User:Kyriakos27/sandbox
This article has multiple issues. Please help improve it or discuss these issues on the talk page. (Learn how and when to remove these messages)
|
Asymptomatic Hyperleukocytosis/Symptomatic Hyperleukocytosis (Leukostasis)
[edit]
Symptomatic Hyperleukocytosis (Leukostasis) is defined by a tremendously high blast cell count along with symptoms of decreased tissue perfusion. Leukostasis is associated with people who suffer from bone and blood disorders and is very common among people suffering from acute myeloid leukemia or chronic myeloid leukemia. Leukostasis is a pathlogic diagnosis that inhibits efficient flow to the microvasculature of the body. Continued and untreated leukostasis presents respiratory and neurological distress simultaneously and is a medical emergency, with untreated patient mortality rates reaching a minimum of 20 and a maximum of 40 percent.. A leukemia blood cell count greater than 50 x 10^9/ L (50,000 / microL) or 100 x 10^9 L / (100,000/ microL) signifies hyperleuckocytosis. Symptoms of leukostasis start when blood levels of leukocytes reach over 100 x 10^9 / L (100,000 / microL). As stated before, these counts are critical and associated with Leukemias.[1]
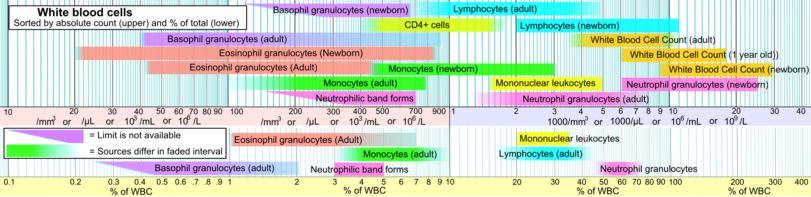
The mechanism in which hyperleukocytosis / leukostasis manifests and disrupts homeostasis is greatly associated with leukemia's but there are multiple other factors that may cause leukocytosis. Major types of leukocytosis and their mechanisms depend on the types of Leukemia that cause them. White blood cell levels either rise in distinct white blood levels or in unison with others, a patient may be suffering from neutrophilia, lymphocytosis, monocytosis, eosinophilia, basophllia or a rise in immature blast cells.
Acute myeloid leukemia - 10 to 20 percent of patients newly diagnosed with this type leukemia have hyperleukocytosis
Acute lymphblastic Leukemia - 20 to 30 percent of patients newly diagnosed with this type of leukemia have hyperleukocytosis
Chronic lymphocytic leukemia - Exact percentage of people diagnosed with chronic lymphocytic leukemia is unknown but a significant amount is also suffer from hyperleuckocytosis
Chronic myeloid leukemia - The majority of patients suffering from chronic myeloid leukemia usually suffer from hyperleuckocytosis.
The primary pathophysiology of leukostatis is not completely understood but there are two possible theories.
Theory 1: Increased blood viscosity due to large leukemic blast populations which are less deformable than mature leuckocytes may lead to leukostasis. The accumulation of less malleable blast products in the bloodstream accumulate within the microcirculation causing an accumulation of blockages leading to leuckostasis.
Theory 2: Hypoxic events in body regions may increase the high metabolic activity of dividing blast cells and lead to an increase in cytokine production. The increasing levels of cytokines within tissues, may results in endothelial damage and subsequent hemorrhage. Therefore, hypoxia in addition to various cytokine accumulations, act in unison to further damage tissue and attract leukemic blast cells to form a triad of damage.
The combination of these theory's in addition to other events may lead to hyperleukocytosis.
When a patient is suffering from symptomatic leuckocytosis, specifically caused by a form a leukemia, it is extremely common to find leukostasis in all their organs. The majority of the time a patient dies from neurological complications (40% of patients die due to neurological conditions) as opposed to particular organ damage. The lungs alone account for approximately 30 percent of leukostasis fatalities. All other organs combined attribute to 30 percent of deaths, with the major outliers being neurological and respiratory failure equating to 70 percent of all death rates. Damage to the microvasculature of the body is the primary cause of death by leukostasis. Microvasculatre damage to the lungs is only second to neurological damage because the body is already suffering from hypoxic conditions, which leads to lung tissue damage as the second leading cause of fatalities.
Pulmonary signs - Dyspnea and Hypoxia with or without diffuse interstitial or alveolar infiltrates on imaging studies.
Neurological signs - visual changes, headache, dizziness, tinnitus, gait instability, confusion, somnolence, coma.
The most common symptom is the patient is usually febrile, which is often linked with inflammation and possible infection.
Less common symptoms include electroencephalographic, signs of myocardial ischemia / right ventricular overload, increased renal insufficiency, priapism, acute limb ischemia and bowel infarction.
White blood counts exceeding 100 x 10^9 / L (100,000 / microL) present symptoms of tissue hypoxia and may signal possible neurological and respiratory distress. Continuing research has shown that patients have suffered from hypoxia at leukocyte levels below 100 x 10^9 / L (100,000 / microL), therefore patients with leukemia need regular neurological and respiratory monitoring when leukocyte counts are approaching 100 x 10^9 / L (100,000 / microL) to decrease chances of tissue hypoxia.
Biopsy's acquired are examined for damage to microvasculature, which serves as evidence of hypoxia through the identification of leukocyte blockage within the tissue. Due to a biopsy's invasive nature and the risks associated with the procedure, it is only used when deemed necessary.
Measurements for arterial pO2 have shown to be falsely decreased in patients with hyperleuckocytosis because of white blood cells ability to utilize oxygen. Pulse oximetry should be used to more accurately asses pO2 levels of a patient suspected to be suffering from leukocytosis.
Automated blood cell counters may be inaccurate due to fragments of blast cells being labeled on blood smears as platelets. The most accurate form of confirming platelet counts is by using a manual platelet count and review of a peripheral smear.
Serum potassium levels may also be artificially elevated caused by a release from leukemic blasts during in vitro clotting process, therefore serum potassium levels should be monitored by herparinized (the addition of herapin prevents coagulation) plasma samples in order to obtain accurate results of potassium levels.
Disseminated intravascular coagulation may occur in a significant amount of patients with presentation of various degrees of thrombin generation, followed by decreased fibrinogen and increased fibrinolysis.
Spontaneous tumor lysis syndrome is present in approximately 10 percent of patients with leuckostasis, lab tests are used to measure the potential of elevated serum concentrations such as uric acid, potassium, phosphate, and hyocalcemia.
Disseminated intravascular coagulation and spontaneous tumor lysis syndrome have the ability to develop before and after chemotherapy treatment. Patients undergoing this type of therapy need to be closely monitored before and after in addition to undergoing prophylactic measures to prevent possible complications.
Since leukostais/ hyperleukostasis is associated with leukemia, preventative treatments are put into action upon diagnosis.
Patients with hyerleukocystois associated with leukemia are always considered candidates for tumor lysis syndrome prophylaxis in addition to aggressive intravenous hydration with allopurinol or rasburicase to decrease serum uric acid levels.
Additional causes of Asymptomatic/Symptomatic Hyperleukocytosis (Leukostasis)
[edit]| Causes of leukocytosis | ||||
|---|---|---|---|---|
| Neutrophilic leukocytosis (neutrophilia) |
||||
| Eosinophilic leukocytosis (eosinophilia) |
| |||
| Basophilic leukocytosis Basophilia |
(rare)[3] | |||
| Monocytosis | ||||
| Lymphocytosis |
| |||
Hyperleukocytosis is very common in acutely ill patients. It occurs in response to a wide variety of conditions, including viral, bacterial, fungal, or parasitic infection, cancer, hemorrhage, and exposure to certain medications.
For lung diseases such as pneumonia and tuberculosis, white blood cell count is very important for the diagnosis of the disease, as leukocytosis is usually present.
Specific medications, including corticosteroids, lithium and beta agonists have the ability cause hyperleukocytosis.[4]
Treatment includes utilization of prophylactic methods in the event that the patient has been diagnosed with hyperleukocystosis. This is usually in combination with other treatments which are dependent on the type of leukemia. Specific treatments include lysis syndrome treatment in addition to aggressive intravenous hydration with allopurinol or rasburicase to decrease serum uric acid levels.
Since a primary cause of leukocystatis is caused by leukemia, surgery is often a treatment and dependent on tumor size and location.
Hematopoietic cell transplants are critical to correct leukostasis and leukemia.
Cytoreduction is also a critical course of treatment in order to rapidly decrease white blood cell counts. Twenty to forty percent of patients diagnosed with hyperkeuckocytosis die within the first week of symptom presentation. Patients with the best outcome have none or limited symptoms of respiratory or neurological distress. An accumulation of these symptoms leads to decreased levels of statistical survival compared to patients diagnosed with asymptomatic hyperleukocytosis alone.
Cytoreduction methods include chemotherapy, utilizing the drug hydroxyurea ( Hydroxyurea is usually used in asymptomatic hyperleukocytosis), and the less common leukapheresis procedure. This procedure is often utilized for asymptomatic hyperleuckocytosis patients who have induction chemotherapy postponed for patient specific factors.
Variants of Chemotherapy, including induction chemotherapy, are used to treat both elevated white blood cells counts while simultaneously targeting leukemia cells in bone marrow.
Prognosis of patients suffering from hyperleukocytosis is dependent on the cause and type of leukemia the patient has. Patients diagnosed with asymptomatic hyerpleukocytosis have significantly better survival rates than symptomatic hyperleuckocytosis (leukostasis). Preventative measures and contentious monitoring of patients diagnosed with leukemia is critical in receiving treatment as early as possible to prevent and treat hyperleuckocytosis.
Recent research
[edit]Recent and continuing research has shown that patients have suffered from hypoxia at leukocyte levels below 100 x 10^9 / L (100,000 / microL), therefore patients suffering from leukemia need regular neurological and respiratory monitoring when leukocyte counts are approaching 100 x 10^9 / L (100,000 / microL) to decrease chances of hypoxia.[2]
Leukemia and population types are also believed to be associated with possible symptoms and may require a change in treatment.[2]
Results of Tumore lysis/ consumption of coagulopathy in patients with acute leukemia much more often than in patients with chronic malignant hematological diseases.[5]
- Data retrieved for reference is 2017
References
[edit]- ^ Schiffer, Charles, MD. "Hyperleukocytosis and Leukostasis". UpToDate. Retrieved 11 November 2017.
{{cite web}}: CS1 maint: multiple names: authors list (link) - ^ a b c d e f g "Hyperleukocytosis and leukostasis in hematologic malignancies". www.uptodate.com. Retrieved 2017-12-12.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae Table 12-6 in: Mitchell, Richard Sheppard; Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson (2007), Robbins Basic Pathology, Philadelphia: Saunders, ISBN 978-1-4160-2973-1 8th edition.
- ^ Leukocytosis: Basics of Clinical Assessment, American Family Physician. November 2000.
- ^ Schellongowski, P.; Staudinger, T. (September 2013). "[Leukostasis and tumor lysis: important complications of hyperleukocytosis]". Der Internist. 54 (9): 1051–1060. doi:10.1007/s00108-013-3260-5. ISSN 1432-1289. PMID 23943008.
This section is empty. You can help by adding to it. (October 2017) |
See also
[edit]References
[edit]Category:Leukemia Category:Oncological Emergencies Category:Blood disorders Category:Hematopathology

