Clonidine
Clonidine, sold under the brand name Catapres among others, is an α2A-adrenergic receptor agonist[12] medication used to treat high blood pressure, ADHD, drug withdrawal (e.g., alcohol, opioids, or nicotine), menopausal flushing, diarrhea, spasticity, and certain pain conditions.[13] The drug is often prescribed off-label for tics. It is used orally (by mouth), by injection, or as a transdermal skin patch.[13] Onset of action is typically within an hour with the effects on blood pressure lasting for up to eight hours.[13]
Common side effects include dry mouth, dizziness, headaches, hypotension, and sleepiness.[13] Severe side effects may include hallucinations, heart arrhythmias, and confusion.[14] If rapidly stopped, withdrawal effects may occur, such as a dangerous rise in blood pressure.[13] Use during pregnancy or breastfeeding is not recommended.[14] Clonidine lowers blood pressure by stimulating α2-adrenergic receptors in the brain, which results in relaxation of many arteries.[13]
Clonidine was patented in 1961 and came into medical use in 1966.[15][16][17] It is available as a generic medication.[13] In 2022, it was the 71st most commonly prescribed medication in the United States, with more than 9 million prescriptions.[18][19]
Medical uses
[edit]
Clonidine is used to treat high blood pressure, attention deficit hyperactivity disorder (ADHD), drug withdrawal (alcohol, opioids, or nicotine), menopausal flushing, diarrhea, and certain pain conditions. It also sees some use off-label for episodic insomnia, restless legs syndrome, and anxiety, among other uses.[13]
Resistant hypertension
[edit]Clonidine may be effective for lowering blood pressure in people with resistant hypertension.[20]
Clonidine works by slowing the pulse rate and exerts a reduction of serum concentrations of renin, aldosterone, and catecholamines.[21]
Attention deficit hyperactivity disorder
[edit]Clonidine may improve symptoms of attention deficit hyperactivity disorder in some people but causes many adverse effects and the beneficial effect is modest.[22] In Australia, clonidine is an accepted but not approved use for ADHD by the TGA.[23] Clonidine, along with methylphenidate, has been studied for treatment of ADHD.[24][25][26] While not as effective as methylphenidate in treating ADHD, clonidine does offer some benefit;[24] it can also be useful in combination with stimulant medications.[27] Some studies show clonidine to be more sedating than guanfacine, which may be better at bedtime along with an arousing stimulant in the morning.[28][29] Clonidine has been used to reduce sleep disturbances in ADHD, including to help offset stimulant-associated insomnia.[30][31][32][33] Unlike stimulant medications, clonidine is regarded as having no abuse potential, and may even be used to reduce abuse of drugs including nicotine and cocaine.[34]
In the US, only the extended-release form of clonidine is approved for ADHD treatment.[35]
Drug withdrawal
[edit]Clonidine may be used to ease drug withdrawal symptoms associated with abruptly stopping the long-term use of opioids, alcohol, benzodiazepines, and nicotine.[36] It can alleviate opioid withdrawal symptoms by reducing the sympathetic nervous system response such as tachycardia and hypertension, hyperhidrosis (excessive sweating), hot and cold flashes, and akathisia.[37] It may also be helpful in aiding smokers to quit.[38] The sedation effect can also be useful. Clonidine may also reduce severity of neonatal abstinence syndrome in infants born to mothers that are using certain drugs, particularly opioids.[39] In infants with neonatal withdrawal syndrome, clonidine may improve the neonatal intensive care unit Network Neurobehavioral Score.[40]
Clonidine has also been suggested as a treatment for rare instances of dexmedetomidine withdrawal.[41]
Spasticity
[edit]Clonidine has some role in the treatment of spasticity, acting principally by inhibiting excessive sensory transmission below the level of injury[clarify]. Its use, however, is mainly as a second or third line agent, due to side effects such as hypotension, bradycardia, and drowsiness.[42] Clonidine can be administered intrathecally,[43] which confers various benefits, including a reduction or prevention of the blood pressure lowering effects and increased effectiveness against spasticity.[44] The effectiveness of intrathecal clonidine is comparable to that of intrathecal baclofen for spasticity.[44]
Clonidine suppression test
[edit]The reduction in circulating norepinephrine by clonidine was used in the past as an investigatory test for phaeochromocytoma, which is a catecholamine-synthesizing tumor, usually found in the adrenal medulla.[45] In a clonidine suppression test, plasma catecholamine levels are measured before and 3 hours after a 0.3 mg oral test dose has been given to the patient. A positive test occurs if there is no decrease in plasma levels.[45]
Other uses
[edit]Clonidine also has several off-label uses, and has been prescribed to treat psychiatric disorders including stress, hyperarousal caused by post-traumatic stress disorder, borderline personality disorder, and other anxiety disorders.[46][47][48][49][50][51][52][53] Clonidine is also a mild sedative, and can be used as premedication before surgery or procedures.[54] It has also been studied as a way to calm acute manic episodes.[55] Its epidural use for pain during heart attack, and postoperative and intractable pain has also been studied extensively.[56] Clonidine can be used in restless legs syndrome.[57] It can also be used to treat facial flushing and redness associated with rosacea.[58] It has also been successfully used topically in a clinical trial as a treatment for diabetic neuropathy.[59] Clonidine can also be used for migraine headaches and hot flashes associated with menopause.[60][61] Clonidine has also been used to treat refractory diarrhea associated with irritable bowel syndrome, fecal incontinence, diabetes, diarrhea associated with opioid withdrawal, intestinal failure, neuroendocrine tumors, and cholera.[62] Clonidine can be used in the treatment of Tourette syndrome (specifically for tics).[63] Clonidine has also had some success in clinical trials for helping to remove or ameliorate the symptoms of hallucinogen persisting perception disorder (HPPD).[64]
Injection of α2-adrenergic receptor agonists into the knee joint space, including clonidine, may reduce the severity of knee pain after arthroscopic knee surgery.[65]
Light-activated derivatives of clonidine (adrenoswitches) have been developed for research purposes and shown to control pupillary reflex with light in blind mice by topical application.[66]
Pregnancy and breastfeeding
[edit]It is classified by the TGA of Australia as pregnancy category B3, which means that it has shown some detrimental effects on fetal development in animal studies, although the relevance of this to human beings is unknown.[67] Clonidine appears in high concentration in breast milk; a nursing infant's serum clonidine concentration is approximately 2/3 of the mother's.[68] Caution is warranted in women who are pregnant, planning to become pregnant, or are breastfeeding.[69]
Adverse effects
[edit]The principal adverse effects of clonidine are sedation, dry mouth, and hypotension (low blood pressure).[7]
Very common (>10% frequency):
- Dizziness
- Orthostatic hypotension
- Somnolence (dose-dependent)
- Dry mouth
- Headache (dose-dependent)
- Fatigue
- Skin reactions (if given transdermally)
- Hypotension
Common (1–10% frequency):
- Anxiety
- Constipation
- Sedation (dose-dependent)
- Nausea/vomiting
- Malaise
- Abnormal LFTs
- Rash
- Weight gain/loss
- Pain below the ear (from salivary gland)
- Erectile dysfunction
Uncommon (0.1–1% frequency):
- Delusional perception
- Hallucination
- Nightmare
- Paresthesia
- Sinus bradycardia
- Raynaud's phenomenon
- Pruritus
- Urticaria
Rare (<0.1% frequency):
- Gynaecomastia
- Impaired ability to cry
- Atrioventricular block
- Nasal dryness
- Colonic pseudo-obstruction
- Alopecia
- Hyperglycemia
Withdrawal
[edit]Because clonidine suppresses sympathetic outflow, resulting in lower blood pressure, sudden discontinuation can result in acute hypertension due to a rebound in sympathetic outflow. In extreme cases, this can result in a hypertensive crisis, which is a medical emergency.[71]
Clonidine therapy should generally be gradually tapered when discontinuing therapy to avoid rebound effects from occurring. Treatment of clonidine withdrawal hypertension depends on the severity of the condition. Reintroduction of clonidine for mild cases, alpha and beta blockers for more urgent situations. Beta blockers should never be used alone to treat clonidine withdrawal as alpha vasoconstriction would still continue.[72][73]
Pharmacology
[edit]| Site | Ki (nM) | Species | Ref |
|---|---|---|---|
| NET | >1,000 | Human | [75] |
| 5-HT1B | >10,000 | Rat | [76] |
| 5-HT2A | >10,000 | Human | [74] |
| α1A | 316.23 | Human | [75] |
| α1B | 316.23 | Human | [75] |
| α1D | 125.89 | Human | [75] |
| α2A | 35.48 – 61.65 | Human | [75][77] |
| α2B | 69.18 – 309.0 | Human | [77][75] |
| α2C | 134.89 – 501.2 | Human | [77][75] |
| D1 | > 10,000 | Rat | [78] |
| I1 | 31.62 | Bovine | [75] |
| I2 (cortex) | >1,000 | Rat | [75] |
| MAO-A | >1,000 | Rat | [75] |
| MAO-B | >1,000 | Rat | [75] |
| σ | >10,000 | Guinea Pig | [79] |
| The Ki refers to a drug's affinity for a receptor. The smaller the Ki, the higher the affinity for that receptor.[80] Reported imidazoline-2 binding is measured in the cortex — I2 receptor bindings measured in stomach membranes are much lower.[81] | |||
Mechanism of action
[edit]Clonidine crosses the blood–brain barrier.[9]
High blood pressure
[edit]Clonidine treats high blood pressure by stimulating α2 receptors in the brainstem, which decreases peripheral vascular resistance, lowering blood pressure. It has specificity towards the presynaptic α2 receptors in the vasomotor center in the brainstem. This binding has a sympatholytic effect, suppresses release of norepinephrine, ATP, renin, and neuropeptide Y which if released would increase vascular resistance.[12]: 201–203
Clonidine also acts as an agonist at imidazoline-1 (I1) receptors in the brain, and it is hypothesized that this effect may contribute to reducing blood pressure by reducing signaling in the sympathetic nervous system; this effect acts upstream of the central α2 agonist effect of clonidine.[12]: 201–203 [82]
Clonidine may also cause bradycardia, theoretically by increasing signaling through the vagus nerve. When given intravenously, clonidine can temporarily increase blood pressure by stimulating α1 receptors in smooth muscles in blood vessels.[83] This hypertensive effect is not usual when clonidine is given orally or by the transdermal route.[12]: 201–203
Plasma concentration of clonidine exceeding 2.0 ng/mL does not provide further blood pressure reduction.[84]
Attention deficit hyperactivity disorder
[edit]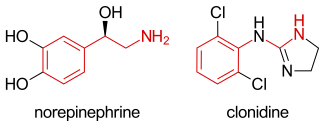
In the setting of attention deficit hyperactivity disorder (ADHD), clonidine's molecular mechanism of action occurs due to its agonism at the α2A adrenergic receptor, the subtype of the adrenergic receptor that is most principally found in the brain. Within the brain, the α2A adrenergic receptors are found within the prefrontal cortex (PFC), among other areas. The α2A adrenergic receptors are found on the presynaptic cleft of a given neuron, and, when activated by an agonist, the effect on downstream neurons is inhibitory. The inhibition is accomplished by preventing the secretion of the neurotransmitter norepinephrine. Thus, clonidine's agonism on α2A adrenergic receptors in the PFC inhibits the action of downstream neurons by preventing the secretion of norepinephrine.[85]
This mechanism is similar to the brain's physiological inhibition of PFC neurons by the locus ceruleus (LC), which secretes norepinephrine into the PFC. Although norepinephrine can also bind to target adrenergic receptors on the downstream neuron (otherwise inducing a stimulatory effect), norepinephrine also binds to α2A adrenergic receptors (akin to clonidine's mechanism of action), inhibiting the release of norepinephrine by that neuron and inducing an inhibitory effect. Because the PFC is required for working memory and attention, it is thought that clonidine's inhibition of PFC neurons helps to eliminate irrelevant attention (and subsequent behaviors), improving the person's focus and correcting deficits in attention.[85]
Growth hormone test
[edit]Clonidine stimulates release of GHRH hormone from the hypothalamus, which in turn stimulates pituitary release of growth hormone.[86] This effect has been used as part of a "growth hormone test," which can assist with diagnosing growth hormone deficiency in children.[87]
Pharmacokinetics
[edit]After being ingested, clonidine is absorbed into the blood stream rapidly with an overall bioavailability around 70–80%.[4] Peak concentrations in human plasma occur within 60–90 minutes for the "immediate release" (IR) version of the drug, which is shorter than the "extended release" (ER/XR) version.[88] Clonidine is fairly lipid soluble with the logarithm of its partition coefficient (log P) equal to 1.6;[89][88] to compare, the optimal log P to allow a drug that is active in the human central nervous system to penetrate the blood brain barrier is 2.0.[90] Less than half of the absorbed portion of an orally administered dose will be metabolized by the liver into inactive metabolites, with roughly the other half being excreted unchanged by the kidneys.[88] About one-fifth of an oral dose will not be absorbed, and is thus excreted in the feces.[88] Work with liver microsomes shows in the liver clonidine is primarily metabolized by CYP2D6 (66%), CYP1A2 (10–20%), and CYP3A (0–20%) with negligible contributions from the less abundant enzymes CYP3A5, CYP1A1, and CYP3A4.[11] 4-hydroxyclonidine, the main metabolite of clonidine, is also an α2A agonist but is non lipophilic and is not believed to contribute to the effects of clonidine since it does not cross the blood–brain barrier.[91][92]
Measurements of the half-life of clonidine vary widely, between 6 and 23 hours, with the half-life being greatly affected by and prolonged in the setting of poor kidney function.[88] Variations in half-life may be partially attributable to CYP2D6 genetics.[11] Some research has suggested the half-life of clonidine is dose dependent and approximately doubles upon chronic dosing,[93] while other work contradicts this.[6] Following a 0.3 mg oral dose, a small study of five patients by Dollery et al. (1976) found half-lives ranging between 6.3 and 23.4 hours (mean 12.7).[94] A similar N=5 study by Davies et al. (1977) found a narrower range of half-lives, between 6.7 and 13 hours (mean 8.6),[4] while an N=8 study by Keraäen et al. that included younger patients found a somewhat shorter mean half-life of 7.5 hours.[95]
History
[edit]Clonidine was introduced in 1966.[96] It was first used as a hypertension treatment under the trade name of Catapres.[97]
Society and culture
[edit]Brand names
[edit]As of June 2017, clonidine is marketed under many brand names worldwide: Arkamin, Aruclonin, Atensina, Catapin, Catapres, Catapresan, Catapressan, Chianda, Chlofazoline, Chlophazolin, Clonid-Ophtal, Clonidin, Clonidina, Clonidinã, Clonidine, Clonidine hydrochloride, Clonidinhydrochlorid, Clonidini, Clonidinum, Clonigen, Clonistada, Clonnirit, Clophelinum, Dixarit, Duraclon, Edolglau, Haemiton, Hypodine, Hypolax, Iporel, Isoglaucon, Jenloga, Kapvay, Klofelino, Kochaniin, Lonid, Melzin, Menograine, Normopresan, Paracefan, Pinsanidine, Run Rui, and Winpress.[98] It is marketed as a combination drug with chlortalidone as Arkamin-H, Bemplas, Catapres-DIU, and Clorpres, and in combination with bendroflumethiazide as Pertenso.[98]
References
[edit]- ^ "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved 22 October 2023.
- ^ "Catapres-TTS-1- clonidine transdermal system patch; Catapres-TTS-2- clonidine transdermal system patch; Catapres-TTS-3- clonidine transdermal system patch". DailyMed. 25 March 2023. Retrieved 5 September 2024.
- ^ "Onyda XR- clonidine hydrochloride suspension, extended release". DailyMed. 7 June 2024. Retrieved 5 September 2024.
- ^ a b c Davies DS, Wing AM, Reid JL, Neill DM, Tippett P, Dollery CT (May 1977). "Pharmacokinetics and concentration-effect relationships of intervenous and oral clonidine". Clinical Pharmacology and Therapeutics. 21 (5): 593–601. doi:10.1002/cpt1977215593. PMID 870272. S2CID 5566079.
- ^ "Catapres- clonidine hydrochloride tablet". DailyMed. 6 September 2016. Archived from the original on 4 August 2020. Retrieved 21 December 2019.
The pharmacokinetics of clonidine is dose-proportional in the range of 100 to 600 µg.The absolute bioavailability of clonidine on oral administration is 70% to 80%. Peak plasma clonidine levels are attained in approximately 1 to 3 hours.
- ^ a b c Lowenthal DT, Matzek KM, MacGregor TR (May 1988). "Clinical pharmacokinetics of clonidine". Clinical Pharmacokinetics. 14 (5): 287–310. doi:10.2165/00003088-198814050-00002. PMID 3293868. S2CID 24783447.
- ^ a b c d "clonidine (Rx) - Catapres, Catapres-TTS, more." Medscape Reference. WebMD. Archived from the original on 4 December 2020. Retrieved 10 November 2013.
- ^ "Catapres- clonidine hydrochloride tablet". DailyMed. 6 September 2016. Archived from the original on 4 August 2020. Retrieved 21 December 2019.
Catapres tablets act relatively rapidly. The patient's blood pressure declines within 30 to 60 minutes after an oral dose, the maximum decrease occurring within 2 to 4 hours.
- ^ a b "Catapres- clonidine hydrochloride tablet". DailyMed. 6 September 2016. Archived from the original on 4 August 2020. Retrieved 21 December 2019.
Following intravenous administration, clonidine displays biphasic disposition with a distribution half-life of about 20 minutes and an elimination half-life ranging from 12 to 16 hours. The half-life increases up to 41 hours in patients with severe impairment of renal function. Clonidine crosses the placental barrier. It has been shown to cross the blood–brain barrier in rats.
- ^ "Kapvay". RxList. Archived from the original on 12 October 2017. Retrieved 30 October 2014.
- ^ a b c Claessens AJ, Risler LJ, Eyal S, Shen DD, Easterling TR, Hebert MF (September 2010). "CYP2D6 mediates 4-hydroxylation of clonidine in vitro: implication for pregnancy-induced changes in clonidine clearance". Drug Metabolism and Disposition. 38 (9): 1393–1396. doi:10.1124/dmd.110.033878. PMC 2939473. PMID 20570945.
- ^ a b c d Westfall TC, Macarthur H, Westfall DP (2017). "Chapter 12:Adrenergic Agonists and Antagonists". In Brunton L, Knollmann B, Hilal-Dandan R (eds.). Goodman and Gilman's The Pharmacological Basis of Therapeutics (13th ed.). McGraw-Hill Education / Medical. ISBN 9781259584732.
- ^ a b c d e f g h "Clonidine Monograph for Professionals". Drugs.com. American Society of Health-System Pharmacists. Archived from the original on 3 February 2019. Retrieved 2 February 2019.
- ^ a b British national formulary : BNF 76 (76 ed.). Pharmaceutical Press. 2018. p. 144. ISBN 9780857113382.
- ^ Neil MJ (November 2011). "Clonidine: clinical pharmacology and therapeutic use in pain management". Current Clinical Pharmacology. 6 (4): 280–287. doi:10.2174/157488411798375886. PMID 21827389. S2CID 40756251.
- ^ Stähle H (June 2000). "A historical perspective: development of clonidine". Best Practice & Research Clinical Anaesthesiology. 14 (2): 237–246. doi:10.1053/bean.2000.0079.
- ^ Fischer J, Ganellin CR (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 550. ISBN 9783527607495. Archived from the original on 29 April 2023. Retrieved 12 September 2020.
- ^ "The Top 300 of 2022". ClinCalc. Archived from the original on 30 August 2024. Retrieved 30 August 2024.
- ^ "Clonidine Drug Usage Statistics, United States, 2013 - 2022". ClinCalc. Retrieved 30 August 2024.
- ^ Viera AJ (June 2018). "Hypertension Update: Resistant Hypertension". FP Essent. 469: 20–25. PMID 29863319.
- ^ "Catapres- clonidine hydrochloride tablet". DailyMed. 6 September 2016. Archived from the original on 4 August 2020. Retrieved 21 December 2019.
Slowing of the pulse rate has been observed in most patients given clonidine, but the drug does not alter normal hemodynamic response to exercise. Other studies in patients have provided evidence of a reduction in plasma renin activity and in the excretion of aldosterone and catecholamines.
- ^ Connor DF, Fletcher KE, Swanson JM (December 1999). "A meta-analysis of clonidine for symptoms of attention-deficit hyperactivity disorder". Journal of the American Academy of Child and Adolescent Psychiatry. 38 (12): 1551–1559. doi:10.1097/00004583-199912000-00017. PMID 10596256.
- ^ Rossi, S, ed. (2013). Australian Medicines Handbook (2013 ed.). Adelaide: The Australian Medicines Handbook Unit Trust. ISBN 978-0-9805790-9-3.
- ^ a b Palumbo DR, Sallee FR, Pelham WE, Bukstein OG, Daviss WB, McDERMOTT MP (February 2008). "Clonidine for attention-deficit/hyperactivity disorder: I. Efficacy and tolerability outcomes". Journal of the American Academy of Child and Adolescent Psychiatry. 47 (2): 180–188. doi:10.1097/chi.0b013e31815d9af7. PMID 18182963.
- ^ Daviss WB, Patel NC, Robb AS, McDERMOTT MP, Bukstein OG, Pelham WE, et al. (February 2008). "Clonidine for attention-deficit/hyperactivity disorder: II. ECG changes and adverse events analysis". Journal of the American Academy of Child and Adolescent Psychiatry. 47 (2): 189–198. doi:10.1097/chi.0b013e31815d9ae4. PMID 18182964.
- ^ Kornfield R, Watson S, Higashi AS, Conti RM, Dusetzina SB, Garfield CF, et al. (April 2013). "Effects of FDA advisories on the pharmacologic treatment of ADHD, 2004-2008". Psychiatric Services. 64 (4): 339–346. doi:10.1176/appi.ps.201200147. PMC 4023684. PMID 23318985.
- ^ Kollins SH, Jain R, Brams M, Segal S, Findling RL, Wigal SB, et al. (June 2011). "Clonidine extended-release tablets as add-on therapy to psychostimulants in children and adolescents with ADHD". Pediatrics. 127 (6): e1406–e1413. doi:10.1542/peds.2010-1260. PMC 3387872. PMID 21555501.
- ^ Jäkälä P, Riekkinen M, Sirviö J, Koivisto E, Kejonen K, Vanhanen M, et al. (May 1999). "Guanfacine, but not clonidine, improves planning and working memory performance in humans". Neuropsychopharmacology. 20 (5): 460–470. doi:10.1016/S0893-133X(98)00127-4. PMID 10192826.
- ^ Freeland K, Turner A, Gormley L (2014). "Clonidine and Guanfacine IR vs ER: Old Drugs With "New" Formulations". Mental Health Clinician. 4: 22–26. doi:10.9740/mhc.n186955. Archived from the original on 9 August 2014. Retrieved 1 August 2014.
- ^ Nguyen M, Tharani S, Rahmani M, Shapiro M (March 2014). "A review of the use of clonidine as a sleep aid in the child and adolescent population". Clinical Pediatrics. 53 (3): 211–216. doi:10.1177/0009922813502123. PMID 24027233. S2CID 742140.
- ^ Hoban TF (March 2004). "Assessment and treatment of disturbed sleep in attention deficit hyperactivity disorder". Expert Review of Neurotherapeutics. 4 (2): 307–316. doi:10.1586/14737175.4.2.307. PMID 15853572. S2CID 35000868.
- ^ Schachar R, Ickowicz A (1999). "Pharmacological Treatment of Attention-Deficit/HyperactivityDisorder". Handbook of Disruptive Behavior Disorders. Springer US. pp. 221–254. doi:10.1007/978-1-4615-4881-2_10. ISBN 978-1-4613-7214-1.
- ^ Wilens TE, Biederman J, Spencer T (1994). "Clonidine for sleep disturbances associated with attention-deficit hyperactivity disorder". Journal of the American Academy of Child and Adolescent Psychiatry. 33 (3): 424–426. doi:10.1097/00004583-199403000-00018. PMID 8169189.
- ^ Clemow DB, Walker DJ (September 2014). "The potential for misuse and abuse of medications in ADHD: a review". Postgraduate Medicine. 126 (5): 64–81. doi:10.3810/pgm.2014.09.2801. PMID 25295651. S2CID 207580823.
- ^ "Highlights of Prescribing Information: Kapvay" (PDF). US FDA. Retrieved 31 March 2024.
- ^ Fitzgerald PJ (October 2013). "Elevated Norepinephrine may be a Unifying Etiological Factor in the Abuse of a Broad Range of Substances: Alcohol, Nicotine, Marijuana, Heroin, Cocaine, and Caffeine". Substance Abuse. 7: 171–183. doi:10.4137/SART.S13019. PMC 3798293. PMID 24151426.
- ^ Giannini AJ (1997). Drugs of Abuse (2nd ed.). Los Angeles: Practice Management Information.
- ^ Gourlay SG, Stead LF, Benowitz NL (2004). "Clonidine for smoking cessation". The Cochrane Database of Systematic Reviews. 2008 (3): CD000058. doi:10.1002/14651858.CD000058.pub2. PMC 7038651. PMID 15266422.
- ^ Streetz VN, Gildon BL, Thompson DF (April 2016). "Role of Clonidine in Neonatal Abstinence Syndrome: A Systematic Review". The Annals of Pharmacotherapy. 50 (4): 301–310. doi:10.1177/1060028015626438. PMID 26783353. S2CID 40652097.
- ^ Disher T, Gullickson C, Singh B, Cameron C, Boulos L, Beaubien L, et al. (March 2019). "Pharmacological Treatments for Neonatal Abstinence Syndrome: A Systematic Review and Network Meta-analysis". JAMA Pediatrics. 173 (3): 234–243. doi:10.1001/jamapediatrics.2018.5044. PMC 6439896. PMID 30667476.
- ^ Kukoyi A, Coker S, Lewis L, Nierenberg D (January 2013). "Two cases of acute dexmedetomidine withdrawal syndrome following prolonged infusion in the intensive care unit: Report of cases and review of the literature". Human & Experimental Toxicology. 32 (1): 107–110. doi:10.1177/0960327112454896. PMID 23111887. S2CID 31570614.
- ^ Chang E, Ghosh N, Yanni D, Lee S, Alexandru D, Mozaffar T (2013). "A Review of Spasticity Treatments: Pharmacological and Interventional Approaches". Critical Reviews in Physical and Rehabilitation Medicine. 25 (1–2): 11–22. doi:10.1615/CritRevPhysRehabilMed.2013007945. PMC 4349402. PMID 25750484.
- ^ Smith HS, Deer TR, Staats PS, Singh V, Sehgal N, Cordner H (March 2008). "Intrathecal drug delivery". Pain Physician. 11 (2 Suppl): S89–S104. doi:10.36076/ppj.2008/11/S89. PMID 18443642.
- ^ a b Rémy-Néris O, Denys P, Bussel B (November 2001). "Intrathecal clonidine for controlling spastic hypertonia". Physical Medicine and Rehabilitation Clinics of North America. 12 (4): 939–51, ix. doi:10.1016/S1047-9651(18)30040-8. PMID 11723871.
- ^ a b Eisenhofer G, Goldstein DS, Walther MM, Friberg P, Lenders JW, Keiser HR, et al. (June 2003). "Biochemical diagnosis of pheochromocytoma: how to distinguish true- from false-positive test results". The Journal of Clinical Endocrinology and Metabolism. 88 (6): 2656–2666. doi:10.1210/jc.2002-030005. PMID 12788870.
- ^ van der Kolk BA (September–October 1987). "The drug treatment of post-traumatic stress disorder". Journal of Affective Disorders. 13 (2): 203–213. doi:10.1016/0165-0327(87)90024-3. PMID 2960712.
- ^ Sutherland SM, Davidson JR (June 1994). "Pharmacotherapy for post-traumatic stress disorder". The Psychiatric Clinics of North America. 17 (2): 409–423. doi:10.1016/S0193-953X(18)30122-9. PMID 7937367.
- ^ Southwick SM, Bremner JD, Rasmusson A, Morgan CA, Arnsten A, Charney DS (November 1999). "Role of norepinephrine in the pathophysiology and treatment of posttraumatic stress disorder". Biological Psychiatry. 46 (9): 1192–1204. doi:10.1016/S0006-3223(99)00219-X. PMID 10560025. S2CID 32148292.
- ^ Strawn JR, Geracioti TD (2008). "Noradrenergic dysfunction and the psychopharmacology of posttraumatic stress disorder". Depression and Anxiety. 25 (3): 260–271. doi:10.1002/da.20292. PMID 17354267. S2CID 33940152.
- ^ Boehnlein JK, Kinzie JD (March 2007). "Pharmacologic reduction of CNS noradrenergic activity in PTSD: the case for clonidine and prazosin". Journal of Psychiatric Practice. 13 (2): 72–78. doi:10.1097/01.pra.0000265763.79753.c1. PMID 17414682. S2CID 1607064.
- ^ Huffman JC, Stern TA (2007). "Neuropsychiatric consequences of cardiovascular medications". Dialogues in Clinical Neuroscience. 9 (1): 29–45. doi:10.31887/DCNS.2007.9.1/jchuffman. PMC 3181843. PMID 17506224.
- ^ Najjar F, Weller RA, Weisbrot J, Weller EB (April 2008). "Post-traumatic stress disorder and its treatment in children and adolescents". Current Psychiatry Reports. 10 (2): 104–108. doi:10.1007/s11920-008-0019-0. PMID 18474199. S2CID 23494905.
- ^ Ziegenhorn AA, Roepke S, Schommer NC, Merkl A, Danker-Hopfe H, Perschel FH, et al. (April 2009). "Clonidine improves hyperarousal in borderline personality disorder with or without comorbid posttraumatic stress disorder: a randomized, double-blind, placebo-controlled trial". Journal of Clinical Psychopharmacology. 29 (2): 170–173. doi:10.1097/JCP.0b013e31819a4bae. PMID 19512980. S2CID 31292297.
- ^ Fazi L, Jantzen EC, Rose JB, Kurth CD, Watcha MF (January 2001). "A comparison of oral clonidine and oral midazolam as preanesthetic medications in the pediatric tonsillectomy patient". Anesthesia and Analgesia. 92 (1): 56–61. doi:10.1097/00000539-200101000-00011. PMID 11133600. S2CID 18885497.
- ^ Giannini AJ, Extein I, Gold MS, Pottash AL, Castellani S (1983). "Clonidine in mania". Drug Development Research. 3 (1): 101–105. doi:10.1002/ddr.430030112. S2CID 85093127.
- ^ Patel SS, Dunn CJ, Bryson HM (1996). "Epidural clonidine: a review of its pharmacology and efficacy in the management of pain during labour and postoperative and intractable pain". CNS Drugs. 6 (6): 474–497. doi:10.2165/00023210-199606060-00007. S2CID 72544106.
- ^ "Treatment and Management of RLS". www.medscape.org. WebMD LLC. Archived from the original on 29 September 2017. Retrieved 3 October 2018.
- ^ Blount BW, Pelletier AL (August 2002). "Rosacea: a common, yet commonly overlooked, condition". American Family Physician. 66 (3): 435–440. PMID 12182520. Archived from the original on 26 July 2011. Retrieved 12 February 2012.
- ^ Campbell CM, Kipnes MS, Stouch BC, Brady KL, Kelly M, Schmidt WK, et al. (September 2012). "Randomized control trial of topical clonidine for treatment of painful diabetic neuropathy". Pain. 153 (9): 1815–1823. doi:10.1016/j.pain.2012.04.014. PMC 3413770. PMID 22683276.
- ^ "Clonidine Oral Uses". WebMD. Archived from the original on 25 October 2007. Retrieved 30 May 2007.
- ^ "Clonidine". Drugs.com. Archived from the original on 14 April 2017. Retrieved 25 May 2017.
- ^ Fragkos KC, Zárate-Lopez N, Frangos CC (May 2016). "What about clonidine for diarrhoea? A systematic review and meta-analysis of its effect in humans". Therapeutic Advances in Gastroenterology. 9 (3): 282–301. doi:10.1177/1756283X15625586. PMC 4830099. PMID 27134659.
- ^ Egolf A, Coffey BJ (February 2014). "Current pharmacotherapeutic approaches for the treatment of Tourette syndrome". Drugs of Today. 50 (2): 159–179. doi:10.1358/dot.2014.50.2.2097801. PMID 24619591.
- ^ Martinotti G, Santacroce R, Pettorruso M, Montemitro C, Spano MC, Lorusso M, et al. (March 2018). "Hallucinogen Persisting Perception Disorder: Etiology, Clinical Features, and Therapeutic Perspectives". Brain Sciences. 8 (3): 47. doi:10.3390/brainsci8030047. PMC 5870365. PMID 29547576.
- ^ Ryan TJ, Holyoak R, Vlok R, Melhuish T, Hodge A, Binks M, et al. (February 2019). "Intra-articular Alpha-2 Agonists as an Adjunct to Local Anesthetic in Knee Arthroscopy: A Systematic Review and Meta-Analysis". J Knee Surg. 32 (2): 138–145. doi:10.1055/s-0038-1636909. PMID 29534270. S2CID 3861878.
- ^ Prischich D, Gomila AM, Milla-Navarro S, Sangüesa G, Diez-Alarcia R, Preda B, et al. (February 2021). "Adrenergic Modulation With Photochromic Ligands". Angewandte Chemie. 60 (7). Wiley: 3625–3631. doi:10.1002/anie.202010553. hdl:2434/778579. PMID 33103317.
- ^ a b "Catapres 150 Tablets Catapres Ampoules" (PDF). TGA eBusiness Services. Boehringer Ingelheim Pty Limited. 28 February 2013. Archived from the original on 16 January 2017. Retrieved 27 November 2013.
- ^ "Clonidine". Drugs and Lactation Database (LactMed). National Library of Medicine (US). 2006. PMID 30000689. Archived from the original on 5 December 2020. Retrieved 5 January 2019.
- ^ "Clonidine". Prescription Marketed Drugs. www.drugsdb.eu. Archived from the original on 28 March 2012. Retrieved 2 August 2011.
- ^ "Clonidine 25 mcg Tablets BP - Summary of Product Characteristics (SPC)". electronic Medicines Compendium. Sandoz Limited. 2 August 2012. Archived from the original on 2 December 2013. Retrieved 27 November 2013.
- ^ Brayfield, A, ed. (13 January 2014). "Clonidine". Martindale: The Complete Drug Reference. London, UK: Pharmaceutical Press. Archived from the original on 28 August 2021. Retrieved 28 June 2014.
- ^ Parker K, Brunton L, Goodman LS, Lazo JS, Gilman A (2006). Goodman & Gilman's - the pharmacological basis of therapeutics. New York: McGraw-Hill. pp. 854–855. ISBN 978-0-07-142280-2.
- ^ Vitiello B (2008). "Understanding the Risk of Using Medications for ADHD with Respect to Physical Growth and Cardiovascular Function". Child Adolesc Psychiatr Clin N Am. 17 (2): 459–474, xi. doi:10.1016/j.chc.2007.11.010. PMC 2408826. PMID 18295156.
- ^ a b Roth BL, Driscol J. "PDSP Ki Database". Psychoactive Drug Screening Program (PDSP). University of North Carolina at Chapel Hill and the United States National Institute of Mental Health. Archived from the original on 14 November 2022. Retrieved 14 August 2017.
- ^ a b c d e f g h i j k Millan MJ, Dekeyne A, Newman-Tancredi A, Cussac D, Audinot V, Milligan G, et al. (December 2000). "S18616, a highly potent, spiroimidazoline agonist at alpha(2)-adrenoceptors: I. Receptor profile, antinociceptive and hypothermic actions in comparison with dexmedetomidine and clonidine". The Journal of Pharmacology and Experimental Therapeutics. 295 (3): 1192–1205. PMID 11082457.
- ^ Matsumoto I, Combs MR, Jones DJ (February 1992). "Characterization of 5-hydroxytryptamine1B receptors in rat spinal cord via [125I]iodocyanopindolol binding and inhibition of [3H]-5-hydroxytryptamine release". The Journal of Pharmacology and Experimental Therapeutics. 260 (2): 614–626. PMID 1738111.
- ^ a b c Jasper JR, Lesnick JD, Chang LK, Yamanishi SS, Chang TK, Hsu SA, et al. (April 1998). "Ligand efficacy and potency at recombinant alpha2 adrenergic receptors: agonist-mediated [35S]GTPgammaS binding". Biochemical Pharmacology. 55 (7): 1035–1043. doi:10.1016/s0006-2952(97)00631-x. PMID 9605427.
- ^ Neve KA, Henningsen RA, Kinzie JM, De Paulis T, Schmidt DE, Kessler RM, et al. (March 1990). "Sodium-dependent isomerization of dopamine D-2 receptors characterized using [125I]epidepride, a high-affinity substituted benzamide ligand". The Journal of Pharmacology and Experimental Therapeutics. 252 (3): 1108–1116. PMID 2138666.
- ^ Weber E, Sonders M, Quarum M, McLean S, Pou S, Keana JF (November 1986). "1,3-Di(2-[5-3H]tolyl)guanidine: a selective ligand that labels sigma-type receptors for psychotomimetic opiates and antipsychotic drugs". Proceedings of the National Academy of Sciences of the United States of America. 83 (22): 8784–8788. Bibcode:1986PNAS...83.8784W. doi:10.1073/pnas.83.22.8784. PMC 387016. PMID 2877462.
- ^ Kenakin T (2009). "Ligand-Receptor Binding and Tissue Response". In Hacker M, Messer W, Bachmann K (eds.). Pharmacology. Elsevier. p. 65. ISBN 9780123695215.
- ^ Molderings GJ, Donecker K, Burian M, Simon WA, Schröder DW, Göthert M (April 1998). "Characterization of I2 imidazoline and sigma binding sites in the rat and human stomach". The Journal of Pharmacology and Experimental Therapeutics. 285 (1): 170–177. PMID 9536007.
- ^ Reis DJ, Piletz JE (1997). "The imidazoline receptor in control of blood pressure by clonidine and drugs". American Journal of Physiology. 273 (5): R1569–R1571. doi:10.1152/ajpregu.1997.273.5.R1569. PMID 9374795.
- ^ Giovannitti JA, Thoms SM, Crawford JJ (2015). "Alpha-2 adrenergic receptor agonists: a review of current clinical applications". Anesthesia Progress. 62 (1): 31–39. doi:10.2344/0003-3006-62.1.31. PMC 4389556. PMID 25849473.
- ^ "Catapres- clonidine hydrochloride tablet". DailyMed. 6 September 2016. Archived from the original on 4 August 2020. Retrieved 21 December 2019.
The antihypertensive effect is reached at plasma concentrations between about 0.2 and 2.0 ng/mL in patients with normal excretory function. A further rise in the plasma levels will not enhance the antihypertensive effect.
- ^ a b c Cinnamon Bidwell L, Dew RE, Kollins SH (October 2010). "Alpha-2 adrenergic receptors and attention-deficit/hyperactivity disorder". Current Psychiatry Reports. 12 (5): 366–373. doi:10.1007/s11920-010-0136-4. PMC 3676929. PMID 20652773.
- ^ Low LC (1991). "Growth hormone-releasing hormone: clinical studies and therapeutic aspects". Neuroendocrinology. 53 (Suppl 1): 37–40. doi:10.1159/000125793. PMID 1901390.
- ^ "Growth Hormone Test". www.cincinnatichildrens.org. Cincinnati Children's Hospital Medical Center. Archived from the original on 14 October 2018. Retrieved 13 October 2018.
- ^ a b c d e Khan ZP, Ferguson CN, Jones RM (February 1999). "alpha-2 and imidazoline receptor agonists. Their pharmacology and therapeutic role". Anaesthesia. 54 (2): 146–165. doi:10.1046/j.1365-2044.1999.00659.x. PMID 10215710. S2CID 28405271.
- ^ Foye's principles of medicinal chemistry (6th ed.). Philadelphia: Lippincott Williams & Wilkins. 2008. p. 403. ISBN 9780781768795.
- ^ Pajouhesh H, Lenz GR (October 2005). "Medicinal chemical properties of successful central nervous system drugs". NeuroRx. 2 (4): 541–553. doi:10.1602/neurorx.2.4.541. PMC 1201314. PMID 16489364.
- ^ Skingle M, Hayes AG, Tyers MB (September 1982). "Antinociceptive activity of clonidine in the mouse, rat and dog". Life Sciences. 31 (11): 1123–1132. doi:10.1016/0024-3205(82)90086-8. PMID 6128647.
- ^ Curtis AL, Marwah J (July 1987). "Alpha adrenoceptor modulation of the jaw-opening reflex". Neuropharmacology. 26 (7A): 649–655. doi:10.1016/0028-3908(87)90224-3. PMID 2819761. S2CID 41743285.
- ^ Frisk-Holmberg M, Paalzow L, Edlund PO (November 1981). "Clonidine kinetics in man--evidence for dose dependency and changed pharmacokinetics during chronic therapy". British Journal of Clinical Pharmacology. 12 (5): 653–658. doi:10.1111/j.1365-2125.1981.tb01284.x. PMC 1401969. PMID 7332729.
- ^ Dollery CT, Davies DS, Draffan GH, Dargie HJ, Dean CR, Reid JL, et al. (January 1976). "Clinical pharmacology and pharmacokinetics of clonidine". Clinical Pharmacology and Therapeutics. 19 (1): 11–17. doi:10.1002/cpt197619111. PMID 1245090. S2CID 39473828.
- ^ Keränen A, Nykänen S, Taskinen J (May 1978). "Pharmacokinetics and side-effects of clonidine". European Journal of Clinical Pharmacology. 13 (2): 97–101. doi:10.1007/BF00609752. PMID 658114. S2CID 24702183.
- ^ Stähle H (June 2000). "A historical perspective: development of clonidine". Best Practice & Research Clinical Anaesthesiology. 14 (2): 237–246. doi:10.1053/bean.2000.0079.
- ^ "Clonidine: Drug Uses, Dosage & Side Effects - Drugs.com". Drugs.com. Archived from the original on 14 April 2017. Retrieved 10 December 2017.
- ^ a b "Clonidine brand names". Drugs.com. Archived from the original on 6 August 2017. Retrieved 16 June 2017.
External links
[edit]- Alpha-2 agonists in ADHD


