Talk:Ectopic pregnancy
| This article is rated B-class on Wikipedia's content assessment scale. It is of interest to the following WikiProjects: | |||||||||||||||||||||||||||
| |||||||||||||||||||||||||||
 | Ideal sources for Wikipedia's health content are defined in the guideline Wikipedia:Identifying reliable sources (medicine) and are typically review articles. Here are links to possibly useful sources of information about Ectopic pregnancy.
|
Wiki Education Foundation-supported course assignment
[edit]![]() This article was the subject of a Wiki Education Foundation-supported course assignment, between 1 July 2019 and 23 August 2019. Further details are available on the course page. Student editor(s): Sara.F.Shaikh, Michaelfashola, Ashleyher, ManuelSeraydarian.
This article was the subject of a Wiki Education Foundation-supported course assignment, between 1 July 2019 and 23 August 2019. Further details are available on the course page. Student editor(s): Sara.F.Shaikh, Michaelfashola, Ashleyher, ManuelSeraydarian.
Above undated message substituted from Template:Dashboard.wikiedu.org assignment by PrimeBOT (talk) 20:08, 16 January 2022 (UTC)
Heading
[edit]I tried to find an academic reference for the Montreal 2003 case, but this was unsuccesful link. JFW | T@lk 12:20, 10 July 2005 (UTC)
"Viability of Pregnancies" heading?
[edit]I don't know if there is some kind of template or standard for medical articles, but I think it would be helpful if there was a heading for "Viability of Pregnancy". Whether or not one could actually deliver an "ectopically" implanted fetus was the first question I had when arriving at this article, especially with the arresting graphic at the top of the page ([1]). kostmo 08:04, 10 February 2007 (UTC)
This graphic is a fanciful depiction classical of the time it was created. The reality is that one does not see a nice fetus as shown, at most it is a little scrap of tissue, or just blood clot. I hope this helps your understanding. JustAnMD 03:49, 6 April 2007 (UTC)
- Do you mean as in a parasitic twin, or as in not developed much? Can it be called a fetus if it's a blood clot? Junulo asked this question at 20:24, 7 November 2007 (UTC).
Good question. One rarely finds more than a blood clot, or the remains of the sac. The analogy with miscarraige is strong; the fetus being abnormal and not developing. ```` —Preceding unsigned comment added by JustAnMD (talk • contribs) 15:18, 10 November 2007 (UTC)
This story is apocryphal and does not merit inclusion in a serious discussion. Without strong and exact references, it should be removed. "Cases have been known where a tubal pregnancy burst and the pregnancy continued with the growing placenta attaching to internal organs. In one such case the pregnancy after this had no amniotic sac and the baby was loose among its mother's intestines; laparotomy rescued the baby, and it lived." I plan to allow time for response before removing it. ```` —Preceding unsigned comment added by JustAnMD (talk • contribs) 15:23, 10 November 2007 (UTC)
University of Iowa
[edit]I have removed this recent unsourced addition for now. It's just an anecdote and needs a citation. The style is not encyclopedic and it would need cleanup if added.
- One such case was in Iowa, at the University of Iowa Hospitals, back in the 50s. To deliver an extra-uterine child via laprarotomy is something more than a one-in-a-million event. To hear a good emergency room nurse relate the story is magical: the whole of University of Iowa baby-deliverers were there in the room, observing and assisting at a majical event.
--Tony Sidaway 12:27, 13 March 2006 (UTC)
Catholic view
[edit]The Catholic view may belong in a larger section on the ethics of surgery in such cases. I have removed the recently added section because it is anecdotal and the writer does not seem to have even seen a good source ("apparently"). --Tony Sidaway 12:27, 13 March 2006 (UTC)
Obtaining accurate figures for the rates of ectopic pregnacy is impossible, since this is one of the few medical grounds on which a Catholic woman can have a pregnancy terminated : at one stage in the late 70s/early 80's, the rates of recorded ectopic pregnancies in the Republic of Ireland and Spain were so high, medical experts formed the opinion that there must be a genetic disposition towards them- the true reason was of course, falisfication of medical records.
- Is there a way to save both the mother and child? —Preceding unsigned comment added by Junulo (talk • contribs) 20:25, 7 November 2007 (UTC)
no --Doc James (talk) 03:13, 17 December 2008 (UTC)
New study information
[edit]http://news.bbc.co.uk/2/hi/health/5234838.stm
Someone who is interested in this topic might want to research this reported data. Figured it might help you out in the work here. ciao
statement with void content
[edit]- "A classical ectopic pregnancy never develops into a live birth."
What does the word "classical" in this context denote. It severely undervalues the usefulness of the word "never" later in the sentence. Without any explanation of what makes an ectopic pregnancy classical, there is no logically sound way to assess what the sentence means. Am commenting it out, until something more sensible can replace it. -- Cimon Avaro; on a pogostick. 09:34, 6 October 2006 (UTC)
confused
[edit]I don't get it; why can't they just relocate the fetus to the uterus and re-implant it? I admit I'm not a doctor or anything, it just seems like in today's world, where we can implant other nerves into arms to create new artificial limbs it's weird we can't even relocate a fetus.--Anoma lee 03:15, 31 October 2006 (UTC)
-Because the placenta would have to be relocated as well. Detatching the placenta from its attachment site would destroy the blood vessels, making it useless. Sjc80 06:20, 13 January 2007 (UTC)
Author?
[edit]"In this author's experience this is invariably bowel or mesentery, but other sites, such as the renal (kidney), liver or hepatic (liver) artery or even aorta have been described. "
Wiki not place for origional research.. maybe it was copied from somewhere?
StarDolph 00:48, 29 November 2006 (UTC)
Hi, actually I am the author, with many years of experience in the Third World, and currently in practice in Canada. My department, with over thirty thousand deliveries a year, under adverse conditions, had likely the largest concurrent series of extrauterine pregnancy in the world. The insertions were as described, so I guess this is extensive personal experience. -- —Preceding unsigned comment added by JustAnMD (talk • contribs)
What about the statement of the possibility of male pregnancy. If that can't be supported with citations then it has to be removed. I am not, however, disagreeable to keeping the statement if a reasonably sizeable group has expressed such a view, evidence can be produce to show that they hold this view, and the statement is reflected as such. -*- u:Chazz/contact/t: 02:31, 3 December 2006 (UTC)
In response to Chazz88, this does worry me a bit. It is actually little more than science fiction, and is not to my knowlege the subject of serious research. Maybe it should go? ``` —Preceding unsigned comment added by JustAnMD (talk • contribs)
If you have an American M.D. and concur with my view then I would go ahead and delete the comment I refer to in my comment above. If, and when, evidence can be produced, as described in my comment above, regarding this issue then it can be re-inserted. Until now I think it is safe to delete it. -*- u:Chazz/contact/t: 20:27, 3 December 2006 (UTC)
Canadian will do? And specialty in OB/Gyn. I will take it out, but am new at this writing thing. —Preceding unsigned comment added by JustAnMd (talk • contribs)
- I suppose it will have to. Just kidding! Ohh.. a tip for you. Sign your comments on talk pages by putting 4 tildes at the end (if in doubt see the information below the page you use to "edit" articles). Welcome to the Wikipedia project I am sure we could do with your support and knowledge. I would suggest that you read the some of the different Wikipedia project articles (i.e. those on how to write articles, what you can and can't write, basic ground rules and a lot more, the Wikipedia Comunity). Don't try and read them all, especially immediately as there are far too many! Just get accustommed with the basics. Can I suggest Community Portal, Wikipedia's Medicine Portal (OB/GYN and [Surger|surgery in general]] comes under the Portal's remit), Wikipedia's policies on [Wikipedia:No original research|original research]] (i.e. don't do it) what it isn't, neutrality, verifiability, citing sources and how to edit a page on Wikipedia. -*- u:Chazz/contact/t: 23:10, 3 December 2006 (UTC)
Thanks
[edit]To the author for such a well written article - We hope you'll be satisfied and not offended by the external link we have added? -
The Ectopic Pregnancy Trust is a source of information and support for those who have suffered the condition. The Charity is medically overseen and moderated, and though UK based, (recognised by the National Health Service(UK), Department of Health(UK), and The Royal College of Obstetricians and Gynaecologists(UK)) They serve the population of the web at large.
Many thousands now use this on line encyclopedia and the missions of the EPT, who provide afore mentioned resource: Is to raise awareness of ectopic pregnancy among health professionals and the general public: To offer support to people affected by the condition: And to support research in to early diagnosis. It provides telephone support and information from trained and qualified staff and connect users with others who have experienced ectopic pregnancy. It promotes research into the causes, treatment and prevention of ectopic pregnancy, and provides information Leaflets. Information is also available, along with message boards, on their website.
Causes
[edit]- The causes of ectopic pregnancy are unknown. After fertilization of the oocyte in the peritoneal cavity, the egg takes about nine days to migrate down the tube to the uterine cavity at which time it implants. Wherever the embryo finds itself at that time, it will begin to implant.
Fertilization does not necessarily occur prior to the egg entering the oviduct; it can occur within the oviduct as well. As such, there are a number of problems with the statements made above:
- fertilization does not necessary occur within the peritoneal cavity.
- Is it the "taking of nine" days that stimulates the egg to implant or does it take nine days for the egg to travel the length of the oviduct? The comment that follows, wherever the embryo finds itself at that time, it will begin to implant suggests that the egg will implant 9 days post-fertilization. At which time it implants, however, is suggestive that entrance into the uterus is a stimulation for implantation, which would result in no ectopic implantations.
This paragraph should be edited to reflect physiologic accuracy and grammatical unambiguity. DRosenbach (Talk | Contribs) 20:26, 9 January 2008 (UTC)
Advanced Maternal Age?
[edit]The article says advanced maternal age is a risk factor. I have never heard this before and there is no citation for it. Can anyone provide a citation? If not, I will remove it. Nathanaver (talk) 20:04, 22 April 2008 (UTC)
- [2] - I can't even see an abstract, so no idea what it contains. Still, the title kinda says everything, doesn't it? Though I'd be interested to know what their population and range of ages were. Also [3] WLU (talk) 20:53, 22 April 2008 (UTC)
- Thanks, I will have a look at these later today. Just glancing at them, and a couple others I found, the discussion sections suggest that the authors believe that the increased risk is likely due to the cumulative effects of other things, like PID, not maternal age itself. Nathanaver (talk) 12:18, 23 April 2008 (UTC)
Nontubal ectopic pregnancy
[edit]Two parts of this section need a citation, If none can be found I think they should be deleted since they seem unlikely anyway. "While a fetus of ectopic pregnancy is typically not viable, very rarely, a live baby has been salvaged from an abdominal pregnancy." "Cases have been known where a tubal pregnancy burst and the pregnancy continued with the growing placenta attaching to internal organs. In one such case the pregnancy after this had no amniotic sac and the baby was loose among its mother's intestines; laparotomy rescued the baby, and it lived."
This last story seems very unlikely since a tubal rupture and ectopic pregnancy are leading causes of maternal deaths. No to mention that the baby living with out an amniotic sac is unlikely, especially after it would have to get cut from its implant site out side of the uterine wall.
I have never edited a Wiki article before let alone wrote anything in the discussion section, so I am afraid to look into this myself. I was simply researching and these seemed out of place and I was afraid that pro-life people may have edited this to try to misinform people about the severity of ectopic pregnancies and the need for removal of the pregnancy to prevent the death of the mother. —Preceding unsigned comment added by 76.219.160.103 (talk) 01:48, 3 May 2008 (UTC)
- Actually, the first paragraph you bring up is cited - just not adjacent to the topic sentence. Check out references 4 and 5 - both are BBC News stories specifically referring to births where the fetus anchored in the abdominal area, in one case near the stomach and the other in the fat lining the bowel. Both citations are near the sentence claiming that there is little data except anecdotes due to the rarity of the condition. While the validity of a news source versus a medical journal may be questioned, the BBC is a reputable source of information and the references in question have stood since 2006. Specifically, the term 'abdominal pregnancy' is used in source 5. A medical source should be used for the initial citation, but it has been shown that the condition described does occur.
- The second sentence you bring up seems to be a continuation of the concept in the paragraph, although it is written vaguely and lacks its own citation. Both would have to be fixed severely for the sentence to be usable in the article. I'm going to comment it out - JustAnMD brought it up as well last year and little progress has been made. It can always be reverted if needed.
- Last, you do realize that most pro-life groups, including such entities as the Catholic Church mentioned earlier in this talk page, allow removal of ectopic pregnancies because of the risk to the mother, right? Both references refer to pregnancies where the ectopism was not recognized until the C-section was performed, else both would have been removed far earlier. Even with both remaining, the articles detail how the mothers needed surgical intervention and large amounts of transfused blood - the risks are pretty well codified there, not to mention earlier in the wiki article itself. Deciding that something should be removed because it might support someone else's position is bad on all sides. ZekeSulastin (talk) 20:58, 6 May 2008 (UTC)
- I added an Associated Press story from Australia of an ectopic pregnancy in an ovary, in which a healthy 2.8 kg baby girl was delivered via Caesarean after a 38 week pregnancy. The story quotes the parents and a general manager of the hospital. I would look for additional sourcing to the doctor and in some medical journal. The ectopic nature of the pregnancy was not detected in exams during the pregnancy. Edison (talk) 14:17, 30 May 2008 (UTC)
- Added more details: Quotes from the obstetrician who delivered the baby. Edison (talk) 18:29, 30 May 2008 (UTC)
I restored another account of an ectopic pregnancy resulting in a live birth, which someone had removed on the ground that all content must come from medical journals or textbooks per a guideline, That guideline actually says that newspapers provide earlier accounts than the more scholarly sources, and does not forbid any mention of things reported by reliable sources such as major newspapers. Edison (talk) 04:25, 4 September 2008 (UTC)
- No journals have the info first and then the newspaper takes the info and sometimes misrepresents it.--Doc James (talk) 03:17, 17 December 2008 (UTC)
I think there should be a reference for this line "but other sites, such as the renal (kidney), liver or hepatic (liver) artery or even aorta have been described". I can't find any medical or scientific papers describing it. —Preceding unsigned comment added by 76.26.101.240 (talk) 17:15, 2 July 2009 (UTC)
Illustration
[edit]I fail to see how the de Graaf illustration is an appropriate picture to include in this article. It is not even close to being anatomically accurate. I think that a more realistic representation would be a positive addition. 68.81.116.33 (talk) 07:39, 20 September 2008 (UTC)
- realistic isn't always the same as informative. IMO it shows clearly to a lay person what is taking place in a way that a more literal depiction wouldn't. --86.138.30.7 (talk) 04:18, 1 November 2008 (UTC)
Erratum?
[edit]Is the following sentence (from the article) a mistake?
An empty uterus with levels lower than 1500 IU/ml may be evidence of an ectopic pregnancy, but may also be consistent with an intrauterine pregnancy which is simply too small to be seen on ultrasound.
164.111.16.221 (talk) 13:40, 4 November 2008 (UTC)
- Nope this is true just poorly worded.--Doc James (talk) 03:15, 17 December 2008 (UTC)
Prevention?
[edit]Are there known working preventive measures? If so, a section on prevention would benefit the article. And if not, that fact should be clearly stated as well. -- 212.63.43.180 (talk) 15:44, 4 December 2008 (UTC)
- No preventative measures other then the avoidance of the risk factures now discussed under cause.--Doc James (talk) 03:16, 17 December 2008 (UTC)
Risk factors
[edit]The role of chlamydia should be discussed (http://www.bmj.com/cgi/content/full/316/7147/0/b.), as with the current increasing ectopic pregnancy rate with the increasing chlamydia incidence (still need citation). IUDs have also been linked to increased ectopic pregnancy (still need citation). —Preceding unsigned comment added by 134.36.53.20 (talk) 21:30, 9 December 2008 (UTC)
- added info about risks --Doc James (talk) 03:14, 17 December 2008 (UTC)
Clarification needed
[edit]The chance of future pregnancy depends on the status of the adnexa left behind. The chance of recurrent ectopic pregnancy is about 10% and depends on whether the affected tube was repaired (salpingostomy) or removed (salpingectomy). Successful pregnancy rates vary widely between different centuries,[clarification needed] and appear to be operator dependent.[clarification needed] Pregnancy rates with successful methotrexate treatment compare favorably with the highest reported pregnancy rates. Often, patients may have to resort to in vitro fertilisation to achieve a successful pregnancy.[clarification needed] The use of in vitro fertilisation does not preclude further ectopic pregnancies, but the likelihood is reduced.
What do centuries have to do with this? And what is the case under discussion?
What is meant by "operator dependent"? Who was the operating surgeon? If so, then it would be interestng to know why.
What is "often"? In wich case? Since "the chance of recurrent ectopic pregnancy is about 10%", an ectopic pregnancy seems no reason to resort to in vitro fertilisation, and certainly not to call it a must. If it means after removal of a tube, then that should be specified. Debresser (talk) 17:23, 21 December 2009 (UTC)
- I didn't author those statements but have clarified the ones I could and have deleted others. --David Iberri (talk) 21:04, 21 December 2009 (UTC)
- Much appreciated. Debresser (talk) 21:37, 21 December 2009 (UTC)
2nd image
[edit]It would be very helpful to have a brief description of what has been removed here [[File:Ruptured_ectopic_pregancy.JPG]] (other than the fetus) please.
Thanks very much.--TyrS (talk) 09:05, 29 August 2010 (UTC)
What percentage of ectopic pregnancies actually threaten the life of the mother?
[edit]The occurrence of these types of pregnancies is given as 1%, but what percentage of that figure actually threatens the life of the mother? 67.233.244.199 (talk) 04:48, 14 June 2011 (UTC)
- All of them if not appropriately treated. Doc James (talk · contribs · email) 06:35, 12 March 2015 (UTC)
video
[edit]Can we use this video? It provides a lot of missing info about the Jane Ingram case and also about another case unique in medical history not mentioned in the article. --Espoo (talk) 16:31, 17 November 2013 (UTC)
- It's unavailable now, so I don't think so. Mikael Häggström (talk) 10:48, 16 February 2014 (UTC)
Inaccurate image
[edit]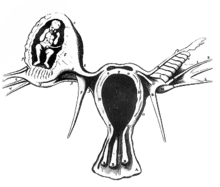
I moved removed the image at right from the article, because it appears to show a fetus inside the ovary, which is nonexistent to extremely rare. Also, there are many other inaccuracies, such as the fallopian tubes appearing to end at the roof of the fundus, and the proper left fallopian tubes has strange appendices attached to it. Mikael Häggström (talk) 10:52, 16 February 2014 (UTC)
History of methotrexate treatment of ectopic pregnancies
[edit]Previously, the "medical" section of the article stated that methotrexate was a viable treatment option "at least since 1993". I have found a reference which states that methotrexate treatment was developed "during the 1980s". Accordingly, I have adjusted the article, replacing the old reference with my new one. Goblinshark17 (talk) 06:20, 18 September 2014 (UTC)
Relation of Endometriosis to ectopic pregnancy
[edit]I note that the page now says (under Causes) there is no link between endometriosis and EPs, despite older texts to the contrary (per citation 12). I think this is a bit oversimplified.
While endometriosis may not increase the risk for all women over control groups, per se, if endometriosis causes partial obstruction of a fallopian tube, either directly or by kinking due to adhesions around the tube, then this will increase the risk, as would any kind of partial obstruction (such as stated in the same section). I believe this should be clarified, because it's blatantly false to say that endometriosis can never result in damage leading to an EP, but at the same time, endometriosis isn't going to increase your risk if your tubes are patent.
I feel that this is worth explaining. Dis/Agree?
82.15.170.150 (talk) 00:43, 12 July 2015 (UTC)
- We should be using reviews not primary sources. Will update thanks. Doc James (talk · contribs · email) 06:38, 12 July 2015 (UTC)
External links modified
[edit]Hello fellow Wikipedians,
I have just added archive links to one external link on Ectopic pregnancy. Please take a moment to review my edit. If necessary, add {{cbignore}} after the link to keep me from modifying it. Alternatively, you can add {{nobots|deny=InternetArchiveBot}} to keep me off the page altogether. I made the following changes:
- Added archive https://web.archive.org/20080603100609/http://ap.google.com:80/article/ALeqM5h7An_4HQLG6rSVO-h1eBIntgYOyAD90VRLKO1 to http://ap.google.com/article/ALeqM5h7An_4HQLG6rSVO-h1eBIntgYOyAD90VRLKO1
When you have finished reviewing my changes, please set the checked parameter below to true to let others know.
This message was posted before February 2018. After February 2018, "External links modified" talk page sections are no longer generated or monitored by InternetArchiveBot. No special action is required regarding these talk page notices, other than regular verification using the archive tool instructions below. Editors have permission to delete these "External links modified" talk page sections if they want to de-clutter talk pages, but see the RfC before doing mass systematic removals. This message is updated dynamically through the template {{source check}} (last update: 5 June 2024).
- If you have discovered URLs which were erroneously considered dead by the bot, you can report them with this tool.
- If you found an error with any archives or the URLs themselves, you can fix them with this tool.
Cheers. —cyberbot IITalk to my owner:Online 11:49, 28 August 2015 (UTC)
Missing word
[edit]"...a "pseudosac", which is a collection of within the endometrial cavity that may be seen in up to 20% of women." A collection of what? Equinox (talk) 19:08, 10 September 2015 (UTC)
Strange language
[edit]It's in the heading and reads as
"The risk of death among those in the developed world is between 0.1 and 0.3 percent while in the developing world it is between one and three percent."
1. Why are the percentages not clear or parallel. Switches from using decimals to words to describe percentage. 2. The source cited does not make a statement about "the developed" world. Inadequate citation. DrOctoCat (talk) 08:52, 16 December 2016 (UTC)
- User:DrOctoCat thanks. Agree and done. Doc James (talk · contribs · email) 23:18, 16 December 2016 (UTC)
External links modified
[edit]Hello fellow Wikipedians,
I have just modified 3 external links on Ectopic pregnancy. Please take a moment to review my edit. If you have any questions, or need the bot to ignore the links, or the page altogether, please visit this simple FaQ for additional information. I made the following changes:
- Added archive https://web.archive.org/web/20150402110050/http://www.catholic.com/audio-player/8236 to http://www.catholic.com/audio-player/8236
- Added archive https://web.archive.org/web/20101223214452/http://www.ardms.org/downloads/RegistryReports/Sep99.pdf to http://www.ardms.org/downloads/RegistryReports/Sep99.pdf
- Added archive https://web.archive.org/web/20110930051227/http://web.ksl.com/dump/news/cc/special/science/ectopic.htm to http://web.ksl.com/dump/news/cc/special/science/ectopic.htm
When you have finished reviewing my changes, you may follow the instructions on the template below to fix any issues with the URLs.
This message was posted before February 2018. After February 2018, "External links modified" talk page sections are no longer generated or monitored by InternetArchiveBot. No special action is required regarding these talk page notices, other than regular verification using the archive tool instructions below. Editors have permission to delete these "External links modified" talk page sections if they want to de-clutter talk pages, but see the RfC before doing mass systematic removals. This message is updated dynamically through the template {{source check}} (last update: 5 June 2024).
- If you have discovered URLs which were erroneously considered dead by the bot, you can report them with this tool.
- If you found an error with any archives or the URLs themselves, you can fix them with this tool.
Cheers.—InternetArchiveBot (Report bug) 17:21, 5 December 2017 (UTC)
UCSF Foundations II 2019, Group 7A goals
[edit]Goals:
- Edit and add new information for each section along with citation
- Improve organization of article if needed
- Add dosage of medications for the treatment of ectopic pregnancies that are used in the US
- Research and add more information about the correlation of chlamydia and ectopic pregnancy
- Research fertility after the treatment of an ectopic pregnancy and the recurrent rate
Sara.F.Shaikh (talk) 21:27, 30 July 2019 (UTC)
- I'm not sure what you mean with that last bullet point. (added list formatting) Health policy (talk) 03:40, 31 July 2019 (UTC)
Chlamydia infections are common in young sexually active adults and often the infection is treated with a course of antibiotics, but if the infection is left untreated it can have long term effects. There have been many studies that have investigated the association, but there have been many contraindications. A study in Sweden found that there was a decrease in the number of ectopic pregnancies when there was a decrease in the rate of C. trachomatic (chlamydia). On the other hand, an Australian study found no association between the two. Although there is no strong evidence of the association, recent studies have stated that there is a low risk of ectopic pregnancies and high fertility rates after a chlamydia infection.
To treat ectopic pregnancies, surgeries are required when there are contraindications to medicine, or if there is a ruptured ectopic pregnancy, or if the patient prefers it. Two of these surgeries include Salpingectomy and Salpingostomy. The Salpingectomy procedure is the removal of a fallopian tube while in Salpingostomy an opening is created into the fallopian tube. A study found that patients that undergo these procedures have a similar recurrent ectopic pregnancy rate. 5% for Salpingectomy and 8% for salpingostomy. Additionally, the rate of intrauterine pregnancy rates were also similar; 56.2% and 60.7% respectively.
Methotrexate is used as a treatment of ectopic pregnancies and studies have shown that the drug does not affect future fertility treatments. There were multiple studies that looked at the number of oocytes that were retrieved before and after the treatment with methotrexate and found that there was not a significant difference.
The United States uses a multi dose protocol of methotrexate (MTX) which involves 4 doses of intramuscular 1mg/kg MTX along with a intramuscular injection of folinic acid (0.1mg/kg) to protect cells from the effects of the drug and to reduce the side effects.[4]
Although the exact mechanism through which chlamydia increases the risk of ectopic pregnancies is uncertain, some research suggests that the infection can significantly affect the structure of Fallopian tubes.[5] Michaelfashola (talk) 08:41, 7 August 2019 (UTC)
References
- ^ Bakken, Inger J (February 2008). "Chlamydia trachomatis and ectopic pregnancy: recent epidemiological findings". Current Opinion in Infectious Diseases. 21 (1): 77–82. doi:10.1097/QCO.0b013e3282f3d972.
- ^ Brady, Paula C. (October 2017). "New Evidence to Guide Ectopic Pregnancy Diagnosis and Management". Obstetrical & Gynecological Survey. 72 (10): 618–625. doi:10.1097/OGX.0000000000000492.
- ^ Ohannessian, A.; Loundou, A.; Courbiere, B.; Cravello, L.; Agostini, A. (23 July 2014). "Ovarian responsiveness in women receiving fertility treatment after methotrexate for ectopic pregnancy: a systematic review and meta-analysis". Human Reproduction. 29 (9): 1949–1956. doi:10.1093/humrep/deu174.
- ^ Marret, Henri; Fauconnier, Arnaud; Dubernard, Gil; Misme, Hélène; Lagarce, Laurence; Lesavre, Magali; Fernandez, Hervé; Mimoun, Camille; Tourette, Claire; Curinier, Sandra; Rabishong, Benoit; Agostini, Aubert (October 2016). "Overview and guidelines of off-label use of methotrexate in ectopic pregnancy: report by CNGOF". European Journal of Obstetrics & Gynecology and Reproductive Biology. 205: 105–109. doi:10.1016/j.ejogrb.2016.07.489.
- ^ Sivalingam, VN; Duncan, WC; Kirk, E; Shephard, LA; Horne, AW (October 2011). "Diagnosis and management of ectopic pregnancy". The journal of family planning and reproductive health care. 37 (4): 231–40. doi:10.1136/jfprhc-2011-0073. PMID 21727242.
Emily's Review to UCSF Foundations II 2019, Group 7A
[edit]Goal 1: The group is off to a good start and has added information to 3 sections, but has not met their goal of editing every section.
Goal 2: The group has not yet edited anything related to guidelines.
Goal 3: The group has met their goal of adding information related to the correlation between chlamydia and ectopic pregnancy.
Goal 4: The group added statistics related to fertility after the use of methotrexate and, salpingectomy and salpingostomy.
"Studies have shown" is mentioned, but there are no names of specific studies mentioned.
Overall, the group has added pertinent information to the article and has improved it. They have not yet met all their goals.
No evidence of plagiarism or copyright violation was found.
Emilyplasencia (talk) 21:46, 5 August 2019 (UTC)
Matt's Review
[edit]Part 1: The article was not substantially improved, however, it is already heavily edited. Group 7a's goals were mostly met as new information was added to multiple sections. Specially, correlation between chlamydia and ectopic pregnancy was stated and rates of recurrent ectopic pregnancy were stated. Also, the role of methotrexate was elaborated upon. However, this information might better belong under the treatment section as opposed to the prognosis section.
Part 2: The information added to the article maintained its neutral point of view.
Maludino (talk) 21:27, 5 August 2019 (UTC)
Colette's Review of UCSF Foundations 2 2019, Group 7a Goals
[edit]Goal 1. Some, but not all, sections were edited with inclusion of significant information.
Goal 2. No guidelines were revised nor updated yet.
Goal 3. Information was added to elaborate on the relationship between chlamydia and ectopic pregnancy.
Goal 4. Additional information on treatment and recurrent rate was provided.
More details on methotrexate would be helpful to readers' overall understanding of this treatment option.
Added points were supported by information included in cited secondary sources.
Cpktruong (talk) 21:39, 5 August 2019 (UTC)
Jacklyn Ang's Review for Foundations II 7a, group edits
[edit]•Do the group’s edits substantially improve the article as described in the Wikipedia peer review “Guiding framework”? It has not been substantially improved, but additional content did provide more points to consider to the article. These points provided neutral perspectives (with statistics and findings from research) along with appropriate references to look up into.
For the sentences added onto the Surgical header, I would recommend reformatting the second sentence that was incorporated. "Respectively" was the last word utilized in both sentences, so there was repetition of sentence formatting.
•Are the edits formatted consistent with Wikipedia’s manual of style? If not, specify…
Yes, the edits were consistent with Wikipedia's manual of style. References were appropriately cited and the sentences were consistent.
• Has the group achieved its overall goals for improvement?
The group's goals were:
Edit and add new information for each section along with citation---->not every section was edited and added, but it may be because it was already heavily worked on; Revise and update any guidelines that are mentioned-->no updates as of right now; Research and add more information about the correlation of chlamydia and ectopic pregnancy-->Yes, this was done (before contents were introduced); Research fertility after the treatment of an ectopic pregnancy and the recurrent rate-->Yes, this was done (under future fertility)
Jacklyn.Ang (talk) 21:56, 5 August 2019 (UTC)
Add something explicitly explaining the science of why the pregnancy cannot be “relocated”
[edit]It has become a “known fact” in political circles that we just aren’t trying to “save these babies.” As an ectopic survivor who is worried that others will die, please spell this out plainly. I see it answered above, but it needs to be that plain on the page… with citations. I don’t have the citations. 2600:1700:F90:6950:3050:6D2C:AA4:29BE (talk) 23:55, 3 May 2022 (UTC)
Fallopian has needless capital letter
[edit]~1/3 of the mentions of fallopian have a capital letter in sentences. Maybe I'm missing some grammar/Wikipedia rule but I don't think they should have capital letter. Wadvann (talk) 16:23, 5 May 2022 (UTC)
- B-Class medicine articles
- High-importance medicine articles
- B-Class WikiProject Medicine Translation Task Force articles
- High-importance WikiProject Medicine Translation Task Force articles
- WikiProject Medicine Translation Task Force articles
- B-Class reproductive medicine articles
- High-importance reproductive medicine articles
- Reproductive medicine task force articles
- All WikiProject Medicine pages
- B-Class women's health articles
- High-importance women's health articles
- WikiProject Women's Health articles


