Labetalol
 | |
| Clinical data | |
|---|---|
| Pronunciation | /ləˈbɛtəlɔːl/ |
| Trade names | Normodyne, Trandate, others |
| Other names | Ibidomide; AH-5158; SCH-19927 |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a685034 |
| License data | |
| Pregnancy category |
|
| Routes of administration | By mouth, intravenous |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 25% (11–86%)[1][2][3] |
| Protein binding | 50%[1][3] |
| Metabolism | Mainly conjugation via glucuronidation[1][2][3] |
| Metabolites | • Glucuronide conjugates[2] |
| Elimination half-life | Oral: 6–8 hours[1][2][3] IV: 5.52 hours[2] |
| Duration of action | 8–12 hours[1] |
| Excretion | Urine (55–60% as conjugates or unchanged within 24 hours)[1] |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.048.401 |
| Chemical and physical data | |
| Formula | C19H24N2O3 |
| Molar mass | 328.412 g·mol−1 |
| 3D model (JSmol) | |
| Chirality | Racemic mixture |
| |
| |
| (verify) | |
Labetalol is a medication used to treat high blood pressure and in long term management of angina.[4][5] This includes essential hypertension, hypertensive emergencies, and hypertension of pregnancy.[5] In essential hypertension it is generally less preferred than a number of other blood pressure medications.[4] It can be given by mouth or by injection into a vein.[4]
Common side effects include low blood pressure with standing, dizziness, feeling tired, and nausea.[4] Serious side effects may include low blood pressure, liver problems, heart failure, and bronchospasm.[4] Use appears safe in the latter part of pregnancy and it is not expected to cause problems during breastfeeding.[5][6] It works by blocking the activation of β- and α-adrenergic receptors.[4]
Labetalol was patented in 1966 and came into medical use in 1977.[7] It is available as a generic medication.[5] In 2021, it was the 213th most commonly prescribed medication in the United States, with more than 2 million prescriptions.[8][9]
Medical uses
[edit]Labetalol is effective in the management of hypertensive emergencies, postoperative hypertension, pheochromocytoma-associated hypertension, and rebound hypertension from beta blocker withdrawal.[10]
It has a particular indication in the treatment of pregnancy-induced hypertension which is commonly associated with pre-eclampsia.[11]
It is also used as an alternative in the treatment of severe hypertension.[10]
Labetalol is useful in the treatment of acute cardiovascular toxicity (e.g. in overdose) caused by sympathomimetics like amphetamine, methamphetamine, cocaine, ephedrine, and pseudoephedrine.[12][13] Other beta blockers are also used.[12][13] However, the controversial yet possible phenomenon of "unopposed α-stimulation" with administration of selective beta blockers to block non-selective sympathomimetics potentially makes dual alpha-1 and beta blockers like labetalol and carvedilol more favorable for such purposes.[12][13] The rate of unopposed α-stimulation with selective beta blockers has been reported to be 0.4%,[12] whereas no cases of unopposed α-stimulation have been reported with dual alpha and beta blockers like labetalol.[13]
Special populations
[edit]Pregnancy: studies in lab animals showed no harm to the baby. However, a comparable well-controlled study has not been performed in pregnant women.[1]
Nursing: breast milk has been shown to contain small amounts of labetalol (0.004% original dose). Prescribers should be cautious in the use of labetalol for nursing mothers.[1]
Pediatric: no studies have established safety or usefulness in this population.[1]
Geriatric: the elderly are more likely to experience dizziness when taking labetalol. Labetalol should be dosed with caution in the elderly and counseled on this side effect.[1]
Side effects
[edit]Common
[edit]- Neurologic: headache (2%), dizziness (11%)[1]
- Gastrointestinal: nausea (6%), dyspepsia (3%)[1]
- Cholinergic: nasal congestion (3%), ejaculation failure (2%)[1]
- Respiratory: dyspnea (2%)[1]
- Other: fatigue (5%), vertigo (2%), orthostatic hypotension[1]
Low blood pressure with standing is more severe and more common with IV formulation (58% vs 1%[1]) and is often the reason larger doses of the oral formulation cannot be used.[14]
Rare
[edit]- Fever[1]
- Muscle cramps[1]
- Dry eyes[1]
- Heart block[1]
- Hyperkalemia[1]
- Hepatotoxicity[1]
- Drug eruption similar to lichen planus[15]
- Hypersensitivity – which may result in a lethal respiratory distress[1]
Contraindications
[edit]Labetalol is contraindicated in people with overt cardiac failure, greater-than-first-degree heart block, severe bradycardia, cardiogenic shock, severe hypotension, anyone with a history of obstructive airway disease including asthma, and those with hypersensitivity to the drug.[16]
Pharmacology
[edit]Mechanism of action
[edit]Labetalol is a beta blocker, or an antagonist of the β-adrenergic receptors. It is specifically a non-selective antagonist of the β1- and β2-adrenergic receptors.[17] Labetalol has intrinsic sympathomimetic activity.[17] It is also an antagonist of the α1-adrenergic receptor, and hence is additionally an alpha blocker. The antagonism of the adrenergic receptors by labetalol is competitive against other catecholamines[18] and its actions on the receptors are potent and reversible.[16] Labetalol acts by blocking α- and β-adrenergic receptors, resulting in decreased peripheral vascular resistance without significant alteration of heart rate or cardiac output.
Labetalol is about equipotent in blocking β1- and β2-adrenergic receptors.[19] The amount of α to β blockade depends on whether labetalol is administered orally or intravenously (IV). Orally, the ratio of α to β blockade is 1:3.[20][21] Intravenously, α to β blockade ratio is 1:7.[19][16] Thus, the labetalol can be thought to be a beta blocker with some α-blocking effects.[16][18][22] By comparison, labetalol is a weaker β-adrenergic receptor blocker than propranolol, and has a weaker affinity for α-adrenergic receptors compared to phentolamine.[19][18]
Labetalol's dual α- and β-adrenergic antagonism has different physiological effects in short- and long-term situations. In short-term, acute situations, labetalol decreases blood pressure by decreasing systemic vascular resistance with little effect on stroke volume, heart rate and cardiac output.[23] During long-term use, labetalol can reduce heart rate during exercise while maintaining cardiac output by an increase in stroke volume.[24]
Labetalol possesses significant intrinsic sympathomimetic activity (ISA).[2][22] In particular, it is a partial agonist at β2-adrenergic receptors located in the vascular smooth muscle. Labetalol relaxes vascular smooth muscle by a combination of this partial β2-adrenergic receptor agonism and through α1-adrenergic receptor blockade.[22][25] Overall, this vasodilatory effect can decrease blood pressure.[26] It was originally reported to lack ISA, but a slight degree of activity was subsequently characterized.[2]
Similar to local anesthetics and sodium channel blocking antiarrhythmics, labetalol also has membrane stabilizing activity.[2][22][27] By decreasing sodium entry, labetalol decreases action potential firing and thus has local anesthetic activity.[28]
Physiological action
[edit]The physiological effects of labetalol when administered acutely (intravenously) are not predictable solely by their receptor blocking effect, i.e. blocking β1-adrenergic receptors should decrease heart rate, but labetalol does not. When labetalol is given in acute situations, it decreases the peripheral vascular resistance and systemic blood pressure while having little effect on the heart rate, cardiac output and stroke volume, despite its α1-, β1- and β2-adrenergic receptor blocking mechanism.[23][24] These effects are mainly seen when the person is in the upright position.[26]
Long term labetalol use also has different effects from other beta blockers. Other beta blockers, such as propranolol, persistently reduce cardiac output during exercise. The peripheral vascular resistance decreases when labetalol is first administered. Continuous labetalol use further decreases peripheral vascular resistance. However, during exercise, cardiac output remains the same due to a compensatory mechanism that increases stroke volume. Thus, labetalol is able to reduce heart rate during exercise while maintaining cardiac output by the increase in stroke volume.[24]
Pharmacokinetics
[edit]Distribution
[edit]Labetalol is often classified as a beta blocker with low lipophilicity and hence lower potential for crossing the blood–brain barrier and blood–placenta barrier.[17][29][30] This in turn may result in fewer effects in the central nervous system as well as a lower risk of neuropsychiatric side effects.[17] Paradoxically however, labetalol actually shows high lipophilicity.[31][3][32][33][34][2] In any case, labetalol, in animals including rats, rabbits, and dogs, was found to cross into the brain in negligible amounts, probably for reasons other than low lipophilicity.[1][2][35] On the other hand, the drug has been shown to cross the blood–placenta barrier in humans.[1]
Chemistry
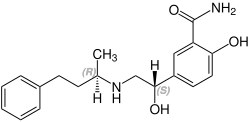
[edit]The minimum requirement for adrenergic agents is a primary or secondary amine separated from a substituted benzene ring by one or two carbons.[36] This configuration results in strong agonist activity. As the size of the substituent attached to the amine becomes greater, particularly with respect to a t-butyl group, then the molecule typically is found to have receptor affinity without intrinsic activity, and is, therefore, an antagonist.[36] Labetalol, with its 1-methyl-3-phenylpropyl substituted amine, is greater in size relative to a t-butyl group and therefore acts predominantly as an antagonist. The overall structure of labetalol is very polar. This was created by substituting the isopropyl group in the standard beta blocker structure with an aralkyl group, including a carboxamide group on the meta position, and by adding a hydroxyl group on the para position.[19]
Labetalol has two chiral carbons and consequently exists as four stereoisomers.[37] Two of these isomers, the (S,S)- and (R,S)- forms are inactive. The third, the (S,R)-isomer, is a powerful α1-adrenergic receptor blocker. The fourth isomer, the (R,R)-isomer which is also known as dilevalol, is a mixed non-selective β-adrenergic receptor blocker and selective α1 blocker.[19] Labetalol is typically given as a racemic mixture to achieve both α- and β-adrenergic receptor blocking activity.[38]
| Stereoisomers of labetalol | |
|---|---|
 (R,R)-Labetalol CAS number: 75659-07-3 |
 (S,S)-Labetalol CAS number: 83167-24-2 |
 (R,S)-Labetalol CAS number: 83167-32-2 |
 (S,R)-Labetalol CAS number: 83167-31-1 |
It is chemically designated in International Union of Pure and Applied Chemistry (IUPAC) nomenclature as 2-hydroxy-5-[1-hydroxy-2-[(1-methyl-3-phenylpropyl)amino]ethyl]benzamide monohydrochloride.[38][39]
The experimental log P of labetalol is 2.7 to 3.1 and its predicted log P ranges from 1.73 to 3.1.[31][3][32][33] Hence, it has relatively high lipophilicity.[31][3][32][33][34]
History
[edit]Labetalol was the first drug created that combined both α- and β-adrenergic receptor blocking properties. It was created to potentially fix the compensatory reflex issue that occurred when blocking a single receptor subtype, i.e. vasoconstriction after blocking β-adrenergic receptors or tachycardia after blocking α-adrenergic receptors. Because the reflex from blocking the single receptor subtypes acted to prevent the lowering of blood pressure, it was postulated that weak blocking of both α- and β-adrenergic receptors could work together to decrease blood pressure.[19][24]
References
[edit]- ^ a b c d e f g h i j k l m n o p q r s t u v w x y "Trandate" (PDF). Prometheus Laboratories Inc. November 2010. Retrieved 3 November 2015.
- ^ a b c d e f g h i j MacCarthy EP, Bloomfield SS (1983). "Labetalol: a review of its pharmacology, pharmacokinetics, clinical uses and adverse effects". Pharmacotherapy. 3 (4): 193–219. doi:10.1002/j.1875-9114.1983.tb03252.x. PMID 6310529.
- ^ a b c d e f g "Labetalol: Uses, Interactions, Mechanism of Action". DrugBank Online. 1 August 1984. Retrieved 1 August 2024.
- ^ a b c d e f "Labetalol Hydrochloride Monograph for Professionals". Drugs.com. American Society of Health-System Pharmacists. Retrieved 3 March 2019.
- ^ a b c d British national formulary : BNF 76 (76 ed.). Pharmaceutical Press. 2018. pp. 147–148. ISBN 9780857113382.
- ^ "Labetalol Use During Pregnancy". Drugs.com. Retrieved 11 March 2019.
- ^ Fischer J, Ganellin CR (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 463. ISBN 9783527607495.
- ^ "The Top 300 of 2021". ClinCalc. Archived from the original on 15 January 2024. Retrieved 14 January 2024.
- ^ "Labetalol - Drug Usage Statistics". ClinCalc. Retrieved 14 January 2024.
- ^ a b Watson K, Watson B, Summers K, Michocki R (2013). "Chapter 21: Hypertensive Crises". In Koda-Kimble MA, Alldredge BK (eds.). Koda-Kimble and Young's Applied Therapeutic: The Clinical Use of Drugs. Philadelphia: Lippincott Williams & Wilkins. pp. 520–535. ISBN 978-1-60913-713-7.
- ^ Arulkumaran N, Lightstone L (December 2013). "Severe pre-eclampsia and hypertensive crises". Best Practice & Research. Clinical Obstetrics & Gynaecology. 27 (6): 877–884. doi:10.1016/j.bpobgyn.2013.07.003. PMID 23962474.
- ^ a b c d Richards JR, Albertson TE, Derlet RW, Lange RA, Olson KR, Horowitz BZ (May 2015). "Treatment of toxicity from amphetamines, related derivatives, and analogues: a systematic clinical review". Drug Alcohol Depend. 150: 1–13. doi:10.1016/j.drugalcdep.2015.01.040. PMID 25724076.
- ^ a b c d Richards JR, Hollander JE, Ramoska EA, Fareed FN, Sand IC, Izquierdo Gómez MM, et al. (May 2017). "β-Blockers, Cocaine, and the Unopposed α-Stimulation Phenomenon". J Cardiovasc Pharmacol Ther. 22 (3): 239–249. doi:10.1177/1074248416681644. PMID 28399647.
- ^ "Labetalol hydrochloride" (PDF). Hospira. May 2015. Archived from the original (PDF) on 4 March 2016. Retrieved 3 November 2015.
- ^ Shiohara T, Kano Y (2007). "Lichen planus and lichenoid dermatoses". In Bolognia JL (ed.). Dermatology. St. Louis: Mosby. p. 161. ISBN 978-1-4160-2999-1.
- ^ a b c d "Labetalol [package insert]. Spring Valley, NY: Par Pharmaceutical; 2011" (PDF). Archived from the original (PDF) on 10 December 2015. Retrieved 3 November 2015.
- ^ a b c d Cojocariu SA, Maștaleru A, Sascău RA, Stătescu C, Mitu F, Leon-Constantin MM (February 2021). "Neuropsychiatric Consequences of Lipophilic Beta-Blockers". Medicina (Kaunas). 57 (2): 155. doi:10.3390/medicina57020155. PMC 7914867. PMID 33572109.
- ^ a b c Robertson D, Biaggioni I (2012). Katzung BG (ed.). Adrenoceptor Antagonist Drugs IN: Basic & Clinical Pharmacology (12th ed.). San Francisco: McGraw Hill Lange Medical. pp. 151–168. ISBN 978-0-07-176401-8.
- ^ a b c d e f Louis W, McNeill JJ, Drummer OH (1988). "Labetalol and other vasodilator/Beta-blocking drugs.". In Doyle AE (ed.). Handbook of Hypertension. Amsterdam, Netherlands: Elsevier Sciences Publishing Co. pp. 246–273. ISBN 978-0-444-90469-0.
- ^ Katzung BF (2006). Basic and clinical pharmacology. New York: McGraw-Hill Medical. p. 170. ISBN 978-0-07-145153-6.
- ^ Richards DA, Tuckman J, Prichard BN (October 1976). "Assessment of alpha- and beta-adrenoceptor blocking actions of labetalol". British Journal of Clinical Pharmacology. 3 (5): 849–855. doi:10.1111/j.1365-2125.1976.tb00637.x. PMC 1428931. PMID 9968.
- ^ a b c d Westfall DP (2004). Craig CR (ed.). Adrenoreceptor Antagonists IN: Modern Pharmacology with Clinical Applications (6th ed.). Baltimore, MD: Lippincott Williams & Wilkins. pp. 109–117. ISBN 978-0781737623.
- ^ a b MacCarthy EP, Bloomfield SS (August 1983). "Labetalol: a review of its pharmacology, pharmacokinetics, clinical uses and adverse effects". Pharmacotherapy. 3 (4): 193–219. doi:10.1002/j.1875-9114.1983.tb03252.x. PMID 6310529. S2CID 20410587.
- ^ a b c d Louis WJ, McNeil JJ, Drummer OH (January 1984). "Pharmacology of combined alpha-beta-blockade. I". Drugs. 28 (Suppl 2): 16–34. doi:10.2165/00003495-198400282-00003. PMID 6151889. S2CID 46974416.
- ^ Lund-Johansen P (1 January 1988). "Hemodynamic effects of beta-blocking compounds possessing vasodilating activity: a review of labetalol, prizidilol, and dilevalol". Journal of Cardiovascular Pharmacology. 11 (Suppl 2): S12–S17. doi:10.1097/00005344-198800000-00004. PMID 2464093.
- ^ a b Lund-Johansen P (1 January 1984). "Pharmacology of combined alpha-beta-blockade. II. Haemodynamic effects of labetalol". Drugs. 28 (Suppl 2): 35–50. doi:10.2165/00003495-198400282-00004. PMID 6151890. S2CID 46986875.
- ^ Mottram AR, Erickson T (2009). Field J (ed.). Toxicology in Emergency Cardiovascular Care IN: The Textbook of Emergency Cardiovascular Care and CPR. Philadelphia, PA: Lippincott Williams & Wilkins. pp. 443–452B. ISBN 978-0-7817-8899-1.
- ^ Narender R, Aggarawal G, Rohilla JK, eds. (1 January 2009). Elsevier Comprehensive Guide to Postgraduate Medical Entrance Examinations (PGMEE). Vol. 2. Elsevier India. pp. 449–. ISBN 978-81-312-1620-0.
- ^ Donnelly R, Macphee GJ (August 1991). "Clinical pharmacokinetics and kinetic-dynamic relationships of dilevalol and labetalol". Clin Pharmacokinet. 21 (2): 95–109. doi:10.2165/00003088-199121020-00002. PMID 1884570.
- ^ Peacock WF, Hilleman DE, Levy PD, Rhoney DH, Varon J (July 2012). "A systematic review of nicardipine vs labetalol for the management of hypertensive crises". Am J Emerg Med. 30 (6): 981–993. doi:10.1016/j.ajem.2011.06.040. PMID 21908132.
- ^ a b c "Labetalol". PubChem. Retrieved 1 August 2024.
- ^ a b c "C19H24N2O3". ChemSpider. 21 July 2022. Retrieved 1 August 2024.
- ^ a b c "Human Metabolome Database: Showing metabocard for Labetalol (HMDB0014736)". Human Metabolome Database. 6 September 2012. Retrieved 1 August 2024.
- ^ a b Woods PB, Robinson ML (March 1981). "An investigation of the comparative liposolubilities of beta-adrenoceptor blocking agents". J Pharm Pharmacol. 33 (3): 172–173. doi:10.1111/j.2042-7158.1981.tb13743.x. PMID 6116760.
- ^ Ganten D, Mulrow PJ (6 December 2012). Pharmacology of Antihypertensive Therapeutics. Springer Science & Business Media. pp. 147–. ISBN 978-3-642-74209-5.
- ^ a b Mehta A (2007). "Adrenergics and Cholinergic their Biosynthesis, Metabolism and Structure Activity Relationships". Medicinal Chemistry of the Peripheral Nervous System. PharmaXChange.info. Archived from the original on 4 November 2010. Retrieved 16 October 2010.
- ^ Riva E, Mennini T, Latini R (December 1991). "The alpha- and beta-adrenoceptor blocking activities of labetalol and its RR-SR (50:50) stereoisomers". British Journal of Pharmacology. 104 (4): 823–828. doi:10.1111/j.1476-5381.1991.tb12513.x. PMC 1908821. PMID 1687367.
- ^ a b Robertson D, Biaggioni, I. Adrenoceptor Antagonist Drugs. In: Katzung BG, Masters SB, Trevor AJ, eds. Basic & Clinical Pharmacology. 12th ed. San Francisco, CA: McGraw Hill Lange Medical; 2012: 151–168. ISBN 978-0-07-176401-8.
- ^ "labetalol | C19H24N2O3". PubChem. U.S. National Library of Medicine. Retrieved 4 November 2015.
