Tasimelteon
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Hetlioz, Hetlioz LQ |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a615004 |
| License data |
|
| Dependence liability | Low[1] |
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | not determined in humans[2] |
| Protein binding | 89–90% |
| Metabolism | extensive liver, primarily CYP1A2 and CYP3A4-mediated |
| Elimination half-life | 0.9–1.7 h / 0.8–5.9 h (terminal) |
| Excretion | 80% in urine, 4% in feces |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| ChEBI | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.114.889 |
| Chemical and physical data | |
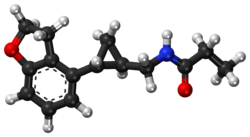
| Formula | C15H19NO2 |
| Molar mass | 245.322 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Tasimelteon, sold under the brand name Hetlioz, is a medication approved by the U.S. Food and Drug Administration (FDA)[3] in January 2014, for the treatment of non-24-hour sleep–wake disorder (also called non-24, N24 and N24HSWD).[4] In June 2014, the European Medicines Agency (EMA) accepted an EU filing application for tasimelteon[5] and in July 2015, the drug was approved in the European Union for the treatment of non-24-hour sleep-wake rhythm disorder in totally blind adults,[6] but not in the case of non-24 in sighted people.
The most common side effects include headache, somnolence, nausea (feeling sick) and dizziness.[7]
Medical uses
[edit]In the United States, tasimelteon capsules are indicated for the treatment of non-24-hour sleep–wake disorder (Non-24) in adults and for the treatment of nighttime sleep disturbances in Smith-Magenis Syndrome (SMS) in people sixteen years of age and older.[8] Tasimelteon oral suspension is indicated for the treatment of nighttime sleep disturbances in SMS in children from 3 to 15 years of age.[8]
In the European Union, tasimelteon capsules are indicated for the treatment of non-24-hour sleep–wake disorder (Non-24) in totally blind adults.[7]
The capsule and liquid suspension forms of tasimelteon are not interchangeable.[8]
Tasimelteon is a selective agonist for the melatonin receptors MT1 and MT2, similar to other members of the melatonin receptor agonist class of which ramelteon (2005), melatonin (2007), and agomelatine (2009) were the first approved.[9] As a treatment for N24HSWD, as with melatonin or other melatonin derivatives, the patient may experience improved sleep timing while taking the drug. Reversion to baseline sleep performance occurs within a month of discontinuation.[10]
Development
[edit]Tasimelteon (previously known as BMS-214,778) was developed for the treatment of insomnia and other sleep disorders. A phase II trial on circadian rhythm sleep disorders was concluded in March 2005.[11] A phase III insomnia trial was conducted in 2006.[12] A second phase III trial on insomnia, this time concerning primary insomnia, was completed in June 2008.[13] In 2010, the FDA granted orphan drug status to tasimelteon, then regarded as an investigational medication, for use in totally blind adults with N24HSWD.[14] (Through mechanisms such as easing the approval process and extending exclusivity periods, orphan drug status encourages development of drugs for rare conditions that otherwise might lack sufficient commercial incentive.)
On completion of Phase III trials, interpretations of the clinical trials by the research team concluded that the drug may have therapeutic potential for transient insomnia in circadian rhythm sleep disorders.[15] A year-long (2011–2012) study at Harvard tested the use of tasimelteon in blind subjects with non-24-hour sleep-wake disorder. The drug has not been tested in children nor in any non-blind people.
FDA approval
[edit]In May 2013, Vanda Pharmaceuticals submitted a New Drug Application to the Food and Drug Administration for tasimelteon for the treatment of non-24-hour sleep–wake disorder in totally blind people. It was approved by the FDA on January 31, 2014, under the brand name Hetlioz.[4] In the opinion of Public Citizen, an advocacy group, the FDA erroneously allowed it to be labelled without stating that it is only approved for use by totally blind people.[16] However, FDA updated its press release on Oct. 2, 2014 to clarify the approved use of Hetlioz, which includes both sighted and blind individuals. The update did not change the drug labeling (prescribing information).[17]
In Dec 2020, tasimelteon is approved by FDA for the treatment of Smith-Magenis Syndrome.[18]
Toxicity
[edit]Experiments with rodents revealed fertility impairments, an increase in certain cancers, and serious adverse events during pregnancy at dosages in excess of what is considered the "human dose".[19][20]
See also
[edit]References
[edit]- ^ Kim HK, Yang KI (December 2022). "Melatonin and melatonergic drugs in sleep disorders". Translational and Clinical Pharmacology. 30 (4): 163–171. doi:10.12793/tcp.2022.30.e21. PMC 9810491. PMID 36632077.
- ^ "Tasimelteon Advisory Committee Meeting Briefing Materials" (PDF). Vanda Pharmaceuticals Inc. November 2013.
- ^ "FDA transcript approval minutes" (PDF). FDA. November 14, 2013.
- ^ a b Food and Drug Administration (January 31, 2014). "FDA approves Hetlioz: first treatment for non-24 hour sleep-wake disorder" (Press release). FDA. Archived from the original on February 2, 2014. Retrieved December 16, 2019.
- ^ "tasimelteon (Hetlioz) UKMi New Drugs Online Database". Archived from the original on June 29, 2016. Retrieved August 6, 2014.
- ^ "Hetlioz Receives European Commission Approval for the Treatment of Non-24-Hour Sleep-Wake Disorder in the Totally Blind". MarketWatch. 7 July 2015. Archived from the original on 9 July 2015. Retrieved 8 July 2015 – via PR Newswire.
- ^ a b "Hetlioz EPAR". European Medicines Agency (EMA). Retrieved 2 December 2020.
- ^ a b c "Hetlioz- tasimelteon capsule". DailyMed.
- ^ Vachharajani NN, Yeleswaram K, Boulton DW (April 2003). "Preclinical pharmacokinetics and metabolism of BMS-214778, a novel melatonin receptor agonist". Journal of Pharmaceutical Sciences. 92 (4): 760–72. doi:10.1002/jps.10348. PMID 12661062.
- ^ Sack RL, Brandes RW, Kendall AR, Lewy AJ (October 2000). "Entrainment of free-running circadian rhythms by melatonin in blind people". The New England Journal of Medicine. 343 (15): 1070–7. doi:10.1056/NEJM200010123431503. PMID 11027741.
- ^ Clinical trial number NCT00490945 for "Safety and Efficacy of VEC-162 on Circadian Rhythm in Healthy Adult Volunteers" at ClinicalTrials.gov
- ^ Clinical trial number NCT00291187 for "VEC-162 Study in Healthy Adult Volunteers in a Model of Insomnia" at ClinicalTrials.gov
- ^ Clinical trial number NCT00548340 for "VEC-162 Study in Adult Patients With Primary Insomnia" at ClinicalTrials.gov
- ^ Lamberg L. "Improving Sleep and Alertness in the Blind (Part 5)". Matilda Ziegler Magazine for the Blind. Retrieved May 15, 2014.
- ^ Rajaratnam SM, Polymeropoulos MH, Fisher DM, Roth T, Scott C, Birznieks G, et al. (February 2009). "Melatonin agonist tasimelteon (VEC-162) for transient insomnia after sleep-time shift: two randomised controlled multicentre trials". Lancet. 373 (9662): 482–91. doi:10.1016/S0140-6736(08)61812-7. PMID 19054552. S2CID 36568291.
- ^ Carome M (1 July 2015). "Outrage of the Month: FDA Makes Major Blunder After Approving Drug for Rare Sleep Disorder". Huffington Post. Retrieved 8 July 2015.
- ^ Food and Drug Administration (January 31, 2014). "FDA NEWS RELEASE: FDA approves Hetlioz: first treatment for non-24 hour sleep–wake disorder in blind individuals". FDA.
- ^ "Search Orphan Drug Designations and Approvals". FDA. 1 December 2020. Retrieved 28 March 2023.
- ^ "Side Effects Drug Center: Hetlioz Clinical Pharmacology". RxList. February 10, 2014.
- ^ "Side Effects Drug Center: Hetlioz Warnings and Precautions". RxList. February 10, 2014.
In animal studies, administration of tasimelteon during pregnancy resulted in developmental toxicity (embryofetal mortality, neurobehavioral impairment, and decreased growth and development in offspring) at doses of up to 200 times greater than those used clinically.
External links
[edit]- "Tasimelteon". Drug Information Portal. U.S. National Library of Medicine.
