User:Nargisaslami/sandbox
 | This is a user sandbox of Nargisaslami. You can use it for testing or practicing edits. This is not the sandbox where you should draft your assigned article for a dashboard.wikiedu.org course. To find the right sandbox for your assignment, visit your Dashboard course page and follow the Sandbox Draft link for your assigned article in the My Articles section. |
| Nargisaslami/sandbox |
|---|
The long-term effects of alcohol (also known formerly as ethanol) consumption range from cardioprotective health benefits for low to moderate alcohol consumption in industrialized societies with higher rates of cardiovascular disease[1][2] to severe detrimental effects in cases of chronic alcohol abuse.[3] Health effects associated with alcohol intake in large amounts include an increased risk of alcoholism, malnutrition, chronic pancreatitis, alcoholic liver disease, and cancer. In addition, damage to the central nervous system and peripheral nervous system can occur from chronic alcohol abuse.[4][5] The long-term use of alcohol is capable of damaging nearly every organ and system in the body.[6] The developing adolescent brain is particularly vulnerable to the toxic effects of alcohol.[7] In addition, the developing fetal brain is also vulnerable, and fetal alcohol spectrum disorders (FASDs) may result if pregnant mothers consume alcohol.
The inverse relation in Western cultures between alcohol consumption and cardiovascular disease has been known for over 100 years.[8] Many physicians do not promote alcohol consumption, however, given the many health concerns associated with it, some suggest that alcohol should be regarded as a recreational drug, and promote exercise and good nutrition to combat cardiovascular disease.[9][10] Others have argued that the benefits of moderate alcohol consumption may be outweighed by other increased risks, including those of injuries, violence, fetal damage, liver disease, and certain forms of cancer.[11]
Withdrawal effects and dependence are also almost identical.[12] Alcohol at moderate levels has some positive and negative effects on health. The negative effects include increased risk of liver diseases, oropharyngeal cancer, esophageal cancer and pancreatitis. Conversely moderate intake of alcohol may have some beneficial effects on gastritis and cholelithiasis.[13] Of the total number of deaths and diseases caused by alcohol, most happen to the majority of the population who are moderate drinkers, rather than the heavy drinker minority.[14] Chronic alcohol misuse and abuse has serious effects on physical and mental health. Chronic excess alcohol intake, or alcohol dependence, can lead to a wide range of neuropsychiatric or neurological impairment, cardiovascular disease, liver disease, and malignant neoplasms. The psychiatric disorders which are associated with alcoholism include major depression, dysthymia, mania, hypomania, panic disorder, phobias, generalized anxiety disorder, personality disorders, schizophrenia, suicide, neurologic deficits (e.g. impairments of working memory, emotions, executive functions, visuospatial abilities and gait and balance) and brain damage. Alcohol dependence is associated with hypertension, coronary heart disease, and ischemic stroke, cancer of the respiratory system, and also cancers of the digestive system, liver, breast and ovaries. Heavy drinking is associated with liver disease, such as cirrhosis.[15] Excessive alcohol consumption can have a negative impact on aging.[16]
Recent studies have focused on understanding the mechanisms by which moderate alcohol consumption confers cardiovascular benefit.[17]
Maximum quantity recommended
[edit]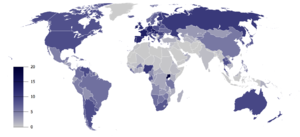
Different countries recommend different maximum quantities. For most countries, the maximum quantity for men is 140 g–210 g per week. For women, the range is 84 g–140 g per week.[citation needed] Most countries recommend total abstinence during pregnancy and lactation.
Alcohol-related death
[edit]
Over-consumption of alcohol causes many deaths worldwide. The overall mortality from alcohol use was found to be similar to that of the effect of physical inactivity.[19] A review in 2009 found that "the net effect of alcohol consumption on health is detrimental, with an estimated 3.8% of all global deaths and 4.6% of global disability-adjusted life-years attributable to alcohol."[20]
Extensive research of Western cultures has consistently shown increased survival associated with light to moderate alcohol consumption.[21][22] A 23-year prospective study of 12,000 male British physicians aged 48–78, found that overall mortality was significantly lower in current drinkers compared to non-drinkers even after correction for ex-drinkers. This benefit was strongest for ischemic heart disease, but was also noted for other vascular disease and respiratory disease. Death rate amongst current drinkers was higher for 'alcohol augmentable' disease such as liver disease and oral cancers, but these deaths were much less common than cardiovascular and respiratory deaths. The lowest mortality rate was found for consumption of 8 to 14 'units' per week. In the UK a unit is defined as 10ml or 8g of pure alcohol.[23] Higher consumption increased overall mortality rate, but not above that of non-drinkers.[24] Other studies have found age-dependent mortality risks of low-to-moderate alcohol use: an increased risk for individuals aged 16–34 (due to increased risk of cancers, accidents, liver disease, and other factors), but a decreased risk for individuals ages 55+ (due to lower incidence of ischemic heart disease).[25]
This is consistent with other research that found a J-curve dependency between alcohol consumption and total mortality among middle aged and older men. While the mortality rates of ex-drinkers and heavy drinkers are significantly elevated, the all-cause mortality rates may be 15-18% lower among moderate drinkers. Although the definition of a drink varies between studies and countries, this meta-analysis found that low levels of alcohol intake, defined as 1-2 drinks per day for women and 2-4 drinks per day for men, was associated with lower mortality than abstainers.[26] This claim was challenged by another study[27][28] that found that in certain low quality studies occasional drinkers or ex-drinkers were included as abstainers, resulting in the increased mortality in that group. However, the J-curve for total and CHD mortality was reconfirmed by studies that took the mentioned confounders into account.[29][30][31][32] There seems to be little discussion of what proportion of individuals classified as abstainers are those already at greater risk of mortality due to chronic conditions and do not or cannot consume alcohol for reasons of health or harmful interactions with medication.
The observed decrease in mortality of light-to-moderate drinkers compared to never drinkers might be partially explained by superior health and social status of the drinking group;[33] however, the protective effect of alcohol in light to moderate drinkers remains significant even after adjusting for these confounders.[30][32] Additionally, confounders such as underreporting of alcohol intake might lead to the underestimation of how much mortality is reduced in light-to-moderate drinkers.[29][34]
A 2010 study confirmed the beneficial effect of moderate alcohol consumption on mortality.[32] Subjects were grouped into abstainers, light, moderate, and heavy drinkers. The order of mortality rates from lowest to highest were moderate, light, heavy, and abstainers. The increased risk for abstainers was twice the mortality rate as for moderate drinkers. This study specifically sought to control for confounding factors including the problem of ex-drinkers considered as non-drinkers.[32] According to another study, drinkers with heavy drinking occasions (six or more drinks at a time) have a 57% higher all-cause mortality than drinkers without heavy drinking occasions.[35]
Mortality is lowest among young abstainers and highest among young heavy drinkers.[36]
In contrast to studies of Western cultures, research in other cultures has yielded some opposite findings. The landmark INTERHEART Study has revealed that alcohol consumption in South Asians was not protective against CAD in sharp contrast to other populations who benefit from it.[37] In fact Asian Indians who consume alcohol had a 60% higher risk of heart attack which was greater with local spirits (80%) than branded spirits (50%).[38] The harm was observed in alcohol users classified as occasional as well as regular light, moderate, and heavy consumers.[38]
Another large study of 4465 subjects in India also confirmed the possible harm of alcohol consumption on coronary risk in men. Compared to lifetime abstainers, alcohol users had higher blood sugar (2 mg/dl), blood pressure (2 mm Hg) levels, and the HDL-C levels (2 mg/dl) and significantly higher tobacco use (63% vs. 21%).[38]
Many countries collect statistics on alcohol-related deaths. While some categories relate to short-term effects, such as accidents, many relate to long-term effects of alcohol.
Russia
[edit]One study claims that "excessive alcohol consumption in Russia, particularly by men, has in recent years caused more than half of all the deaths at ages 15-54 years."[39] However, there are some difficulties with this study. For instance the same study also found a protective effect of heavy drinking on breast cancer mortality. This contradicts the well established scientific view that alcohol increases breast cancer risk.[40] On this account in further correspondence it was advised that "careful interpretation of mortality statistics in relation to alcohol use is needed, taking into account other relevant risk factors, incidence, and survival."[41]
The authors replied that "whether or not the apparent shortfall in breast cancer mortality among heavy drinkers is real, it accounts for only about 0·1% of adult deaths in Russia. Careful interpretation of it is therefore of little relevance to the findings for alcohol and overall mortality".
United Kingdom
[edit]A governmental report from Britain has found that "There were 8,724 alcohol-related deaths in 2007, lower than 2006, but more than double the 4,144 recorded in 1991. The alcohol-related death rate was 13.3 per 100,000 population in 2007, compared with 6.9 per 100,000 population in 1991."[42] In Scotland, the NHS estimate that in 2003 one in every 20 deaths could be attributed to alcohol.[43] A 2009 report noted that the death rate from alcohol-related disease was 9,000, a number three times that of 25 years previously.[44]
A UK report came to the result that the effects of low-to-moderate alcohol consumption on mortality are age-dependent. Low-to-moderate alcohol use increases the risk of death for individuals aged 16–34 (due to increased risk of cancers, accidents, liver disease, and other factors), but decreases the risk of death for individuals ages 55+ (due to decreased risk of ischemic heart disease).[45]
A study in the United Kingdom found that alcohol causes about 4% of cancer cases in the UK (12,500 cases per year).[46]
United States
[edit]The Centers for Disease Control and Prevention report, "From 2001–2005, there were approximately 79,000 deaths annually attributable to excessive alcohol use. In fact, excessive alcohol use is the 3rd leading lifestyle-related cause of death for people in the United States each year."[47] A 1993 study estimated US deaths through alcohol at 100,000.[48]
Another Centers for Disease Control report from 2001 estimated that medium and high consumption of alcohol led to 75,754 deaths in the United States in 2001. Low consumption of alcohol had some beneficial effects, so a net 59,180 deaths were attributed to alcohol.[49]
Longevity
[edit]In 2016, a meta-analysis of 87 studies investigating alcohol use and mortality risk was conducted. The studies analyzed had shown the largest mortality risk reduction in moderate drinkers, but these studies did not correct for confounding variables common with certain abstainers, such as previous alcoholism, and chronic health issues. After adjusting these studies for abstainer biases, no reduction in mortality risk was found for low-volume drinkers.[50] However, there have been individual studies that show abstainers and heavy drinkers have an increased mortality of about 50% over moderate drinkers after adjustment for confounding factors.[51]
Some animal studies have found increased longevity with exposure to various alcohols. The roundworm Caenorhabditis elegans has been used as a model for aging and age-related diseases.[52] The lifespan of these worms has been shown to double when fed 0.005% ethanol, but does not markedly increase at higher concentrations. Supplementing starved cultures with n-propanol and n-butanol also extended lifespan.[53]
Cardiovascular system
[edit]A meta-analysis of 34 studies found a reduced risk of mortality from coronary heart disease in men who drank 2 - 4 drinks per day and women who drank 1 - 2 drinks per day.[26] Alcohol has been found to have anticoagulant properties.[54][55] Thrombosis is lower among moderate drinkers than abstainers.[56] A meta-analysis of randomized trials found that alcohol consumption in moderation decreases serum levels of fibrinogen, a protein that promotes clot formation, while it increases levels of tissue type plasminogen activator, an enzyme that helps dissolve clots.[57] These changes were estimated to reduce coronary heart disease risk by about 24%. Another meta-analysis in 2011 found favorable changes in HDL cholesterol, adiponectin, and fibrinogen associated with moderate alcohol consumption.[58]
Also, serum levels of C-reactive protein (CRP), a marker of inflammation and predictor of CHD (coronary heart disease) risk, are lower in moderate drinkers than in those who abstain from alcohol, suggesting that alcohol consumption in moderation might have anti-inflammatory effects.[59][60][61]
Despite epidemiological evidence, many have cautioned against recommendations for the use of alcohol for health benefits. A physician from the World Health Organisation labeled such alcohol promotion as "ridiculous and dangerous".[62][63] One reviewer has noted, "Despite the wealth of observational data, it is not absolutely clear that alcohol reduces cardiovascular risk, because no randomized controlled trials have been performed. Alcohol should never be recommended to patients to reduce cardiovascular risk as a substitute for the well-proven alternatives of appropriate diet, exercise, and drugs."[64] It has been argued[who?] that the health benefits from alcohol are at best debatable and may have been exaggerated by the alcohol industry. Some investigators hold that alcohol should be regarded as a recreational drug with potentially serious adverse effects on health and should not be promoted for cardio-protection.[9]
Nevertheless, a large prospective non-randomized study has shown that moderate alcohol intake in individuals already at low risk based on body mass index, physical activity, smoking, and diet, yields further improvement in cardiovascular risk.[65] Furthermore, a multicenter randomized diet study published in 2013 found that a Mediterranean-diet, which included an encouragement to daily wine consumption in habitual drinkers, led to a dramatic reduction in cardiovascular events.[66]
Peripheral arterial disease
[edit]A prospective study published in 1997 found "moderate alcohol consumption appears to decrease the risk of PAD in apparently healthy men."[67] In a large population-based study, moderate alcohol consumption was inversely associated with peripheral arterial disease in women but not in men. But when confounding by smoking was considered, the benefit extended to men. The study concluded "an inverse association between alcohol consumption and peripheral arterial disease was found in nonsmoking men and women."[68][69]
Intermittent claudication
[edit]A study found that moderate consumption of alcohol had a protective effect against intermittent claudication. The lowest risk was seen in men who drank 1 to 2 drinks per day and in women who drank half to 1 drink per day.[70]
Heart attack and stroke
[edit]Drinking in moderation has been found to help those who have suffered a heart attack survive it.[71][72][73] However, excessive alcohol consumption leads to an increased risk of heart failure.[74] A review of the literature found that half a drink of alcohol offered the best level of protection. However, they noted that at present there have been no randomised trials to confirm the evidence which suggests a protective role of low doses of alcohol against heart attacks.[75] However, moderate alcohol consumption is associated with hypertension.[11] There is an increased risk of hypertriglyceridemia, cardiomyopathy, hypertension, and stroke if 3 or more standard drinks of alcohol are taken per day.[76]
Cardiomyopathy
[edit]Large amount of alcohol over the long term can lead to alcoholic cardiomyopathy. Alcoholic cardiomyopathy presents in a manner clinically identical to idiopathic dilated cardiomyopathy, involving hypertrophy of the musculature of the heart that can lead to congestive heart failure.[77]
Hematologic diseases
[edit]Alcoholics may have anemia from several causes;[78] they may also develop thrombocytopenia from direct toxic effect on megakaryocytes, or from hypersplenism.
Atrial fibrillation
[edit]Alcohol consumption increases the risk of atrial fibrillation, a type of abnormal heart rhythm. This remains true even at moderate levels of consumption.[79]
Nervous system
[edit]
Chronic heavy alcohol consumption impairs brain development, causes alcohol dementia, brain shrinkage, physical dependence, alcoholic polyneuropathy (also known as 'alcohol leg'), increases neuropsychiatric and cognitive disorders and causes distortion of the brain chemistry. At present, due to poor study design and methodology, the literature is inconclusive on whether moderate alcohol consumption increases the risk of dementia or decreases it.[80] Evidence for a protective effect of low to moderate alcohol consumption on age-related cognitive decline and dementia has been suggested by some research; however, other research has not found a protective effect of low to moderate alcohol consumption.[81] Some evidence suggests that low to moderate alcohol consumption may speed up brain volume loss.[82] Chronic consumption of alcohol may result in increased plasma levels of the toxic amino acid homocysteine;[83][84] which may explain alcohol withdrawal seizures,[85] alcohol-induced brain atrophy[86] and alcohol-related cognitive disturbances.[87] Alcohol's impact on the nervous system can also include disruptions of memory and learning (see Effects of alcohol on memory), such as resulting in a blackout phenomenon.
Strokes
[edit]Epidemiological studies of middle-aged populations generally find the relationship between alcohol intake and the risk of stroke to be either U- or J-shaped.[88][89][90][91] There may be very different effects of alcohol based on the type of stroke studied. The predominant form of stroke in Western cultures is ischemic, whereas non-western cultures have more hemorrhagic stroke. In contrast to the beneficial effect of alcohol on ischemic stroke, consumption of more than 2 drinks per day increases the risk of hemorrhagic stroke. The National Stroke Association estimates this higher amount of alcohol increases stroke risk by 50%.[92] "For stroke, the observed relationship between alcohol consumption and risk in a given population depends on the proportion of strokes that are hemorrhagic. Light-to-moderate alcohol intake is associated with a lower risk of ischemic stroke which is likely to be, in part, causal. Hemorrhagic stroke, on the other hand, displays a loglinear relationship with alcohol intake."[93]
Brain
[edit]Alcohol abuse is associated with widespread and significant brain lesions. Alcohol related brain damage is not only due to the direct toxic effects of alcohol; alcohol withdrawal, nutritional deficiency, electrolyte disturbances, and liver damage are also believed to contribute to alcohol-related brain damage.[94]
Cognition and dementia
[edit]Excessive alcohol intake is associated with impaired prospective memory. This impaired cognitive ability leads to increased failure to carry out an intended task at a later date, for example, forgetting to lock the door or to post a letter on time. The higher the volume of alcohol consumed and the longer consumed, the more severe the impairments.[95] One of the organs most sensitive to the toxic effects of chronic alcohol consumption is the brain. In the United States approximately 20% of admissions to mental health facilities are related to alcohol-related cognitive impairment, most notably alcohol-related dementia. Chronic excessive alcohol intake is also associated with serious cognitive decline and a range of neuropsychiatric complications. The elderly are the most sensitive to the toxic effects of alcohol on the brain.[96] There is some inconclusive evidence that small amounts of alcohol taken in earlier adult life is protective in later life against cognitive decline and dementia.[97] However, a study concluded, "Our findings suggest that, despite previous suggestions, moderate alcohol consumption does not protect older people from cognitive decline."[98]
There is tentative evidence that drinking a small amount of alcohol may decrease the risk of Alzheimer's disease latter in life.[99]
Wernicke–Korsakoff syndrome is a manifestation of thiamine deficiency, usually as a secondary effect of alcohol abuse.[100] The syndrome is a combined manifestation of two eponymous disorders, Korsakoff's Psychosis and Wernicke's encephalopathy, named after Drs. Sergei Korsakoff and Carl Wernicke. Wernicke's encephalopathy is the acute presentation of the syndrome and is characterised by a confusional state while Korsakoff's psychosis main symptoms are amnesia and executive dysfunction.[101] Banana bags, a bag of intravenous fluids containing vitamins and minerals, can be used to mitigate these outcomes.[102][103]
Essential tremor
[edit]Essential tremors—or, in the case of essential tremors on a background of family history of essential tremors, familial tremors—can be temporarily relieved in up to two-thirds of patients by drinking small amounts of alcohol.[104]
Ethanol is known to activate aminobutyric acid type A (GABAA) and inhibit N-methyl-D-aspartate (NMDA) glutamate receptors, which are both implicated in essential tremor pathology[105] and could underlie the ameliorative effects.[106][107] Additionally, the effects of ethanol have been studied in different animal essential tremor models. (For more details on this topic, see Essential tremor.)
Sleep
[edit]Chronic use of alcohol used to induce sleep can lead to insomnia: frequent moving between sleep stages occurs, with awakenings due to headaches and diaphoresis. Stopping chronic alcohol abuse can also lead to profound disturbances of sleep with vivid dreams. Chronic alcohol abuse is associated with NREM stage 3 and 4 sleep as well as suppression of REM sleep and REM sleep fragmentation. During withdrawal REM sleep is typically exaggerated as part of a rebound effect.[108]
Mental health effects
[edit]High rates of major depressive disorder occur in heavy drinkers and those who abuse alcohol. Whether it is more true that major depressive disorder causes self-medicating alcohol abuse, or the increased incidence of the disorder in alcohol abusers is caused by the drinking, is not known though some evidence suggests drinking causes the disorder.[109] Alcohol misuse is associated with a number of mental health disorders and alcoholics have a very high suicide rate.[110] A study of people hospitalised for suicide attempts found that those who were alcoholics were 75 times more likely to go on to successfully commit suicide than non-alcoholic suicide attempters.[111] In the general alcoholic population the increased risk of suicide compared to the general public is 5-20 times greater. About 15 percent of alcoholics commit suicide. Abuse of other drugs is also associated with an increased risk of suicide. About 33 percent of suicides in the under 35s are due to alcohol or other substance misuse.[112]
Social skills are significantly impaired in people suffering from alcoholism due to the neurotoxic effects of alcohol on the brain, especially the prefrontal cortex area of the brain. The social skills that are impaired by alcohol abuse include impairments in perceiving facial emotions, prosody perception problems and theory of mind deficits; the ability to understand humour is also impaired in alcohol abusers.[113]
Studies have shown that alcohol dependence relates directly to cravings and irritability.[114] Another study has shown that alcohol use is a significant predisposing factor towards antisocial behavior in children.[115] Depression, anxiety and panic disorder are disorders commonly reported by alcohol dependent people. Alcoholism is associated with dampened activation in brain networks responsible for emotional processing (e.g. the amygdala and hippocampus).[116] Evidence that the mental health disorders are often induced by alcohol misuse via distortion of brain neurochemistry is indicated by the improvement or disappearance of symptoms that occurs after prolonged abstinence, although problems may worsen in early withdrawal and recovery periods.[117][118][119] Psychosis is secondary to several alcohol-related conditions including acute intoxication and withdrawal after significant exposure.[120] Chronic alcohol misuse can cause psychotic type symptoms to develop, more so than with other drugs of abuse. Alcohol abuse has been shown to cause an 800% increased risk of psychotic disorders in men and a 300% increased risk of psychotic disorders in women which are not related to pre-existing psychiatric disorders. This is significantly higher than the increased risk of psychotic disorders seen from cannabis use making alcohol abuse a very significant cause of psychotic disorders.[121] Approximately 3 percent of people who are alcohol dependent experience psychosis during acute intoxication or withdrawal. Alcohol-related psychosis may manifest itself through a kindling mechanism. The mechanism of alcohol-related psychosis is due to distortions to neuronal membranes, gene expression, as well as thiamin deficiency. It is possible in some cases that alcohol abuse via a kindling mechanism can cause the development of a chronic substance-induced psychotic disorder, i.e. schizophrenia. The effects of an alcohol-related psychosis include an increased risk of depression and suicide as well as psychosocial impairments.[120] However, moderate wine drinking has been shown to lower the risk for depression.[122]
While alcohol initially helps social phobia or panic symptoms, with longer term alcohol misuse can often worsen social phobia symptoms and can cause panic disorder to develop or worsen, during alcohol intoxication and especially during the alcohol withdrawal syndrome. This effect is not unique to alcohol but can also occur with long-term use of drugs which have a similar mechanism of action to alcohol such as the benzodiazepines, which are sometimes prescribed as tranquillizers to people with alcohol problems.[123] Approximately half of patients attending mental health services for conditions including anxiety disorders such as panic disorder or social phobia suffer from alcohol or benzodiazepine dependence. It was noted that every individual has an individual sensitivity level to alcohol or sedative hypnotic drugs and what one person can tolerate without ill health another will suffer very ill health and that even moderate drinking can cause rebound anxiety syndromes and sleep disorders. A person who is suffering the toxic effects of alcohol will not benefit from other therapies or medications as they do not address the root cause of the symptoms.[124]
Addiction to alcohol, as with any drug of abuse tested so far, has been correlated with an enduring reduction in the expression of GLT1 (EAAT2) in the nucleus accumbens and is implicated in the drug-seeking behavior expressed nearly universally across all documented addiction syndromes. This long-term dysregulation of glutamate transmission is associated with an increase in vulnerability to both relapse-events after re-exposure to drug-use triggers as well as an overall increase in the likelihood of developing addiction to other reinforcing drugs. Drugs which help to re-stabilize the glutamate system such as N-acetylcysteine have been proposed for the treatment of addiction to cocaine, nicotine, and alcohol.[125]
Digestive system and weight gain
[edit]The impact of alcohol on weight-gain is contentious: some studies find no effect,[126] others find decreased[127] or increased effect on weight gain.
Alcohol use increases the risk of chronic gastritis (stomach inflammation);[3][128] it is one cause of cirrhosis, hepatitis, and pancreatitis in both its chronic and acute forms.
Metabolic syndrome
[edit]A study concluded, "Mild to moderate alcohol consumption is associated with a lower prevalence of the metabolic syndrome, with a favorable influence on lipids, waist circumference, and fasting insulin. This association was strongest among whites and among beer and wine drinkers."[129] This is also true for Asians. A J-curve association between alcohol intake and metabolic syndrome was found: "The results of the present study suggest that the metabolic syndrome is negatively associated with light alcohol consumption (1–15 g alcohol/d) in Korean adults". However, "odds ratios for the metabolic syndrome and its components tended to increase with increasing alcohol consumption."[130]
Gallbladder effects
[edit]Research has found that drinking reduces the risk of developing gallstones. Compared with alcohol abstainers, the relative risk of gallstone disease, controlling for age, sex, education, smoking, and body mass index, is 0.83 for occasional and regular moderate drinkers (< 25 ml of ethanol per day), 0.67 for intermediate drinkers (25-50 ml per day), and 0.58 for heavy drinkers. This inverse association was consistent across strata of age, sex, and body mass index."[131] Frequency of drinking also appears to be a factor. "An increase in frequency of alcohol consumption also was related to decreased risk. Combining the reports of quantity and frequency of alcohol intake, a consumption pattern that reflected frequent intake (5-7 days/week) of any given amount of alcohol was associated with a decreased risk, as compared with nondrinkers. In contrast, infrequent alcohol intake (1-2 days/week) showed no significant association with risk."[132]
A large self-reported study published in 1998 found no correlation between gallbladder disease and multiple factors including smoking, alcohol consumption, hypertension, and coffee consumption.[133] A retrospective study from 1997 found vitamin C (ascorbic acid) supplement use in drinkers was associated with a lower prevalence of gallbladder disease, but this association was not seen in non-drinkers.[134]
Liver disease
[edit]Alcoholic liver disease is a major public health problem. For example, in the United States up to two million people have alcohol-related liver disorders.[135] Chronic alcohol abuse can cause fatty liver, cirrhosis and alcoholic hepatitis. Treatment options are limited and consist of most importantly discontinuing alcohol consumption. In cases of severe liver disease, the only treatment option may be a liver transplant from alcohol abstinent donors. Research is being conducted into the effectiveness of anti-TNFs. Certain complementary medications, e.g., milk thistle and silymarin, appear to offer some benefit.[135][136] Alcohol is a leading cause of liver cancer in the Western world, accounting for 32-45% of hepatic cancers. Up to half a million people in the United States develop alcohol-related liver cancer.[137][138] Moderate alcohol consumption also increases the risk of liver disease.[11]
Pancreatitis
[edit]Alcohol abuse is a leading cause of both acute pancreatitis and chronic pancreatitis.[139][140] Alcoholic pancreatitis can result in severe abdominal pain and may progress to pancreatic cancer.[141] Chronic pancreatitis often results in intestinal malabsorption, and can result in diabetes.[142]
Other systems
[edit]Respiratory system
[edit]Chronic alcohol ingestion can impair multiple critical cellular functions in the lungs.[citation needed] These cellular impairments can lead to increased susceptibility to serious complications from lung disease. Recent research cites alcoholic lung disease as comparable to liver disease in alcohol-related mortality.[citation needed] Alcoholics have a higher risk of developing acute respiratory distress syndrome (ARDS) and experience higher rates of mortality from ARDS when compared to non-alcoholics.[citation needed] Despite these effects, a large prospective study has shown a protective effect of moderate alcohol consumption on respiratory mortality.[24]
Kidney stones
[edit]Research indicates that drinking alcohol is associated with a lower risk of developing kidney stones. One study concludes, "Since beer seemed to be protective against kidney stones, the physiologic effects of other substances besides ethanol, especially those of hops, should also be examined."[143] "...consumption of coffee, alcohol, and vitamin C supplements were negatively associated with stones."[144] "After mutually adjusting for the intake of other beverages, the risk of stone formation decreased by the following amount for each 240-ml (8-oz) serving consumed daily: caffeinated coffee, 10%; decaffeinated coffee, 10%; tea, 14%; beer, 21%; and wine, 39%."[145] "...stone formation decreased by the following amount for each 240-mL (8-oz) serving consumed daily: 10% for caffeinated coffee, 9% for decaffeinated coffee, 8% for tea, and 59% for wine." (CI data excised from last two quotes.).[146]
Sexual dysfunction
[edit]Long term excessive intake of alcohol can lead to damage to the central nervous system and the peripheral nervous system resulting in loss of sexual desire and impotence in men.[147] This is caused by reduction of testosterone from ethanol-induced testicular atrophy, resulting in increased feminisation of males and is a clinical feature of alcohol abusing males who have cirrhosis of the liver.[148]
Hormonal Imbalance
[edit]Excessive alcohol intake can result in hyperoestrogenisation.[149] It has been speculated that alcohol beverages may contain estrogen like compounds. In men, high levels of estrogen can lead to testicular failure and the development of feminine traits including development of male breasts, called gynecomastia.[150][151] In women, increased levels of estrogen due to excessive alcohol intake have been related to an increased risk of breast cancer.[151][152]
Diabetes mellitus
[edit]A meta-analysis found with data from 477,200 individuals determined the dose-response relationships by sex and end point using lifetime abstainers as the reference group. The search revealed 20 cohort studies that met our inclusion criteria. A U-shaped relationship was found for both sexes. Compared with lifetime abstainers, the relative risk (RR) for type 2 diabetes among men was most protective when consuming 22 g/day alcohol (RR 0.87 [95% CI 0.76–1.00]) and became deleterious at just over 60 g/day alcohol (1.01 [0.71–1.44]). Among women, consumption of 24 g/day alcohol was most protective (0.60 [0.52–0.69]) and became deleterious at about 50 g/day alcohol (1.02 [0.83–1.26]).
Because former drinkers may be inspired to abstain due to health concerns, they may actually be at increased risk of developing diabetes, known as the sick-quitter effect. Moreover, the balance of risk of alcohol consumption on other diseases and health outcomes, even at moderate levels of consumption, may outweigh the positive benefits with regard to diabetes.
Additionally, the way in which alcohol is consumed (i.e., with meals or bingeing on weekends) affects various health outcomes. Thus, it may be the case that the risk of diabetes associated with heavy alcohol consumption is due to consumption mainly on the weekend as opposed to the same amount spread over a week.[153] In the United Kingdom "advice on weekly consumption is avoided".
Also, a twenty-year twin study from Finland has shown that moderate alcohol consumption may reduce the risk of type 2 diabetes in men and women. However, binge drinking and high alcohol consumption was found to increase the risk of type 2 diabetes in women. [154] A study in mice has suggested a beneficial effect of alcohol in promoting insulin sensitivity.[155]
Rheumatoid arthritis
[edit]Regular consumption of alcohol is associated with an increased risk of gouty arthritis[156][157] and a decreased risk of rheumatoid arthritis.[158][159][160][161][162] Two recent studies report that the more alcohol consumed, the lower the risk of developing rheumatoid arthritis. Among those who drank regularly, the one-quarter who drank the most were up to 50% less likely to develop the disease compared to the half who drank the least.[163]
The researchers noted that moderate alcohol consumption also reduces the risk of other inflammatory processes such as cardiovascualar disease. Some of the biological mechanisms by which ethanol reduces the risk of destructive arthritis and prevents the loss of bone mineral density (BMD), which is part of the disease process.[164]
A study concluded, "Alcohol either protects from RA or, subjects with RA curtail their drinking after the manifestation of RA".[165] Another study found, "Postmenopausal women who averaged more than 14 alcoholic drinks per week had a reduced risk of rheumatoid arthritis..."[166]
Osteoporosis
[edit]Moderate alcohol consumption is associated with higher bone mineral density in postmenopausal women. "...Alcohol consumption significantly decreased the likelihood [of osteoporosis]."[167] "Moderate alcohol intake was associated with higher BMD in postmenopausal elderly women."[168] "Social drinking is associated with higher bone mineral density in men and women [over 45]."[169] However, alcohol abuse is associated with bone loss.[170][171]
Skin
[edit]Chronic excessive alcohol abuse is associated with a wide range of skin disorders including urticaria, porphyria cutanea tarda, flushing, cutaneous stigmata of cirrhosis, psoriasis, pruritus, seborrheic dermatitis and rosacea.[172]
A 2010 study concluded, "Nonlight beer intake is associated with an increased risk of developing psoriasis among women. Other alcoholic beverages did not increase the risk of psoriasis in this study."[173]
Immune system
[edit]Bacterial infection
[edit]There is a protective effect of alcohol consumption against active infection with H. pylori[174] In contrast, alcohol intake (comparing those who drink > 30g of alcohol per day to non-drinkers) is not associated with higher risk of duodenal ulcer.[175] Excessive alcohol consumption seen in alcoholics is a known risk factor for pneumonia.
Common cold
[edit]A study on the common cold found that "Greater numbers of alcoholic drinks (up to three or four per day) were associated with decreased risk for developing colds because drinking was associated with decreased illness following infection. However, the benefits of drinking occurred only among nonsmokers. [...] Although alcohol consumption did not influence risk of clinical illness for smokers, moderate alcohol consumption was associated with decreased risk for nonsmokers."[176]
Another study concluded, "Findings suggest that wine intake, especially red wine, may have a protective effect against common cold. Beer, spirits, and total alcohol intakes do not seem to affect the incidence of common cold."[177]
Cancer
[edit]In 1988 the International Agency for Research on Cancer (Centre International de Recherche sur le Cancer) of the World Health Organization classified alcohol as a Group 1 carcinogen, stating "There is sufficient evidence for the carcinogenicity of alcoholic beverages in humans.... Alcoholic beverages are carcinogenic to humans (Group 1)."[178] The U.S. Department of Health & Human Services’ National Toxicology Program in 2000 listed alcohol as a known carcinogen.[179]
It was estimated in 2006 that "3.6% of all cancer cases worldwide are related to alcohol drinking, resulting in 3.5% of all cancer deaths."[180] A European study from 2011 found that one in 10 of all cancers in men and one in 33 in women were caused by past or current alcohol intake.[181][182] The World Cancer Research Fund panel report Food, Nutrition, Physical Activity and the Prevention of Cancer: a Global Perspective finds the evidence "convincing" that alcoholic drinks increase the risk of the following cancers: mouth, pharynx and larynx, oesophagus, colorectum (men), breast (pre- and postmenopause).[183]
Acetaldehyde, a metabolic product of alcohol, is suspected to promote cancer. Typically the liver eliminates 99% of acetaldehyde produced. However, liver disease and certain genetic enzyme deficiencies result in high acetaldehyde levels. Heavy drinkers who are exposed to high acetaldehyde levels due to a genetic defect in alcohol dehydrogenase have been found to be at greater risk of developing cancers of the upper gastrointestinal tract and liver.[184] A review in 2007 found "convincing evidence that acetaldehyde... is responsible for the carcinogenic effect of ethanol... owing to its multiple mutagenic effects on DNA."[185] Acetaldehyde can react with DNA to create DNA adducts including the Cr-Pdg adduct. This Cr-PdG adduct "is likely to play a central role in the mechanism of alcoholic beverage related carcinogenesis."[186] Some have pointed out that even moderate levels of alcohol consumption are associated with an increased risk of certain forms of cancer.[11]
Alcohol's effect on the fetus
[edit]Fetal alcohol syndrome or FAS is a birth defect that occurs in the offspring of women who drink alcohol during pregnancy. Drinking heavily or during the early stages of prenatal development has been conclusively linked to FAS; moderate consumption is associated with fetal damage.[11] Alcohol crosses the placental barrier and can stunt fetal growth or weight, create distinctive facial stigmata, damaged neurons and brain structures, and cause other physical, mental, or behavioural problems.[187] Fetal alcohol exposure is the leading known cause of intellectual disability in the Western world.[188] Alcohol consumption during pregnancy is associated with brain insulin and insulin-like growth factor resistance.[170]
See also
[edit]- Short-term effects of alcohol
- Alcohol and suicide
- Self-medication on CNS depressants (alcohol)
- Self-medicated effectiveness on alcohol
References
[edit]- ^ Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. Paul E Ronksley, Susan E Brien, Barbara J Turner, Kenneth J Mukamal, William A Ghali BMJ 2011;342:d671
- ^ Prospective study of alcohol drinking patterns and coronary heart disease in women and men. Janne Tolstrup, Majken K Jensen, Tjønneland Anne, Kim Overvad, Kenneth J Mukamal, and Morten Grønbæk. BMJ 2006;332:1244.
- ^ a b National Institute on Alcohol Abuse and Alcoholism (NIAAA) (2000). "Health risks and benefits of alcohol consumption" (PDF). Alcohol Res Health. 24 (1): 5–11. doi:10.4135/9781412963855.n839. PMC 6713002. PMID 11199274.
- ^ Müller D, Koch RD, von Specht H, Völker W, Münch EM; Koch; von Specht; Völker; Münch (March 1985). "Neurophysiologic findings in chronic alcohol abuse". Psychiatr Neurol Med Psychol (Leipz) (in German). 37 (3): 129–32. PMID 2988001.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Testino G (2008). "Alcoholic diseases in hepato-gastroenterology: a point of view". Hepatogastroenterology. 55 (82–83): 371–7. PMID 18613369.
- ^ Caan, Woody; Belleroche, Jackie de, eds. (11 April 2002). Drink, Drugs and Dependence: From Science to Clinical Practice (1st ed.). Routledge. pp. 19–20. ISBN 978-0-415-27891-1.
- ^ Guerri C.; Pascual M.A. (2010). "Mechanisms involved in the neurotoxic, cognitive, and neurobehavioral effects of alcohol consumption during adolescence". Alcohol. 44 (1): 15–26. doi:10.1016/j.alcohol.2009.10.003. PMID 20113871.
- ^ Cabot, R.C. (1904). "The relation of alcohol to arteriosclerosis". Journal of the American Medical Association. 43 (12): 774–775. doi:10.1001/jama.1904.92500120002a.
- ^ a b Sellman, D.; Connor, J.; Robinson, G.; Jackson, R. (2009). "Alcohol cardio-protection has been talked up". N Z Med J. 122 (1303): 97–101. PMID 19851424.
- ^ Sinkiewicz, W.; Weglarz, M. (2009). "Alcohol and wine and cardiovascular diseases in epidemiologic studies". Przegl Lek. 66 (5): 233–8. PMID 19739580.
- ^ a b c d e Andréasson, S.; Allebeck, P. (28 February – 6 March 2005). "Alcohol as medication is no good. More risks than benefits according to a survey of current knowledge". Lakartidningen. 102 (9): 632–7. PMID 15804034.
- ^ Gitlow, Stuart (1 October 2006). Substance Use Disorders: A Practical Guide (2nd ed.). USA: Lippincott Williams and Wilkins. pp. 101–103. ISBN 978-0-7817-6998-3.
- ^ Taylor B, Rehm J, Gmel G; Rehm; Gmel (2005). "Moderate alcohol consumption and the gastrointestinal tract". Dig Dis. 23 (3–4): 170–6. doi:10.1159/000090163. PMID 16508280. S2CID 30141003. Archived from the original on November 22, 2011.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "ISCD". "In fact, most of the total number of deaths and diseases caused by alcohol happen to people in the large majority of the population who are ‘moderate’ drinkers, not in the minority who are heavy drinkers."
- ^ Cargiulo T (March 2007). "Understanding the health impact of alcohol dependence". Am J Health Syst Pharm. 64 (5 Suppl 3): S5–11. doi:10.2146/ajhp060647. PMID 17322182.
- ^ Stevenson JS (2005). "Alcohol use, misuse, abuse, and dependence in later adulthood". Annu Rev Nurs Res. 23: 245–80. doi:10.1891/0739-6686.23.1.245. PMID 16350768. S2CID 24586529.
- ^ Vliegenthart R; Oei HH; van den Elzen AP; et al. (November 2004). "Alcohol consumption and coronary calcification in a general population". Arch. Intern. Med. 164 (21): 2355–60. doi:10.1001/archinte.164.21.2355. PMID 15557415.
Koppes LL, Twisk JW, Snel J, Van Mechelen W, Kemper HC (May 2000). "Blood cholesterol levels of 32-year-old alcohol consumers are better than of nonconsumers". Pharmacol Biochem Behav. 66 (1): 163–7. doi:10.1016/S0091-3057(00)00195-7. PMID 10837856. S2CID 23229834.
Albert MA, Glynn RJ, Ridker PM (January 2003). "Alcohol consumption and plasma concentration of C-reactive protein". Circulation. 107 (3): 443–7. doi:10.1161/01.CIR.0000045669.16499.EC. PMID 12551869. S2CID 323583.
Baer DJ; Judd JT; Clevidence BA; et al. (1 March 2002). "Moderate alcohol consumption lowers risk factors for cardiovascular disease in postmenopausal women fed a controlled diet". Am J Clin Nutr. 75 (3): 593–9. doi:10.1093/ajcn/75.3.593. PMID 11864868. - ^ "Global Status Report on Alcohol 2004" (PDF). Retrieved 2014-04-22.
- ^ Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ (May 2006). "Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data". Lancet. 367 (9524): 1747–57. doi:10.1016/S0140-6736(06)68770-9. PMID 16731270. S2CID 22609505.
- ^ Rehm Jürgen; Mathers Colin; Popova Svetlana; Thavorncharoensap Montarat; Teerawattananon Yot; Patra Jayadeep (2014). "Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders". The Lancet. 373 (9682): 2223–2233. doi:10.1016/S0140-6736(09)60746-7. PMID 19560604. S2CID 27947246.
- ^ O'Keefe, JH; Bhatti, SK; Bajwa, A; DiNicolantonio, JJ; Lavie, CJ (March 2014). "Alcohol and cardiovascular health: the dose makes the poison…or the remedy". Mayo Clinic Proceedings. 89 (3): 382–93. doi:10.1016/j.mayocp.2013.11.005. PMID 24582196.
- ^ Di Castelnuovo A, Costanzo S, Bagnardi V, Donati MB, Iacoviello L, de Gaetano G. Alcohol dosing and total mortality in men and women: an updated meta-analysis of 34 prospective studies. Arch Intern Med. 2006 Dec 11-25;166(22) 2437-45.
- ^ [1] Archived September 23, 2012, at the Wayback Machine
- ^ a b Doll R, Peto R, Boreham J, Sutherland I (February 2005). "Mortality in relation to alcohol consumption: a prospective study among male British doctors". Int J Epidemiol. 34 (1): 199–204. doi:10.1093/ije/dyh369. PMID 15647313.
- ^ "'Optimal' levels of alcohol consumption for men and women at different ages, and the all-cause mortality attributable to drinking" (PDF). London: London School of Hygiene and Tropical Medicine. Technical report. 2000.
{{cite web}}: Unknown parameter|authors=ignored (help) - ^ a b Di Castelnuovo, A.; Costanzo, S.; Bagnardi, V.; Donati, MB.; Iacoviello, L.; de Gaetano, G. (2006). "Alcohol dosing and total mortality in men and women: an updated meta-analysis of 34 prospective studies". Arch Intern Med. 166 (22): 2437–45. doi:10.1001/archinte.166.22.2437. PMID 17159008. Cite error: The named reference "Di Castelnuovo-" was defined multiple times with different content (see the help page).
- ^ Fillmore, KM.; Stockwell, T.; Chikritzhs, T.; Bostrom, A.; Kerr, W. (May 2007). "Moderate alcohol use and reduced mortality risk: systematic error in prospective studies and new hypotheses". Ann Epidemiol. 17 (5 Suppl): S16–23. doi:10.1016/j.annepidem.2007.01.005. PMID 17478320.
- ^ Chikritzhs, T.; Fillmore, K.; Stockwell, T. (Jul 2009). "A healthy dose of scepticism: four good reasons to think again about protective effects of alcohol on coronary heart disease". Drug Alcohol Rev. 28 (4): 441–4. doi:10.1111/j.1465-3362.2009.00052.x. hdl:20.500.11937/8299. PMID 19594799.
- ^ a b Klatsky Arthur L.; Udaltsova Natalia (2007). "Alcohol Drinking and Total Mortality Risk". Ann Epidemiol. 17 (5): 555. doi:10.1016/j.annepidem.2007.01.014.
- ^ a b Lee, SJ.; Sudore, RL.; Williams, BA.; Lindquist, K.; Chen, HL.; Covinsky, KE. (Jun 2009). "Functional limitations, socioeconomic status, and all-cause mortality in moderate alcohol drinkers". J Am Geriatr Soc. 57 (6): 955–62. doi:10.1111/j.1532-5415.2009.02184.x. PMC 2847409. PMID 19473456.
- ^ Arriola, L.; Martinez-Camblor, P.; Larrañaga, N.; Basterretxea, M.; Amiano, P.; Moreno-Iribas, C.; Carracedo, R.; Agudo, A.; Ardanaz, E. (Jan 2010). "Alcohol intake and the risk of coronary heart disease in the Spanish EPIC cohort study". Heart. 96 (2): 124–30. doi:10.1136/hrt.2009.173419. PMID 19933099. S2CID 10125924.
- ^ a b c d Holahan, CJ.; Schutte, KK.; Brennan, PL.; Holahan, CK.; Moos, BS.; Moos, RH. (Nov 2010). "Late-life alcohol consumption and 20-year mortality". Alcohol Clin Exp Res. 34 (11): 1961–71. doi:10.1111/j.1530-0277.2010.01286.x. PMID 20735372.
- ^ Hansel, B.; Thomas, F.; Pannier, B.; Bean, K.; Kontush, A.; Chapman, MJ.; Guize, L.; Bruckert, E. (Jun 2010). "Relationship between alcohol intake, health and social status and cardiovascular risk factors in the urban Paris-Ile-De-France Cohort: is the cardioprotective action of alcohol a myth?" (PDF). Eur J Clin Nutr. 64 (6): 561–8. doi:10.1038/ejcn.2010.61. PMID 20485310. S2CID 4488107.
- ^ Klatsky, AL. (Oct 2008). "Invited commentary: never, or hardly ever? It could make a difference". Am J Epidemiol. 168 (8): 872–5, discussion 876–7. doi:10.1093/aje/kwn192. PMID 18701441.
- ^ Laatikainen, T.; Manninen, L.; Poikolainen, K.; Vartiainen, E. (May 2003). "Increased mortality related to heavy alcohol intake pattern". J Epidemiol Community Health. 57 (5): 379–84. doi:10.1136/jech.57.5.379. PMC 1732462. PMID 12700224.
- ^ Andreasson, Sven; Romelsjo, Anders; Allebeck, Peter (2006-01-24). "Alcohol, social factors and mortality among young men". Addiction. 86 (7): 877–887. doi:10.1111/j.1360-0443.1991.tb01843.x. PMID 1912740. Retrieved 2014-04-22.
- ^ Joshi, Prashant; Islam, Shofiqul; Pais, Prem; Reddy, Srinath; Dorairaj, Prabhakaran; Kazmi, Khawar; Pandey, Mrigendra Raj; Haque, Sirajul; Mendis, Shanthi; Rangarajan, Sumathy; Yusuf, Salim (17 January 2007). "Risk Factors for Early Myocardial Infarction in South Asians Compared With Individuals in Other Countries" (PDF). JAMA. 297 (3). American Medical Association: 286–294. doi:10.1001/jama.297.3.286. PMID 17227980. Retrieved 20 March 2012.
- ^ a b c Roy, A.; Prabhakaran, D.; Jeemon, P.; Thankappan, K.R.; Mohan, V.; Ramakrishnan, L.; Joshi, P.; Ahmed, F.; Mohan, B.V.; Saran, R.K.; Sinha, N.; Reddy, K.S. (26 February 2010). "Impact of alcohol on coronary heart disease in Indian men". Atherosclerosis. 210 (2): 531–535. doi:10.1016/j.atherosclerosis.2010.02.033. PMID 20226461.
- ^ IARC Alcohol causes more than half of all the premature deaths in Russian adults
- ^ Tjønneland, A.; Christensen, J.; Olsen, A.; Stripp, C.; Thomsen, BL.; Overvad, K.; Peeters, PH.; van Gils, CH.; et al. (May 2007). "Alcohol intake and breast cancer risk: the European Prospective Investigation into Cancer and Nutrition (EPIC)". Cancer Causes Control. 18 (4): 361–73. doi:10.1007/s10552-006-0112-9. PMID 17364225. S2CID 21762284.
- ^ Soerjomataram, I.; de Vries, E.; Coebergh, JW. (Sep 2009). "Did alcohol protect against death from breast cancer in Russia?". Lancet. 374 (9694): 975, author reply 975–6. doi:10.1016/S0140-6736(09)61657-3. PMID 19766875. S2CID 46431359.
- ^ "Alcohol Deaths: Rates stabilise in the UK". Statistics.gov.uk. Retrieved 2014-04-22.
- ^ BBC Alcohol 'kills one in 20 Scots' 30 June 2009
- ^ Sam Lister The price of alcohol: an extra 6,000 early deaths a year The Times, 19 October 2009
- ^ "'Optimal' levels of alcohol consumption for men and women at different ages, and the all-cause mortality attributable to drinking" (PDF). London: London School of Hygiene and Tropical Medicine. Technical report. 2000.
{{cite web}}: Unknown parameter|authors=ignored (help) - ^ "Alcohol and cancer". Cancer Research UK.
- ^ Centers for Disease Control and Prevention Alcohol and Public Health
- ^ McGinnis, J. Michael; Foege, William H. (1993). "Actual Causes of Death in the United States". JAMA. 270 (18): 2207–2212. doi:10.1001/jama.270.18.2207. PMID 8411605.
- ^ "Alcohol-Attributable Deaths and Years of Potential Life Lost — United States, 2001". Centers for Disease Control and Prevention. 2004-09-24.
- ^ Stockwell, Tim; Zhao, Jinhui; Panwar, Sapna; Roemer, Audra; Naimi, Timothy; Chikritzhs, Tanya (2016-03-01). "Do "Moderate" Drinkers Have Reduced Mortality Risk? A Systematic Review and Meta-Analysis of Alcohol Consumption and All-Cause Mortality". Journal of Studies on Alcohol and Drugs. 77 (2): 185–198. doi:10.15288/jsad.2016.77.185. ISSN 1937-1888. PMC 4803651. PMID 26997174.
- ^ Holahan, Charles J.; Schutte, Kathleen K.; Brennan, Penny L.; Holahan, Carole K.; Moos, Bernice S.; Moos, Rudolf H. (2010). "Late-Life Alcohol Consumption and 20-Year Mortality". Alcoholism: Clinical and Experimental Research. 34 (11): 1961–71. doi:10.1111/j.1530-0277.2010.01286.x. PMID 20735372.
- ^ Olsen A, Vantipalli MC, Lithgow GJ (2014-01-24). "Using Caenorhabditis elegans as a model for aging and age-related diseases". Ann. N. Y. Acad. Sci. 1067: 120–8. doi:10.1196/annals.1354.015. PMID 16803977. S2CID 45457944.
- ^ "Caenorhabditis elegans Battling Starvation Stress: Low Levels of Ethanol Prolong Lifespan in L1 Larvae". PLOS ONE. 7 (1): e29984. 2012-01-18. doi:10.1371/journal.pone.0029984. PMC 3261173. PMID 22279556.
{{cite journal}}: Unknown parameter|authors=ignored (help) - ^ Mennen LI, Balkau B, Vol S, Cacès E, Eschwège E (1 April 1999). "Fibrinogen: a possible link between alcohol consumption and cardiovascular disease? DESIR Study Group". Arterioscler Thromb Vasc Biol. 19 (4): 887–92. doi:10.1161/01.atv.19.4.887. PMID 10195914.
- ^ Paassilta M, Kervinen K, Rantala AO, et al. (14 February 1998). "Social alcohol consumption and low Lp(a) lipoprotein concentrations in middle aged Finnish men: population based study". BMJ. 316 (7131): 594–5. doi:10.1136/bmj.316.7131.594. PMC 28464. PMID 9518912.
- ^ Lacoste L, Hung J, Lam JY (January 2001). "Acute and delayed antithrombotic effects of alcohol in humans". Am J Cardiol. 87 (1): 82–5. doi:10.1016/S0002-9149(00)01277-7. PMID 11137839.
Pahor M, Guralnik JM, Havlik RJ, et al. (September 1996). "Alcohol consumption and risk of deep venous thrombosis and pulmonary embolism in older persons". J Am Geriatr Soc. 44 (9): 1030–7. doi:10.1111/j.1532-5415.1996.tb02933.x. PMID 8790226. S2CID 11553439.
Ridker, P., et al. Moderate alcohol intake may reduce risk of thrombosis. American Medical Association press release, September 22, 1994
Ridker, P. (1996). "The Pathogenesis of Atherosclerosis and Acute Thrombosis". In Manson, JoAnn E. (ed.). Prevention of myocardial infarction. Oxford [Oxfordshire]: Oxford University Press. ISBN 0-19-508582-5. - ^ Rimm, EB.; Williams, P.; Fosher, K.; Criqui, M.; Stampfer, MJ. (Dec 1999). "Moderate alcohol intake and lower risk of coronary heart disease: meta-analysis of effects on lipids and haemostatic factors". BMJ. 319 (7224): 1523–8. doi:10.1136/bmj.319.7224.1523. PMC 28294. PMID 10591709.
- ^ Brien Susan E, Ronksley Paul E, Turner Barbara J, Mukamal Kenneth J, Ghali William A (2011). "Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: systematic review and meta-analysis of interventional studies". BMJ. 342: d636. doi:10.1136/bmj.d636. PMC 3043110. PMID 21343206.
- ^ Albert, MA.; Glynn, RJ.; Ridker, PM. (Jan 2003). "Alcohol consumption and plasma concentration of C-reactive protein". Circulation. 107 (3): 443–7. doi:10.1161/01.CIR.0000045669.16499.EC. PMID 12551869. S2CID 323583.
- ^ Stewart, SH.; Mainous, AG.; Gilbert, G. (2002). "Relation between alcohol consumption and C-reactive protein levels in the adult US population" (PDF). J Am Board Fam Pract. 15 (6): 437–42. PMID 12463288.
- ^ Imhof, A.; Froehlich, M.; Brenner, H.; Boeing, H.; Pepys, MB.; Koenig, W. (Mar 2001). "Effect of alcohol consumption on systemic markers of inflammation". Lancet. 357 (9258): 763–7. doi:10.1016/S0140-6736(00)04170-2. PMID 11253971. S2CID 8046780.
- ^ Abdulla S (December 1997). "Is alcohol really good for you?". J R Soc Med. 90 (12): 651. doi:10.1177/014107689709001204. PMC 1296731. PMID 9496287.
- ^ Naimi TS, Brown DW, Brewer RD, et al. (May 2005). "Cardiovascular risk factors and confounders among nondrinking and moderate-drinking U.S. adults". Am J Prev Med. 28 (4): 369–73. doi:10.1016/j.amepre.2005.01.011. PMID 15831343.
- ^ Vogel, RA. (2002). "Alcohol, heart disease, and mortality: a review". Rev Cardiovasc Med. 3 (1): 7–13. PMID 12439349.
- ^ Sesso HD, Stampfer MJ, Rosner B, Hennekens CH, Manson JE, Gaziano JM (2000). "Seven-Year Changes in Alcohol Consumption and Subsequent Risk of Cardiovascular Disease in Men". Arch Intern Med. 160 (17): 2605–12. doi:10.1001/archinte.160.17.2605. PMID 10999974.
- ^ Estruch, Ramón; Ros, Emilio; Salas-Salvadó, Jordi; Covas, Maria-Isabel; Corella, Dolores; Arós, Fernando; Gómez-Gracia, Enrique; Ruiz-Gutiérrez, Valentina; Fiol, Miquel; Lapetra, José; Lamuela-Raventos, Rosa Maria; Serra-Majem, Lluís; Pintó, Xavier; Basora, Josep; Muñoz, Miguel Angel; Sorlí, José V.; Martínez, José Alfredo; Martínez-González, Miguel Angel; PREDIMED Study Investigators (2013). "Primary Prevention of Cardiovascular Disease with a Mediterranean Diet". New England Journal of Medicine. 368 (14): 1279–1290. doi:10.1056/NEJMoa1200303. hdl:2445/68456. PMID 23432189.
- ^ Camargo CA, Stampfer MJ, Glynn RJ, et al. (4 February 1997). "Prospective study of moderate alcohol consumption and risk of peripheral arterial disease in US male physicians". Circulation. 95 (3): 577–80. doi:10.1161/01.cir.95.3.577. PMID 9024142.
- ^ Vliegenthart R, Geleijnse JM, Hofman A, et al. (February 2002). "Alcohol consumption and risk of peripheral arterial disease: the Rotterdam study". Am J Epidemiol. 155 (4): 332–8. doi:10.1093/aje/155.4.332. PMID 11836197.
- ^ Mingardi R, Avogaro A, Noventa F, et al. (1997). "Alcohol intake is no longer associated with a lower prevalence of peripheral vascular disease in non-insulin dependent diabetic women". Nutrition Metabolism and Cardiovascular Disease. 7 (4): 301–8.
- ^ Djoussé L, Levy D, Murabito JM, Cupples LA, Ellison RC (19 December 2000). "Alcohol consumption and risk of intermittent claudication in the Framingham Heart Study". Circulation. 102 (25): 3092–7. doi:10.1161/01.cir.102.25.3092. PMID 11120700. S2CID 1586122.
- ^ Muntwyler J, Hennekens CH, Buring JE, Gaziano JM (December 1998). "Mortality and light to moderate alcohol consumption after myocardial infarction". Lancet. 352 (9144): 1882–5. doi:10.1016/S0140-6736(98)06351-X. PMID 9863785. S2CID 54365788.
- ^ Mukamal KJ, Maclure M, Muller JE, Sherwood JB, Mittleman MA (April 2001). "Prior alcohol consumption and mortality following acute myocardial infarction". JAMA. 285 (15): 1965–70. doi:10.1001/jama.285.15.1965. PMID 11308432.
- ^ "Alcohol helps reduce damage after heart attacks". Newswise.com. 2004-08-30. Retrieved 2014-04-22.
- ^ Djoussé L, Gaziano JM (April 2008). "Alcohol consumption and heart failure: a systematic review". Curr Atheroscler Rep. 10 (2): 117–20. doi:10.1007/s11883-008-0017-z. PMC 2365733. PMID 18417065.
- ^ Kloner RA, Rezkalla SH (September 2007). "To drink or not to drink? That is the question". Circulation. 116 (11): 1306–17. doi:10.1161/CIRCULATIONAHA.106.678375. PMID 17846344.
- ^ Saremi A, Arora R (2008). "The cardiovascular implications of alcohol and red wine". Am J Ther. 15 (3): 265–77. doi:10.1097/MJT.0b013e3180a5e61a. PMID 18496264. S2CID 7243756.
- ^ Awtry, EH.; Philippides, GJ. (2010). "Alcoholic and cocaine-associated cardiomyopathies". Prog Cardiovasc Dis. 52 (4): 289–99. doi:10.1016/j.pcad.2009.11.004. PMID 20109599.
- ^ Savage D, Lindenbaum J (1986). "Anemia in alcoholics". Medicine (Baltimore). 65 (5): 322–38. doi:10.1097/00005792-198609000-00005. PMID 3747828. S2CID 25790752.
- ^ Larsson, Susanna C.; Drca, Nikola; Wolk, Alicja (July 2014). "Alcohol Consumption and Risk of Atrial Fibrillation". Journal of the American College of Cardiology. 64 (3): 281–289. doi:10.1016/j.jacc.2014.03.048. PMID 25034065.
- ^ Panza F, Capurso C, D'Introno A, et al. (2008). "Vascular risk factors, alcohol intake, and cognitive decline". J Nutr Health Aging. 12 (6): 376–81. doi:10.1007/BF02982669. PMID 18548174. S2CID 3123226.
- ^ Panza, F.; Capurso, C.; D'Introno, A.; Colacicco, AM.; Frisardi, V.; Lorusso, M.; Santamato, A.; Seripa, D.; et al. (May 2009). "Alcohol drinking, cognitive functions in older age, predementia, and dementia syndromes". J Alzheimers Dis. 17 (1): 7–31. doi:10.3233/JAD-2009-1009. PMID 19494429.
- ^ Verbaten, MN. (Apr 2009). "Chronic effects of low to moderate alcohol consumption on structural and functional properties of the brain: beneficial or not?". Hum Psychopharmacol. 24 (3): 199–205. doi:10.1002/hup.1022. PMID 19330800. S2CID 205924421.
- ^ Bleich S, Bleich K, Kropp S, et al. (2001). "Moderate alcohol consumption in social drinkers raises plasma homocysteine levels: a contradiction to the 'French Paradox'?". Alcohol Alcohol. 36 (3): 189–92. doi:10.1093/alcalc/36.3.189. PMID 11373253.
- ^ Bleich S, Carl M, Bayerlein K, et al. (March 2005). "Evidence of increased homocysteine levels in alcoholism: the Franconian alcoholism research studies (FARS)". Alcohol. Clin. Exp. Res. 29 (3): 334–6. doi:10.1097/01.alc.0000156083.91214.59. PMID 15770107.
- ^ Bleich S, Degner D, Bandelow B, von Ahsen N, Rüther E, Kornhuber J (August 2000). "Plasma homocysteine is a predictor of alcohol withdrawal seizures". NeuroReport. 11 (12): 2749–52. doi:10.1097/00001756-200008210-00028. PMID 10976956. S2CID 20270541.
- ^ Bleich S, Bandelow B, Javaheripour K, et al. (January 2003). "Hyperhomocysteinemia as a new risk factor for brain shrinkage in patients with alcoholism". Neurosci. Lett. 335 (3): 179–82. doi:10.1016/S0304-3940(02)01194-1. PMID 12531462. S2CID 33032529.
- ^ Wilhelm J, Bayerlein K, Hillemacher T, et al. (March 2006). "Short-term cognition deficits during early alcohol withdrawal are associated with elevated plasma homocysteine levels in patients with alcoholism". J Neural Transm. 113 (3): 357–63. doi:10.1007/s00702-005-0333-1. PMID 15997414. S2CID 11980558.
- ^ Di Castelnuovo, A.; Costanzo, S.; di Giuseppe, R.; de Gaetano, G.; Iacoviello, L. (Sep 2009). "Alcohol consumption and cardiovascular risk: mechanisms of action and epidemiologic perspectives". Future Cardiol. 5 (5): 467–77. doi:10.2217/fca.09.36. PMID 19715411.
- ^ Klatsky, AL. (May 2009). "Alcohol and cardiovascular diseases". Expert Rev Cardiovasc Ther. 7 (5): 499–506. doi:10.1586/erc.09.22. PMID 19419257. S2CID 23782870.
- ^ Galimanis, A.; Mono, ML.; Arnold, M.; Nedeltchev, K.; Mattle, HP. (Feb 2009). "Lifestyle and stroke risk: a review". Current Opinion in Neurology. 22 (1): 60–8. doi:10.1097/WCO.0b013e32831fda0e. PMID 19155763. S2CID 22619761.
- ^ O'Keefe, JH.; Bybee, KA.; Lavie, CJ. (Sep 2007). "Alcohol and cardiovascular health: the razor-sharp double-edged sword". J Am Coll Cardiol. 50 (11): 1009–14. doi:10.1016/j.jacc.2007.04.089. PMID 17825708.
- ^ "Stroke Risk Reduction - Alcohol Use - National Stroke Association". Stroke.org. Retrieved 2014-04-22.
- ^ Emberson, JR.; Bennett, DA. (2006). "Effect of alcohol on risk of coronary heart disease and stroke: causality, bias, or a bit of both?". Vasc Health Risk Manag. 2 (3): 239–49. doi:10.2147/vhrm.2006.2.3.239. PMC 1993990. PMID 17326330.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Neiman, J. (Oct 1998). "Alcohol as a risk factor for brain damage: neurologic aspects". Alcohol Clin Exp Res. 22 (7 Suppl): 346S–351S. doi:10.1111/j.1530-0277.1998.tb04389.x. PMID 9799959.
- ^ Heffernan, TM. (Jan 2008). "The impact of excessive alcohol use on prospective memory: a brief review". Curr Drug Abuse Rev. 1 (1): 36–41. doi:10.2174/1874473710801010036. PMID 19630703.
- ^ Pierucci-Lagha A, Derouesné C (December 2003). "Alcoholism and aging. 2. Alcoholic dementia or alcoholic cognitive impairment?". Psychol Neuropsychiatr Vieil (in French). 1 (4): 237–49. PMID 15683959.
- ^ Peters R, Peters J, Warner J, Beckett N, Bulpitt C (September 2008). "Alcohol, dementia and cognitive decline in the elderly: a systematic review". Age Ageing. 37 (5): 505–12. doi:10.1093/ageing/afn095. PMID 18487267.
- ^ Cooper Claudia, Bebbington Paul, Meltzer Howard, Jenkins Rachel, Brugha Traolach, Lindesay James, Livingston Gill (2009). "Alcohol in moderation, premorbid intelligence and cognition In Older Adults: results from the Psychiatric Morbidity Survey". J Neurol Neurosurg Psychiatry. 80 (11): 1236–1239. doi:10.1136/jnnp.2008.163964. PMID 19620140. S2CID 9226226.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Peters, R; Peters, J; Warner, J; Beckett, N; Bulpitt, C (September 2008). "Alcohol, dementia and cognitive decline in the elderly: a systematic review". Age and Ageing. 37 (5): 505–12. doi:10.1093/ageing/afn095. PMID 18487267.
- ^ Martin PR, Singleton CK, Hiller-Sturmhöfel S (2003). "The role of thiamine deficiency in alcoholic brain disease". Alcohol Res Health. 27 (2): 134–42. PMC 6668887. PMID 15303623.
- ^ Butters N (1981). "The Wernicke-Korsakoff syndrome: a review of psychological, neuropathological and etiological factors". Curr Alcohol. 8: 205–32. PMID 6806017.
- ^ Jeffrey E Kelsey; D Jeffrey Newport & Charles B Nemeroff (2006). "Alcohol Use Disorders". Principles of Psychopharmacology for Mental Health Professionals. Wiley-Interscience. pp. 196–197. ISBN 978-0-471-79462-2.
- ^ Merle A. Carter & Edward Bernstein (2005). "Acute and Chronic Alcohol Intoxication". In Elizabeth Mitchell & Ron Medzon (eds.). Introduction to Emergency Medicine. Lippincott Williams & Wilkins. p. 272. ISBN 978-0-7817-3200-0.
- ^
Bain PG, Findley LJ, Thompson PD, et al. (August 1994). "A study of hereditary essential tremor". Brain. 117 (Pt 4): 805–24. doi:10.1093/brain/117.4.805. PMID 7922467.
Lou JS, Jankovic J (February 1991). "Essential tremor: clinical correlates in 350 patients". Neurology. 41 (2 (Pt 1)): 234–8. doi:10.1212/WNL.41.2_Part_1.234. PMID 1992367. S2CID 20531450.
Wasielewski PG, Burns JM, Koller WC (1998). "Pharmacologic treatment of tremor". Mov Disord. 13 (Suppl 3): 90–100. doi:10.1002/mds.870131316. PMID 9827602. S2CID 21004382.
Boecker H, Wills AJ, Ceballos-Baumann A, et al. (May 1996). "The effect of ethanol on alcohol-responsive essential tremor: a positron emission tomography study". Annals of Neurology. 39 (5): 650–8. doi:10.1002/ana.410390515. PMID 8619551. S2CID 11083928.
"Setting a steady course for benign essential tremor". Johns Hopkins Med Lett Health After 50. 11 (10): 3. December 1999. PMID 10586714. - ^ Mostile, G.; Jankovic, J. (2010). "Alcohol in essential tremor and other movement disorders". Movement Disorders. 25 (14): 2274–2284. doi:10.1002/mds.23240. PMID 20721919. S2CID 39981956.
- ^ Iseri, P. K.; Karson, A.; Gullu, K. M.; Akman, O.; Kokturk, S.; Yardýmoglu, M.; Erturk, S.; Ates, N. (2011). "The effect of memantine in harmaline-induced tremor and neurodegeneration". Neuropharmacology. 61 (4): 715–723. doi:10.1016/j.neuropharm.2011.05.015. PMID 21640732. S2CID 16296043.
- ^ Miwa, H. (2007). "Rodent models of tremor". The Cerebellum. 6 (1): 66–72. doi:10.1080/14734220601016080. PMID 17366267. S2CID 24179439.
- ^ Lee-chiong, Teofilo (24 April 2008). Sleep Medicine: Essentials and Review. Oxford University Press, USA. p. 105. ISBN 978-0-19-530659-0.
- ^ Fergusson DM, Boden JM, Horwood LJ (March 2009). "Tests of causal links between alcohol abuse or dependence and major depression". Arch. Gen. Psychiatry. 66 (3): 260–6. doi:10.1001/archgenpsychiatry.2008.543. PMID 19255375.
- ^ Chignon JM, Cortes MJ, Martin P, Chabannes JP (1998). "Tentative de suicide et dépendance alcoolique : résultats d'une enquête épidémiologique" [Attempted suicide and alcohol dependence: results of an epidemiologic survey]. Encephale (in French). 24 (4): 347–54. PMID 9809240.
- ^ Ayd, Frank J. (31 May 2000). Lexicon of psychiatry, neurology, and the neurosciences. Philadelphia: Lippincott-Williams Wilkins. p. 349. ISBN 978-0-7817-2468-5.
- ^ Appleby, Louis; Duffy, David; Ryan, Tony (25 Aug 2004). New Approaches to Preventing Suicide: A Manual For Practitioners. Jessica Kingsley Publishers. pp. 31–32. ISBN 978-1-84310-221-2.
- ^ Uekermann J, Daum I (May 2008). "Social cognition in alcoholism: a link to prefrontal cortex dysfunction?". Addiction. 103 (5): 726–35. doi:10.1111/j.1360-0443.2008.02157.x. PMID 18412750.
- ^ Jasova D, Bob P, Fedor-Freybergh P (December 2007). "Alcohol craving, limbic irritability, and stress". Med Sci Monit. 13 (12): CR543–7. PMID 18049433. Retrieved 2008-05-13.
- ^ Marinkovic K; Oscar-Berman M; Urban T; O'Reilly CE; Howard JA; Sawyer K; Harris GJ (November 2009). "Alcoholism and dampened temporal limbic activation to emotional faces". Alcohol Clin Exp Res. 33 (11): 1880–92. doi:10.1111/j.1530-0277.2009.01026.x. PMC 3543694. PMID 19673745.
- ^ Wetterling T; Junghanns K (December 2000). "Psychopathology of alcoholics during withdrawal and early abstinence". Eur Psychiatry. 15 (8): 483–8. doi:10.1016/S0924-9338(00)00519-8. PMID 11175926. S2CID 24094651.
- ^ Cowley DS (24 January 1992). "Alcohol abuse, substance abuse, and panic disorder". Am J Med. 92 (1A): 41S–8S. doi:10.1016/0002-9343(92)90136-Y. PMID 1346485.
- ^ Cosci F; Schruers KR; Abrams K; Griez EJ (June 2007). "Alcohol use disorders and panic disorder: a review of the evidence of a direct relationship". J Clin Psychiatry. 68 (6): 874–80. doi:10.4088/JCP.v68n0608. PMID 17592911.
- ^ a b Alcohol-Related Psychosis at eMedicine
- ^ Tien AY, Anthony JC (August 1990). "Epidemiological analysis of alcohol and drug use as risk factors for psychotic experiences". J. Nerv. Ment. Dis. 178 (8): 473–80. doi:10.1097/00005053-199017880-00001. PMID 2380692.
- ^ "A wine a day ... keeps the psychiatrist away? Light drinking linked to lower risk of depression". ScienceDaily. Retrieved 2014-04-22.
- ^ Terra MB, Figueira I, Barros HM (August 2004). "Impact of alcohol intoxication and withdrawal syndrome on social phobia and panic disorder in alcoholic inpatients". Rev Hosp Clin Fac Med Sao Paulo. 59 (4): 187–92. doi:10.1590/S0041-87812004000400006. PMID 15361983.
- ^ Cohen SI (February 1995). "Alcohol and benzodiazepines generate anxiety, panic and phobias". J R Soc Med. 88 (2): 73–7. PMC 1295099. PMID 7769598.
- ^ McClure EA, Gipson CD, Malcolm RJ, Kalivas PW, Gray KM (2014). "Potential role of N-acetylcysteine in the management of substance use disorders". CNS Drugs. 28 (2): 95–106. doi:10.1007/s40263-014-0142-x. PMC 4009342. PMID 24442756.
- ^ Cordain L, Bryan ED, Melby CL, Smith MJ (1 April 1997). "Influence of moderate daily wine consumption on body weight regulation and metabolism in healthy free-living males". J Am Coll Nutr. 16 (2): 134–9. doi:10.1080/07315724.1997.10718663. PMID 9100213. Archived from the original on 23 February 2007.
- ^ Arif AA, Rohrer JE (2005). "Patterns of alcohol drinking and its association with obesity: data from the Third National Health and Nutrition Examination Survey, 1988-1994". BMC Public Health. 5 (1): 126. doi:10.1186/1471-2458-5-126. PMC 1318457. PMID 16329757.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Bode C, Bode JC (1997). "Alcohol's role in gastrointestinal tract disorders" (PDF). Alcohol Health Res World. 21 (1): 76–83. PMC 6826790. PMID 15706765.
- ^ Freiberg MS, Cabral HJ, Heeren TC, Vasan RS, Curtis Ellison R (December 2004). "Alcohol consumption and the prevalence of the Metabolic Syndrome in the US.: a cross-sectional analysis of data from the Third National Health and Nutrition Examination Survey". Diabetes Care. 27 (12): 2954–9. doi:10.2337/diacare.27.12.2954. PMID 15562213.
- ^ Yoon YS, Oh SW, Baik HW, Park HS, Kim WY (1 July 2004). "Alcohol consumption and the metabolic syndrome in Korean adults: the 1998 Korean National Health and Nutrition Examination Survey". Am. J. Clin. Nutr. 80 (1): 217–24. doi:10.1093/ajcn/80.1.217. PMID 15213051.
- ^ La Vecchia C, Decarli A, Ferraroni M, Negri E (September 1994). "Alcohol drinking and prevalence of self-reported gallstone disease in the 1983 Italian National Health Survey". Epidemiology. 5 (5): 533–6. JSTOR 3702209. PMID 7986868.
- ^ Leitzmann MF, Giovannucci EL, Stampfer MJ, et al. (May 1999). "Prospective study of alcohol consumption patterns in relation to symptomatic gallstone disease in men". Alcohol Clin Exp Res. 23 (5): 835–41. doi:10.1111/j.1530-0277.1999.tb04191.x. PMID 10371403.
- ^ Sahi T, Paffenbarger RS, Hsieh CC, Lee IM (1 April 1998). "Body mass index, cigarette smoking, and other characteristics as predictors of self-reported, physician-diagnosed gallbladder disease in male college alumni". Am J Epidemiol. 147 (7): 644–51. doi:10.1093/oxfordjournals.aje.a009505. PMID 9554603.
- ^ Simon JA, Grady D, Snabes MC, Fong J, Hunninghake DB (March 1998). "Ascorbic acid supplement use and the prevalence of gallbladder disease. Heart & Estrogen-Progestin Replacement Study (HERS) Research Group". J Clin Epidemiol. 51 (3): 257–65. doi:10.1016/S0895-4356(97)80280-6. PMID 9495691.
- ^ a b Barve A, Khan R, Marsano L, Ravindra KV, McClain C (2008). "Treatment of alcoholic liver disease" (PDF). Ann Hepatol. 7 (1): 5–15. doi:10.1016/S1665-2681(19)31883-6. PMID 18376362.
- ^ Fehér J, Lengyel G (December 2008). "Silymarin in the treatment of chronic liver diseases: past and future". Orv Hetil (in Hungarian). 149 (51): 2413–8. doi:10.1556/OH.2008.28519. PMID 19073452.
- ^ Voigt MD (February 2005). "Alcohol in hepatocellular cancer". Clin Liver Dis. 9 (1): 151–69. doi:10.1016/j.cld.2004.10.003. PMID 15763234.
- ^ Morgan TR, Mandayam S, Jamal MM (November 2004). "Alcohol and hepatocellular carcinoma". Gastroenterology. 127 (5 Suppl 1): S87–96. doi:10.1053/j.gastro.2004.09.020. PMID 15508108.
- ^ Frossard JL, Steer ML, Pastor CM (January 2008). "Acute pancreatitis". Lancet. 371 (9607): 143–52. doi:10.1016/S0140-6736(08)60107-5. PMID 18191686.
- ^ Bachmann K, Mann O, Izbicki JR, Strate T (November 2008). "Chronic pancreatitis--a surgeons' view". Med. Sci. Monit. 14 (11): RA198–205. PMID 18971885.
- ^ Nair RJ, Lawler L, Miller MR (December 2007). "Chronic pancreatitis". Am Fam Physician. 76 (11): 1679–88. PMID 18092710.
- ^ Tattersall SJ, Apte MV, Wilson JS (July 2008). "A fire inside: current concepts in chronic pancreatitis". Intern Med J. 38 (7): 592–8. doi:10.1111/j.1445-5994.2008.01715.x. PMID 18715303. S2CID 205502466.
- ^ Hirvonen T, Pietinen P, Virtanen M, Albanes D, Virtamo J (15 July 1999). "Nutrient intake and use of beverages and the risk of kidney stones among male smokers". Am J Epidemiol. 150 (2): 187–94. doi:10.1093/oxfordjournals.aje.a009979. PMID 10412964.
- ^ Soucie JM, Coates RJ, McClellan W, Austin H, Thun M (1 March 1996). "Relation between geographic variability in kidney stones prevalence and risk factors for stones". Am J Epidemiol. 143 (5): 487–95. doi:10.1093/oxfordjournals.aje.a008769. PMID 8610664.
- ^ Curhan GC, Willett WC, Rimm EB, Spiegelman D, Stampfer MJ (1 February 1996). "Prospective study of beverage use and the risk of kidney stones". Am J Epidemiol. 143 (3): 240–7. doi:10.1093/oxfordjournals.aje.a008734. PMID 8561157.
- ^ Curhan GC, Willett WC, Speizer FE, Stampfer MJ (1 April 1998). "Beverage use and risk for kidney stones in women". Annals of Internal Medicine. 128 (7): 534–40. doi:10.7326/0003-4819-128-7-199804010-00003. PMID 9518397. S2CID 43163872.
- ^ Taniguchi N, Kaneko S (November 1997). "Alcoholic effect on male sexual function". Nippon Rinsho (in Japanese). 55 (11): 3040–4. PMID 9396310.
- ^ Yoshitsugu M, Ihori M (November 1997). "Endocrine disturbances in liver cirrhosis--focused on sex hormones". Nippon Rinsho (in Japanese). 55 (11): 3002–6. PMID 9396303.
- ^ Fentiman, IS.; Fourquet, A.; Hortobagyi, GN. (Feb 2006). "Male breast cancer". Lancet. 367 (9510): 595–604. doi:10.1016/S0140-6736(06)68226-3. PMID 16488803. S2CID 21618414.
- ^ Gavaler, JS. (1998). "Alcoholic beverages as a source of estrogens". Alcohol Health Res World. 22 (3): 220–7. PMC 6761902. PMID 15706799.
- ^ a b Weiss, JR.; Moysich, KB.; Swede, H. (Jan 2005). "Epidemiology of male breast cancer". Cancer Epidemiol Bio-markers Prev. 14 (1): 20–6. doi:10.1158/1055-9965.20.14.1. PMID 15668471.
- ^ Boffetta, P.; Hashibe, M. (Feb 2006). "Alcohol and cancer". Lancet Oncol. 7 (2): 149–56. doi:10.1016/S1470-2045(06)70577-0. PMID 16455479.
- ^ Baliunas DO, Taylor BJ, Irving H, Roerecke M, Patra J, Mohapatra S, Rehm J (2009). "Alcohol as a Risk Factor for Type 2 Diabetes". Diabetes Care. 32 (11): 2123–32. doi:10.2337/dc09-0227. PMC 2768203. PMID 19875607.
- ^ Carlsson S, Hammar N, Grill V, Kaprio J (October 2003). "Alcohol consumption and the incidence of type 2 diabetes: a 20-year follow-up of the Finnish twin cohort study". Diabetes Care. 26 (10): 2785–90. doi:10.2337/diacare.26.10.2785. PMID 14514580.
- ^ Hong1 J, Smith R R, Harvey A E, Núñez N P (2009). "Alcohol consumption promotes insulin sensitivity without affecting body fat levels". International Journal of Obesity. 33 (2): 197–203. doi:10.1038/ijo.2008.266. PMID 19125162. S2CID 8824592.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: numeric names: authors list (link) - ^ Star VL, Hochberg MC (February 1993). "Prevention and management of gout". Drugs. 45 (2): 212–22. doi:10.2165/00003495-199345020-00004. PMID 7681372. S2CID 36034581.
- ^ Eggebeen AT (September 2007). "Gout: an update". Am Fam Physician. 76 (6): 801–8. PMID 17910294.
- ^ http://arc.org.uk/arthinfo/patpubs/6033/6033.asp
- ^ Myllykangas-Luosujärvi R, Aho K, Kautiainen H, Hakala M (January 2000). "Reduced incidence of alcohol related deaths in subjects with rheumatoid arthritis". Ann. Rheum. Dis. 59 (1): 75–6. doi:10.1136/ard.59.1.75. PMC 1752983. PMID 10627433.
- ^ Nagata C, Fujita S, Iwata H, et al. (May 1995). "Systemic lupus erythematosus: a case-control epidemiologic study in Japan". Int J Dermatol. 34 (5): 333–7. doi:10.1111/j.1365-4362.1995.tb03614.x. PMID 7607794. S2CID 24940881.
- ^ Aho K, Heliövaara M (December 1993). "Alcohol, androgens and arthritis". Ann. Rheum. Dis. 52 (12): 897. doi:10.1136/ard.52.12.897-b. PMC 1005228. PMID 8311545.
- ^ Hardy CJ, Palmer BP, Muir KR, Sutton AJ, Powell RJ (August 1998). "Smoking history, alcohol consumption, and systemic lupus erythematosus: a case-control study". Ann. Rheum. Dis. 57 (8): 451–5. doi:10.1136/ard.57.8.451. PMC 1752721. PMID 9797548.
- ^ Källberg H, Jacobsen S, Bengtsson C, et al. (July 2008). "Alcohol consumption is associated with decreased risk of rheumatoid arthritis; Results from two Scandinavian case-control studies". Ann. Rheum. Dis. 68 (2): 222–7. doi:10.1136/ard.2007.086314. PMC 2937278. PMID 18535114.
- ^ Jonsson IM, Verdrengh M, Brisslert M, et al. (January 2007). "Ethanol prevents development of destructive arthritis". Proc Natl Acad Sci USA. 104 (1): 258–63. doi:10.1073/pnas.0608620104. PMC 1765445. PMID 17185416.
- ^ Myllykangas-Luosujärvi R, Aho K, Kautiainen H, Hakala M (January 2000). "Reduced incidence of alcohol related deaths in subjects with rheumatoid arthritis". Ann. Rheum. Dis. 59 (1): 75–6. doi:10.1136/ard.59.1.75. PMC 1752983. PMID 10627433.
- ^ Voigt LF, Koepsell TD, Nelson JL, Dugowson CE, Daling JR (September 1994). "Smoking, obesity, alcohol consumption, and the risk of rheumatoid arthritis". Epidemiology. 5 (5): 525–32. PMID 7986867.
- ^ Siris ES, Miller PD, Barrett-Connor E, et al. (December 2001). "Identification and fracture outcomes of undiagnosed low bone mineral density in postmenopausal women: results from the National Osteoporosis Risk Assessment". JAMA. 286 (22): 2815–22. doi:10.1001/jama.286.22.2815. PMID 11735756.
- ^ Rapuri PB, Gallagher JC, Balhorn KE, Ryschon KL (1 November 2000). "Alcohol intake and bone metabolism in elderly women". Am. J. Clin. Nutr. 72 (5): 1206–13. doi:10.1093/ajcn/72.5.1206. PMID 11063451.
- ^ Holbrook TL, Barrett-Connor E (June 1993). "A prospective study of alcohol consumption and bone mineral density". BMJ. 306 (6891): 1506–9. doi:10.1136/bmj.306.6891.1506. PMC 1677960. PMID 8518677.
- ^ a b Ronis, MJ.; Wands, JR.; Badger, TM.; de la Monte, SM.; Lang, CH.; Calissendorff, J. (Aug 2007). "Alcohol-induced disruption of endocrine signaling". Alcohol Clin Exp Res. 31 (8): 1269–85. doi:10.1111/j.1530-0277.2007.00436.x. PMID 17559547.
- ^ Peer, KS.; Newsham, KR. (2005). "A case study on osteoporosis in a male athlete: looking beyond the usual suspects". Orthop Nurs. 24 (3): 193–9, quiz 200–1. doi:10.1097/00006416-200505000-00007. PMID 15928528. S2CID 23377405.
- ^ Kostović K, Lipozencić J (2004). "Skin diseases in alcoholics". Acta Dermatovenerol Croat. 12 (3): 181–90. PMID 15369644.
- ^ Qureshi Abrar A., Dominguez Patrick L., Choi Hyon K., Han Jiali, Curhan Gary (2010). "Alcohol Intake and Risk of Incident Psoriasis in US Women: A Prospective Study". Arch Dermatology. 146 (12): 1364–1369. doi:10.1001/archdermatol.2010.204. PMC 3017376. PMID 20713772.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Brenner H, Rothenbacher D, Bode G, Adler G (6 December 1997). "Relation of smoking and alcohol and coffee consumption to active Helicobacter pylori infection: cross sectional study". BMJ. 315 (7121): 1489–92. doi:10.1136/bmj.315.7121.1489. PMC 2127930. PMID 9420488.
- ^ Aldoori WH, Giovannucci EL, Stampfer MJ, Rimm EB, Wing AL, Willett WC (July 1997). "A prospective study of alcohol, smoking, caffeine, and the risk of duodenal ulcer in men". Epidemiology. 8 (4): 420–4. doi:10.1097/00001648-199707000-00012. PMID 9209857. S2CID 20485605.
- ^ Cohen S, Tyrrell DA, Russell MA, Jarvis MJ, Smith AP (September 1993). "Smoking, alcohol consumption, and susceptibility to the common cold". Am J Public Health. 83 (9): 1277–83. doi:10.2105/AJPH.83.9.1277. PMC 1694990. PMID 8363004.
- ^ Takkouche B, Regueira-Méndez C, García-Closas R, Figueiras A, Gestal-Otero JJ, Hernán MA (May 2002). "Intake of wine, beer, and spirits and the risk of clinical common cold". Am J Epidemiol. 155 (9): 853–8. doi:10.1093/aje/155.9.853. PMID 11978590.
- ^ IARC Monographs on the Evaluation of Carcinogenic Risks to Humans: Volume 44 Alcohol Drinking: Summary of Data Reported and Evaluation Archived 2013-06-26 at WebCite
- ^ National Toxicology Program Alcoholic Beverage Consumption: Known to be a human carcinogen Archived 2010-03-04 at WebCite First listed in the Ninth Report on Carcinogens (2000)(PDF)
- ^ Boffetta P, Hashibe M, La Vecchia C, Zatonski W, Rehm J (August 2006). "The burden of cancer attributable to alcohol drinking". International Journal of Cancer. 119 (4): 884–7. doi:10.1002/ijc.21903. PMID 16557583. S2CID 14938863.
- ^ BBC News Drinking over recommended limit 'raises cancer risk' 8 April 2011
- ^ Schütze Madlen; et al. (2011). "Alcohol attributable burden of incidence of cancer in eight European countries based on results from prospective cohort study". BMJ. 342: d1584. doi:10.1136/bmj.d1584. PMC 3072472. PMID 21474525.
{{cite journal}}: Explicit use of et al. in:|author=(help) - ^ WCRF World Cancer Research Fund / American Institute for Cancer Research. Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective. Washington DC: AICR, 2007
- ^ Homann N, Stickel F, König IR, et al. (2006). "Alcohol dehydrogenase 1C*1 allele is a genetic marker for alcohol-associated cancer in heavy drinkers". International Journal of Cancer. 118 (8): 1998–2002. doi:10.1002/ijc.21583. PMID 16287084. S2CID 11716548.
- ^ Seitz HK, Stickel F (Aug 2007). "Molecular mechanisms of alcohol-mediated carcinogenesis" (PDF). Nat Rev Cancer. 7 (8): 599–612. doi:10.1038/nrc2191. PMID 17646865. S2CID 3231314.
- ^ Brooks P, Theruvathu J, Cho CH, Purohit V (2006). "Acetaldehyde-DNA Adducts: Implications for the Molecular Mechanism of Alcohol-Related Carcinogenesis". Alcohol, Tobacco and Cancer. 2006: 78–94. doi:10.1159/000095017. ISBN 3-8055-8107-6.
- ^ Ulleland CN (May 1972). "The offspring of alcoholic mothers". Annals of the New York Academy of Sciences. 197: 167–9. doi:10.1111/j.1749-6632.1972.tb28142.x. PMID 4504588. S2CID 84514766.
- ^ Abel EL, Sokol RJ (January 1987). "Incidence of foetal alcohol syndrome and economic impact of FAS-related anomalies". Drug Alcohol Depend. 19 (1): 51–70. doi:10.1016/0376-8716(87)90087-1. PMID 3545731.
External links
[edit]- Alcohol and Health: Current Evidence. Boston University/National Institute on Alcohol Abuse and Alcoholism Journal
- Alcohol-Attributable Deaths Report, United States 2001
- Health-EU Portal Alcohol and Health in the EU
- Alcohol is linked to high blood pressure, cancers and heart attack (NHS)
