User:9pharmch/sandbox
 | This is a user sandbox of 9pharmch. A user sandbox is a subpage of the user's user page. It serves as a testing spot and page development space for the user and is not an encyclopedia article. |
- "inah" redirects here; for "INAH" see: Instituto Nacional de Antropología e Historia
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Hydra, Isovit, Laniazid, Nydrazid |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682401 |
| Pregnancy category |
|
| Routes of administration | oral, intramuscular, intravenous |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Protein binding | Very low (0-10%) |
| Metabolism | liver; CYP450: 2C19, 3A4 inhibitor |
| Elimination half-life | 0.5-1.6h (fast acetylators), 2-5h (slow acetylators) |
| Excretion | urine (primarily), feces |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| NIAID ChemDB | |
| Chemical and physical data | |
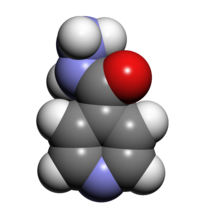
| Formula | C6H7N3O |
| Molar mass | 137.139 g/mol g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Isoniazid, marketed under numerous brand names, including Hydra among others, also known as isonicotinylhydrazide (or INH), is an organic compound that is the first-line medication in prevention and treatment of tuberculosis. Isoniazid is available in tablet, syrup, and injectable forms (given intramuscularly or intravenously).
The compound was first synthesized in the early 20th century,[1] but its activity against tuberculosis was first reported in the early 1950s, and three pharmaceutical companies attempted unsuccessfully to patent the drug simultaneously,[2] the most prominent one being Roche, which launched its version, Rimifon, in 1952.[3] With the introduction of isoniazid, a cure for tuberculosis was first considered to be possible. It is available worldwide, is inexpensive, and is generally well tolerated. It is on the World_Health_Organization's_List_of_Essential_Medicines, a list of medicines that constitute the bare minimum for a basic health system.[4]
Side effects
[edit]This section needs additional citations for verification. (May 2014) |
Adverse reactions include Rash, abnormal Liver_function_tests, Hepatitis, Sideroblastic_anemia, High_anion_gap_metabolic_acidosis, Peripheral_neuropathy, mild central nervous system (CNS) effects, drug interactions resulting in increased Phenytoin (Dilantin) or Disulfiram (Antabuse) levels, intractable seizures (Status_epilepticus) and Drug-induced_lupus_erythematosus.[citation needed]
Peripheral_neuropathy and CNS effects are associated with the use of isoniazid and are due to Pyridoxine (vitamin B6) depletion, but are uncommon at doses of 5 mg/kg.[citation needed] Persons with conditions in which neuropathy is common (e.g., Diabetes, Uremia, Alcoholism, Malnutrition, and HIV infection), as well as Pregnant women and persons with a Seizure disorder, may be given pyridoxine (10–50 mg/day) with isoniazid.
Isoniazid may cause severe and sometimes fatal liver damage.[citation needed] Hepatotoxicity can be avoided with close clinical monitoring of the patient, to be specific, nausea, vomiting, abdominal pain, and loss of appetite. Isoniazid is metabolized by the liver mainly by Acetylation and dehydrazination. The N-acetylhydrazine metabolite is believed to be responsible for the hepatotoxic effects seen in patients treated with isoniazid. The rate of acetylation is genetically determined. About 50% of Black and Caucasian people are slow inactivators; the majority of Inuit and Asians are rapid inactivators. The half-life in fast acetylators is one to two hours, while in slow acetylators, it is two to five hours. Elimination is largely independent of renal function, but the half-life may be prolonged in liver disease. The rate of acetylation has not been shown to significantly alter the effectiveness of isoniazid. However, slow acetylation may lead to higher blood concentrations with chronic administration of the drug, with an increased risk of toxicity. Fast acetylation leads to higher blood levels of the toxic metabolite acetylisoniazid and thus to an increase in toxic reactions - hepatitis which is 250 times more common than in slow acetylators. Isoniazid and its metabolites are excreted in the urine, with 75 to 95% of the dose excreted in 24 hours. Small amounts are also excreted in saliva, sputum, and feces. Isoniazid is removed by hemodialysis and peritoneal dialysis.[5]
Headache, poor concentration, weight gain, poor memory, insomnia, and depression have all been associated with isoniazid use.[citation needed] All patients and healthcare workers should be aware of these serious adverse effects, especially if suicidal thinking or behavior are suspected.[6][7][8]
INH is known to reduce cytochrome P450, and in theory promotes the efficacy of contraceptives.[citation needed] Therapy is often combined with Rifampin. Rifampin increases the P450 enzyme and also can reduce the efficacy of contraceptives. Alternative means of birth control should be used when taking these medications.
As previously mentioned, isoniazid is associated with pyridoxine deficiency. Pyridoxyl phosphate (derivative of pyridoxine) is required for d-aminolevulinic acid synthase, the enzyme responsible for the rate-limiting step in heme synthesis. As such, isoniazid-induced pyridoxine deficiency leads to insufficient heme formation in early red blood cells, leading to Sideroblastic_anemia.
Mechanism of action
[edit]Isoniazid is a Prodrug and must be activated by a bacterial catalase-peroxidase enzyme that in Mycobacterium_tuberculosis is called KatG.[9] KatG couples the isonicotinic acyl with NADH to form isonicotinic acyl-NADH complex. This complex binds tightly to the Enoyl-acyl_carrier_protein_reductase known as InhA, thereby blocking the natural enoyl-AcpM substrate and the action of Fatty_acid_synthase. This process inhibits the synthesis of Mycolic_acid, required for the mycobacterial cell wall. A range of radicals are produced by KatG activation of isoniazid, including Nitric_oxide,[10] which has also been shown to be important in the action of another antimycobacterial prodrug Pretomanid.[11]
Isoniazid is Bactericidal to rapidly dividing mycobacteria, but is Bacteriostatic if the mycobacteria are slow-growing.[12] It inhibits the P450_system and hence acts as a source of free radicals.[13]
Metabolism
[edit]Isoniazid reaches therapeutic concentrations in serum, Cerebrospinal_fluid, and within caseous granulomas. It is metabolized in the liver via Acetylation. Two forms of the enzyme are responsible for acetylation, so some patients metabolize the drug more quickly than others. Hence, the Half-life is bimodal, with peaks at one and three hours in the US population. The metabolites are excreted in the urine. Doses do not usually have to be adjusted in case of Renal_failure.
Manufacture
[edit]Isoniazid is manufactured from Isonicotinic_acid, which is produced from 4-methylpyridine.[14]
History
[edit]The drug was first tested at Many Farms, a Navajo community, due to the Navajo reservation's tuberculosis problem and because the population had not previously been treated with Streptomycin, the main tuberculosis treatment at the time.[15]
Names
[edit]- H (for "hydrazide", and also the WHO standard abbreviation)
- INH
- INHA
- Isonicotinic acid hydrazide
- Isonicotinyl hydrazine
See also
[edit]References
[edit]- ^ Meyer H, Mally J (1912). "On hydrazine derivatives of pyridine carbonic acids" (PDF). Monatshefte Chemie verwandte Teile anderer Wissenschaften (in German). 33 (4): 393–414. doi:10.1007/BF01517946.
- ^ Hans L Riede (2009). "Fourth-generation fluoroquinolones in tuberculosis". Lancet. 373 (9670): 1148–1149. doi:10.1016/S0140-6736(09)60559-6. PMID 19345815.
- ^ Roche USA
- ^ "WHO Model List of Essential Medicines" (PDF). World Health Organization. October 2013. Retrieved 2 February 2015.
- ^ http://www.rxmed.com/b.main/b2.pharmaceutical/b2.1.monographs/CPS-%20Monographs/CPS-%20(General%20Monographs-%20I)/ISONIAZID.html
- ^ Alao AO, Yolles JC (September 1998). "Isoniazid-induced psychosis". The Annals of Pharmacotherapy. 32 (9): 889–91. doi:10.1345/aph.17377. PMID 9762376.
- ^ Iannaccone, R; Sue, YJ; Avner, JR (2002). "Suicidal psychosis secondary to isoniazid". Pediatric emergency care. 18 (1): 25–7. doi:10.1097/00006565-200202000-00008. PMID 11862134.
- ^ Pallone KA, Goldman MP, Fuller MA (February 1993). "Isoniazid-associated psychosis: case report and review of the literature". The Annals of Pharmacotherapy. 27 (2): 167–70. PMID 8439690.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Suarez J, Ranguelova K, Jarzecki AA, et al. (March 2009). "An oxyferrous heme/protein-based radical intermediate is catalytically competent in the catalase reaction of Mycobacterium tuberculosis catalase-peroxidase (KatG)". The Journal of Biological Chemistry. 284 (11): 7017–29. doi:10.1074/jbc.M808106200. PMC 2652337. PMID 19139099.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Timmins GS, Master S, Rusnak F, Deretic V (August 2004). "Nitric oxide generated from isoniazid activation by KatG: source of nitric oxide and activity against Mycobacterium tuberculosis". Antimicrobial Agents and Chemotherapy. 48 (8): 3006–9. doi:10.1128/AAC.48.8.3006-3009.2004. PMC 478481. PMID 15273113.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Singh R, Manjunatha U, Boshoff HI, et al. (November 2008). "PA-824 kills nonreplicating Mycobacterium tuberculosis by intracellular NO release". Science. 322 (5906): 1392–5. doi:10.1126/science.1164571. PMC 2723733. PMID 19039139.
- ^ Ahmad, Z.; Klinkenberg, L. G.; Pinn, M. L.; Fraig, M. M.; Peloquin, C. A.; Bishai, W. R.; Nuermberger, E. L.; Grosset, J. H.; Karakousis, P. C. (2009). "Biphasic Kill Curve of Isoniazid Reveals the Presence of Drug‐Tolerant, Not Drug‐Resistant,Mycobacterium tuberculosisin the Guinea Pig". The Journal of Infectious Diseases. 200 (7): 1136–1143. doi:10.1086/605605. PMID 19686043.
- ^ Harvey (November 2009). Pharmacology (4th ed.).
- ^ Shinkichi Shimizu, Nanao Watanabe, Toshiaki Kataoka, Takayuki Shoji, Nobuyuki Abe, Sinji Morishita, Hisao Ichimura (2007). "Pyridine and Pyridine Derivatives". Ullmann's Encyclopedia of Industrial Chemistry. New York: John Wiley & Sons. doi:10.1002/14356007.a22_399.
{{cite book}}: CS1 maint: multiple names: authors list (link)[page needed] - ^ Jones, David (2002). "The Health Care Experiments at Many Farms: The Navajo, Tuberculosis, and the Limits of Modern Medicine, 1952-1962". Bulletin of the History of Medicine. 76 (4): 749–790. doi:10.1353/bhm.2002.0186. PMID 12446978.
External links
- Core Curriculum on Tuberculosis (2000) Division of Tuberculosis Elimination, Centers for Disease Control and Prevention
- See Chapter 6, Treatment of LTBI Regimens - Isoniazid::
See Chapter 7 - Treatment of TB Disease Monitoring - Adverse Reactions to First-line TB Drugs - Isoniazid::
See Table 5 First-Line Anti-TB Medications
- See Chapter 6, Treatment of LTBI Regimens - Isoniazid::
- Core Curriculum on Tuberculosis (2000) Division of Tuberculosis Elimination, Centers for Disease Control and Prevention
- Isoniazid Overdose: Recognition and Management American Family Physician 1998 Feb 15
