plants of temperate Europe - A review of intoxications from the literature (1966-2018)". Toxicon. 177: 52–88. Bibcode:2020Txcn..177...52F. doi:10.1016/j.toxicon.2020.02.005. PMID 32217234. S2CID 213559151.
- ^ Preissel U, Preissel HG (2002). Brugmansia and Datura: Angel's Trumpets and Thorn Apples. Buffalo, NY: Firefly Books. pp. 106–129. ISBN 1-55209-598-3.
- ^ Harner M (1980). The Way of the Shaman. New York: Harper & Row. ISBN 978-0-06-250373-2.
- ^ Kuklin A (February 1999). How Do Witches Fly?. DNA Press. ISBN 0-9664027-0-7.
- ^ Applegate RB (1975). "The Datura Cult Among the Chumash". The Journal of California Anthropology. 2 (1): 7–17. JSTOR 27824805.
- ^ a b Hansen, Harold A. The Witch's Garden pub. Unity Press 1978 ISBN 978-0913300473
- ^ "Genesis 30:14–16 (King James Version)". Bible Gateway. Archived from the original on 7 January 2014. Retrieved 6 January 2014.
- ^ "Song of Songs 7:12–13 (King James Version)". Bible Gateway. Archived from the original on 7 January 2014. Retrieved 6 January 2014.
- ^ House RE (September 1922). "The Use of Scopolamine in Criminology". Texas State Journal of Medicine. 18: 256–263.
Reprinted in: House RE (July–August 1931). "The Use of Scopolamine in Criminology". American Journal of Police Science. 2 (4): 328–336. doi:10.2307/1147361. JSTOR 1147361. - ^ Bimmerle G (22 September 1993). "'Truth' Drugs in Interrogation". CIA.gov. Central Intelligence Agency. Archived from the original on 27 September 2012. Retrieved 14 June 2012.
- ^ Gazdík J, Navara L (8 August 2009). "Svědek: Grebeníček vězně nejen mlátil, ale dával jim i drogy" [A witness: Grebeníček not only beat prisoners, he also administered drugs to them] (in Czech). iDnes. Archived from the original on 11 August 2009. Retrieved 10 August 2009.
- ^ "Colombia 2012 Crime and Safety Report: Cartagena". Overseas Security Advisory Council, United States Department of State. 4 March 2012. Archived from the original on 15 March 2013. Retrieved 6 August 2015.
- ^ a b c d Domínguez I (25 July 2016). "Burundanga: the stealth drug that cancels the victim's willpower". Crime. El País, Madrid. Archived from the original on 20 August 2016. Retrieved 12 August 2016.
- ^ "Burundanga Business Card Drug Warning". Hoax-Slayer.com. 12 October 2008. Archived from the original on 7 March 2009.
- ^ "Beware the Burundanga Man!". About.com Entertainment. Archived from the original on 10 January 2017. Retrieved 19 December 2016.
- ^ Mikkelson D. "Burundanga/Scopolamine Warning". snopes.com. Retrieved 19 December 2016.
- ^ Reichert S, Lin C, Ong W, Him CC, Hameed S (May 2017). "Million dollar ride: Crime committed during involuntary scopolamine intoxication" (PDF). Canadian Family Physician. 63 (5): 369–370. PMC 5429053. PMID 28500194. Archived (PDF) from the original on 22 April 2021.
- ^ Anderson L. "Devil's Breath: Urban Legend or the World's Most Scary Drug?". Drugs.com. Archived from the original on 23 June 2019. Retrieved 9 July 2019.
- ^ Saner E (2 September 2015). "'Devil's breath' aka scopolamine: can it really zombify you?". The Guardian. Archived from the original on 4 January 2019. Retrieved 4 January 2019.
- ^ Mikkelson B (11 May 2008). "FACT CHECK: Burundanga/Scopolamine Warning". Snopes. Retrieved 1 August 2024.
- ^ Drachman DA, Leavitt J (February 1974). "Human memory and the cholinergic system. A relationship to aging?". Archives of Neurology. 30 (2): 113–121. doi:10.1001/archneur.1974.00490320001001. PMID 4359364.
- ^ a b Hasselmo ME, Wyble BP (December 1997). "Free recall and recognition in a network model of the hippocampus: simulating effects of scopolamine on human memory function". Behavioural Brain Research. 89 (1–2): 1–34. doi:10.1016/s0166-4328(97)00048-x. PMID 9475612. S2CID 584350.
- ^ a b c d e f More SV, Kumar H, Cho DY, Yun YS, Choi DK (September 2016). "Toxin-Induced Experimental Models of Learning and Memory Impairment". International Journal of Molecular Sciences. 17 (9): 1447. doi:10.3390/ijms17091447. PMC 5037726. PMID 27598124.
- ^ Ridley RM, Bowes PM, Baker HF, Crow TJ (1984). "An involvement of acetylcholine in object discrimination learning and memory in the marmoset". Neuropsychologia. 22 (3): 253–263. doi:10.1016/0028-3932(84)90073-3. PMID 6431311. S2CID 7110504.
- ^ Curran HV, Pooviboonsuk P, Dalton JA, Lader MH (January 1998). "Differentiating the effects of centrally acting drugs on arousal and memory: an event-related potential study of scopolamine, lorazepam and diphenhydramine". Psychopharmacology. 135 (1): 27–36. doi:10.1007/s002130050482. PMID 9489931. S2CID 9872819.
- ^ Flicker C, Serby M, Ferris SH (February 1990). "Scopolamine effects on memory, language, visuospatial praxis and psychomotor speed". Psychopharmacology. 100 (2): 243–250. doi:10.1007/bf02244414. PMID 2305013. S2CID 24645744.
- ^ Lisboa SF, Vila-Verde C, Rosa J, Uliana DL, Stern CA, Bertoglio LJ, et al. (January 2019). "Tempering aversive/traumatic memories with cannabinoids: a review of evidence from animal and human studies". Psychopharmacology. 236 (1): 201–226. doi:10.1007/s00213-018-5127-x. PMID 30604182. S2CID 58655082.
- ^ Qin M, Zeidler Z, Moulton K, Krych L, Xia Z, Smith CB (September 2015). "Endocannabinoid-mediated improvement on a test of aversive memory in a mouse model of fragile X syndrome". Behavioural Brain Research. 291: 164–171. doi:10.1016/j.bbr.2015.05.003. PMC 5003021. PMID 25979787.
- ^ Lott IT (2012). "Neurological phenotypes for Down syndrome across the life span". Down Syndrome: From Understanding the Neurobiology to Therapy. Progress in Brain Research. Vol. 197. pp. 101–21. doi:10.1016/b978-0-444-54299-1.00006-6. ISBN 978-0-444-54299-1. PMC 3417824. PMID 22541290.
- ^ Lagalwar S, Bordayo EZ, Hoffmann KL, Fawcett JR, Frey WH (1999). "Anandamides inhibit binding to the muscarinic acetylcholine receptor". Journal of Molecular Neuroscience. 13 (1–2): 55–61. doi:10.1385/jmn:13:1-2:55. PMID 10691292. S2CID 22731716.
- ^ Olson DE (19 September 2018). "Psychoplastogens: A Promising Class of Plasticity-Promoting Neurotherapeutics". Journal of Experimental Neuroscience. 12: 1179069518800508. doi:10.1177/1179069518800508. PMC 6149016. PMID 30262987. S2CID 52877093.
- ^ Drevets WC, Zarate CA, Furey ML (June 2013). "Antidepressant effects of the muscarinic cholinergic receptor antagonist scopolamine: a review". Biological Psychiatry. 73 (12): 1156–1163. doi:10.1016/j.biopsych.2012.09.031. PMC 4131859. PMID 23200525.
- ^ Hasselmann H (2014). "Scopolamine and depression: a role for muscarinic antagonism?". CNS & Neurological Disorders Drug Targets. 13 (4): 673–683. doi:10.2174/1871527313666140618105710. PMID 24938776.
- ^ Jaffe RJ, Novakovic V, Peselow ED (2013). "Scopolamine as an antidepressant: a systematic review". Clinical Neuropharmacology. 36 (1): 24–26. doi:10.1097/wnf.0b013e318278b703. PMID 23334071. S2CID 19740245.
- ^ Wohleb ES, Wu M, Gerhard DM, Taylor SR, Picciotto MR, Alreja M, et al. (July 2016). "GABA interneurons mediate the rapid antidepressant-like effects of scopolamine". The Journal of Clinical Investigation. 126 (7): 2482–2494. doi:10.1172/JCI85033. PMC 4922686. PMID 27270172.
- ^ "NASA Signs Agreement to Develop Nasal Spray for Motion Sickness". NASA (Press release). 26 July 2023. Archived from the original on 15 June 2024. Retrieved 21 June 2024.
- ^ Volgin AD, Yakovlev OA, Demin KA, Alekseeva PA, Kyzar EJ, Collins C, et al. (January 2019). "Understanding Central Nervous System Effects of Deliriant Hallucinogenic Drugs through Experimental Animal Models". ACS Chemical Neuroscience. 10 (1): 143–154. doi:10.1021/acschemneuro.8b00433. PMID 30252437. S2CID 52824516.
External links
[edit] Media related to Scopolamine at Wikimedia Commons
Media related to Scopolamine at Wikimedia Commons
- Carboxylate esters
- Deliriants
- Entheogens
- Epoxides
- Experimental antidepressants
- M1 receptor antagonists
- M2 receptor antagonists
- M3 receptor antagonists
- M4 receptor antagonists
- M5 receptor antagonists
- Motion sickness
- Ophthalmology drugs
- Plant toxins
- Tropane alkaloids found in Solanaceae
- Tropane alkaloids
- World Health Organization essential medicines
