Talk:Neurofibromatosis/Archive 1
note
[edit]Per UTD, NF has complete penetrance, meaning all who have the mutation get the disease, but variable expression, meaning that severity is variable among people, including family members with the same genetic mutation resulting in NF phenotype. 24.211.245.225 (talk) 00:26, 24 June 2008 (UTC)
Added a brief and simplistic section on the hereditability of the diseases, which might be relevant to an a wikipedia reader. This is my first contribution to wikipedia so I'm uncertain how to handle citations -- since I'm not geneticist or neurologist, I can't easily evaluate what is common knowledge and not, and I chose to cite the handbook, though the authors of the handbook do not themselves provide citations for these facts.It can also be a type of skin cancer too.
I suggest that we find an official list of diagnostic criteria and use the same wording for the symptoms. This would add some authority and possibly clean up the language.
There is potentially enough material out there to fork the neurofibromatosis article into two (NF1 and NF2) but I am against the idea because it would require going into greater depth than I think appropriate for an encyclopedia and would increase the amount of material that would have to be maintained.
- We do already have articles for Neurofibromatosis type I and Neurofibromatosis type II. --Arcadian 15:04, 15 January 2006 (UTC)
Treatment
[edit]In the treatment section it is written: "Some people may find something in the herbal remedies that can slow down the growth of these tumors. [6]". Unfortunately, reference [6] does not seem to backup this assertion. Is this the right reference? - July 30, 2009
Another oddity: "A new clinical trial at NIH uses a drug called Pegintron. There are some accounts of cures in foreign countries." Whats 'foreign' on the internet? This whole section is America-centric. —Preceding unsigned comment added by 86.59.109.162 (talk) 02:17, 5 March 2010 (UTC)
I agree. The source does not back up that statement at all. The only information I could find about PEG-Intron as a treatment for NF were some clinical trials that don't seem to have progressed far enough to truly note PEG-Intron as a possible treatment (there are clinical trials relating to NF for several drugs, and it is not prudent to comment on each of them). Would anyone be opposed to the following fix?
"Because there is no cure for the condition itself, the only therapy for those people with neurofibromatosis is a program of treatment by a team of specialists to manage symptoms or complications [7]. Surgery may be needed when the tumors compress organs or other structures. Less than 10% of people with neurofibromatosis develop cancerous growths; in these cases, chemotherapy may be successful."
I basically cut out all the information about "herbal remedies" or "foreign cures" that had no source to back them up. In addition, I moved the current citation up in the paragraph, as it actually does provide information about current treatment options. I'll go ahead and make this change, because I don't think it's too controversial, and this talk page probably doesn't get a lot of attention, but feel free to revert if this goes against discussion etiquette. Zegota (talk) 08:04, 7 April 2010 (UTC)
Six subtypes
[edit]I'm honestly bothered that the six rare 'sub types' are listed. Some of the subtypes were solely found by Dr. Vincent Riccardi, or have such a few documented cases I don't believe the classifications of sub types have any strong stance as sub types, rather rare variants of this disorder. What I find odd is that segmental neurofibromatosis is not listed, which is likely to be more common these six sub types and some of the sub types could be considered segmental neurofibromatosis.
For the sake of educating the general public I think it is better to leave the sub-types out. The OMIM links are of little value to the lay public newly seeking information on NF
Purplesnappy 03:37, 7 March 2006 (UTC)
I have to agree that there are more than six variants. For example I have a vision that only appears as (large) tumors on (mostly-only) the right side of my body. There are sub versions that show Neurofibromatosis as affecting only the left or right site of one's body. What sub-versions I can't say for sure. I for one who is a sub-variant have to say that it is critical to include the sub-types. Bdelisle 08:55, 22 May 2006 (UTC)
NF-related groups
[edit]Perhaps it's time to do write-ups on some of the NF-related groups that do not have articles (e.g. Neurofibromatosis, Inc.) Anyone want to help tackle this? Artsygeek 18:32, 24 January 2007 (UTC)
One point on linking to groups: linking to fundraising pages of existing groups just clouds up the pages. Artsygeek (talk) 04:16, 24 November 2007 (UTC)
Hereditability
[edit]It is unnecessary to include a specific explanation of the inheritance pattern of an autosomal dominant trait in this article since the article's focus is on a particular disease rather than on inheritance patterns. A previous entry was reverted by a user asserting that the terms Autosomal Dominant (AD) and Penetrance were "Jargon". While I agree that penetrance would fall into this category (and agree with how it is presently handled in this article), AD is a term which is found in many wiki articles lacking a detailed explanation of its inheritance pattern. Moreover, the section about AD inheritance patterns, which was removed before the revert, appears twice in the article, once in the first section and again in the section on hereditability and genetics. Since NF displays variable penetrance, it is helpful to explain the disconnect between genotype and phenotype but detailing the % chance of passing along the gene is not warranted.
Users searching for neurofibramatosis who do not understand AD inheritance could find the necessary information by following the link to autosomal dominant.
I strongly recommend that the discussion of the chances of passing the allele to offspring be removed and replaced by a simply stated sentence indicating that the allele follows AD inheritance pattern. Dr. Doof (talk) 18:56, 2 June 2008 (UTC)
| “ | In general, specialized terminology should be avoided in an introduction. Where uncommon terms are essential to describing the subject, they should be placed in context, briefly defined, and linked. | ” |
- I would agree that explaining dominance twice is not useful, although a more complete explanation is suitable for the body of an article. It is not wrong the repeat certain things in the body of an article.
- --Steven Fruitsmaak (Reply) 21:17, 2 June 2008 (UTC)
I would argue that, especially in the lead section of this entry, a detailed discussion of heritability is unwarranted for two reasons. First, the purpose of the lead section is to introduce the subject and provide a short summary of the important aspects of the article. Explaining which child will inherit the gene goes beyond summarizing the important aspects of the article and borders on off topic WP:TOPIC. According to WP:MEDMOS:
| “ | When mentioning technical terms (jargon) for the first time, provide a short plain-English explanation in parentheses if possible. If the concept is too elaborate for this, wikilink to other articles (or Wiktionary entries). | ” |
Secondly, mentioning that a disorder is autosomal dominant, wikilinking it and providing an image describing AD inheritance is how the mention AD inheritance is handled in virtually every other wikipedia article on diseases with autosomal dominant inheritance.
Essentially, the mention of autosomal dominance and penetrance should be handled similarly in the introduction. Both should be mentioned with a concise explanation of their meaning and a wikilink provided to the relevant article. A brief discussion of heritability should be included in the article but spelling out which child born to a patient with NF, will inherit the disease is unnecessary. Dr. Doof (talk) 17:28, 3 June 2008 (UTC)
Since this disease seems to have complete penetrance but incomplete expressivity, shouldn't the article be amended to use the latter term?--Jimerama (talk) 16:53, 25 July 2008 (UTC)
SPRED mutations
[edit]In those with NF1 negative genetics, another marker has been found: http://jama.ama-assn.org/cgi/content/abstract/302/19/2111 JFW | T@lk 22:56, 17 November 2009 (UTC)
Dubious
[edit]Any reason why this woo is still in the article?
- "Some people may find something in the herbal remedies that can slow down the growth of these tumors.[dubious – discuss]" [7]
Joseph449008 (talk) 00:16, 17 February 2010 (UTC)
General Fix ups
[edit]Hello, I am not sure where or how to do this fix up. If you read both of the references I cited at the end, you will see that the most common mutation in NF1 is not a CIP/WAF family of CDK inhibitors like p21 rather a mutation in the neurofibromin, the protein product of the NF1 gene, which contains a GTPase activating gene that can abarently activate RAS which in turn activates the cell cycle in an unregulated fashion.
I also find it disturbing that we allow the citation of Kaplan USMLE study note be our primary source. Even the use of my sources is slightly not acceptable as they are text books (aka secondary sources).
Sources:
- Kumar, Vinay, Abul Abbas, and Nelson Fausto. Robbins and Cotran Pathologic Basis of Disease. 8th edition edition. Philadelphia, Pennsylvania: Elsevier Saunders, 2010. Print. pg 294-295
- Gutmann D, Collins F. Neurofibromatosis 1, 2nd ed. In Vogelstein B, Kinzler K. The genetic basis of human cancer. New York, McGraw-Hill, 2002. Print. pg 417-437
Angry Ayrab (talk) 06:42, 1 January 2011 (UTC)
Ya true, but KAPLAN is pretty valid since most of their authors are very old school physicians with lots of experience. Also KAPLAN offers a great variety of clinical data in a succint fashion. Hey, if you can find something more suitable that carries the same message be my guest. I use a lot of Rubin's stuff and Rubin is essentially a very reliable source. cheers Dr. Persi (talk) 10:18, 1 January 2011 (UTC)
OK, the article was in decent shape but was almost innudated by irrelevant, trivial data such as "popular culture." There were also errors in the sources, and some of the data needed expansion and clarification. There was no link to NF-1, and there were countless other minor issues which are all fixed now! I have removed the section on Popular Culture and am putting it here. It is my stern belief that data like this really offers nothing significant to the reader except cloud the article making it look heavy. Here is the cut section:
"
In popular culture In the television series Dallas, the inherited neurofibromatosis of the Barnes family is a driving plot device, although the portrayal of the condition does leave something to be desired in terms of scientific fact.
The disease is also a pivotal plot element in the Icelandic crime novel Mýrin (Jar City) and the film version of it.
Gillian Anderson, who played Dana Scully on the X-Files, is a spokesperson and helps in the raising of money for neurofibromatosis, because her brother suffers from the disease.
Munya "Mony" Yassir, who was diagnosed with neurofibromatosis at 18 months, appeared in nine episodes of Degrassi: The Next Generation, in season 2.
Neurofibromatosis is mentioned in an episode of House as a possible diagnosis.
In 2010, MTV's True Life showed an episode entitled "I have NF".
In season 6 epiosde 13 on the show Nip/Tuck which was called "Joel Seabrook", Doctor Sean McNamera is talking on the phone and mentions a new treatment for people with Neurofibromatosis. The talk of the new treatment and the disease is again briefly mention again in episode 14 which was called "Shelia Carlton."
"
So here it is. I dont think it belongs back in the article but just so nobody thinks I omitted data here it is in discussion where it belongs. Dr. Persi (talk) 02:13, 14 December 2010 (UTC)
Wikipedia is not a directory
[edit]I have removed the following as it is simple a long list of research centers with no independent evidence of significance.
Foundations
[edit]Several national organizations provide support for those challenged by neurofibromatosis. Some include:
- Australia: NF Australia incorporating the Children's Tumour Foundation of Australia (a nonprofit charitable organisation supporting research and providing awareness, resources and support
- Little Frog Foundation (a nonprofit organization working providing information and resources for families dealing with NF1, NF2, and tumour-related neurofibromatosis in Australia)
- Belgium: NF KONTAKT.be (a nonprofit organization providing information and resources for families, Schools and Health Care workers dealing with NF1, NF2, and tumour-related neurofibromatosis in Belgium and providing awareness and support of Neurofibromatosis in Europe)
- Canada: The Neurofibromatosis Association of Quebec
- Canada: NF Society of Ontario
- France:
- The Neurofibromatosis and Recklinghausen Association
- Centre de Référence labellisé NEUROFIBROMATOSES
- United Kingdom: The Neuro Foundation
- United States:
- The Children's Tumor Foundation (CTF) (a nonprofit organization working towards finding a cure and improving care for individuals living with neurofibromatosis)
- Neurofibromatosis Inc. (a nonprofit organization working towards neurofibromatosis patient support)
- Neurofibromatosis Cafe (a nonprofit organization working providing patient education, awareness and support of Neurofibromatosis)
Academic Research and Clinical Centers
[edit]France
[edit]- At the Neurosurgery Clinic of the Hôpital Beaujon in Clichy, Hauts-de-Seine, and in collaboration with the Black Laboratory at Harvard University which focuses on meningioma research, Michel Kalamarides focuses on mouse modeling of NF2 meningioma.
United States
[edit]- California:
- House Ear Institute in Los Angeles is a CTF NFPC focussing on NF2 schwannoma and meningioma.
- The NF/Ras Pathway Clinic at UCSF Medical Center inSan Francisco. This is a CTF NFPC focussing on NF1 myeloid leukemia.
- Florida:
- The Wallace Lab andMuir Lab at the University of Florida inGainesville, Florida focus on the molecular study of benign Schwann cell tumors and the development of new therapies for NF1.
- The Neurofibromatosis Center at Miami Children's Hospital.
- Illinois: The Neurofibromatosis Program at University of Chicago Medical Center.
- Indiana: The Neurofibromatosis Clinic at Indiana University. This clinic has pioneered the use of Imatinib to treatneurofibromas.[1]
- Maryland: The Hopkins Comprehensive Neurofibromatosis Center at Johns Hopkins Hospital
- Massachusetts:
- The Center for Neurofibromatosis and Allied Disorders at Harvard Medical Schooland Massachusetts General Hospital. This is a CTF NFPC focussing on NF2 schwannoma and meningioma.
- Brigham and Women's Hospital at Harvard Medical School is a CTF NFPC focussing on NF1 malignant peripheral nerve sheath tumors.
- The Center for Human Genetics at Boston University School of Medicine provides genetic testing laboratory service for Neurofibromatosis type I and Legius syndrome. Testing includes DNA sequencing and Multiplex ligation-dependent probe amplification.
- Missouri: The Neurofibromatosis Center at St. Louis Children's Hospital.[2] This is a CTF NFPC focussing on NF1 optic pathway glioma. They maintain a comprehensivelist of current NF research studies.
- New Jersey: The Neurofibromatosis Center of New Jersey andInstitute of Genomic Medicine at University Hospital (Newark, New Jersey)
- New York:
- Ohio: The Cincinnati Neurofibromatosis Center at Cincinnati Children's Hospital Medical Center. This is a CTF NFPC focusing on NF1 plexiform neurofibromas. The Ratner Lab focuses on interactions between glial cells and axons during nervous system development and how those interactions go awry to lead to NF1 and NF2 conditions.
- Pennsylvania: The Neurofibromatosis Program atChildren's Hospital of Philadelphia
- Texas:
Drug Companies
[edit]The following drug companies are supporters of the Children's Tumor Foundation and are actively developing NF-related drugs:
Doc James (talk · contribs · email) (if I write on your page reply on mine) 09:16, 22 January 2013 (UTC)
- Hi User:Jmh649, The significance is that these are all places people with NF might turn to for help. Wikipedia is full of lists of all kinds. Is it OK with you if I put these lists in separate articles? Thanks, Erxnmedia (talk) 16:16, 17 September 2013 (UTC)
- I'm afraid, not. Wikipedia is not a repository of links and Wikipedia is not a directory. While Wikipedia has many lists, they should have distinct, objective, verifiable inclusion criteria, because Wikipedia is not an indiscriminate collection of information. Sorry.Novangelis (talk) 19:13, 17 September 2013 (UTC)
- OK, Novangelis, please nominate the following and similar pages for deleteion: List of art schools in Europe. In the case of Neurofibromatosis Clinics, I think it is fairly obvious what the criteria for inclusion is: They have "Neurofibromatosis Clinic" in the name. They are as notable as Art Schools in Austria because it is a rare disease, the clinics have special qualifications, and there are not that many of them. Also, you've definitely go to get rid of this thing: List of lists of lists. Erxnmedia (talk) 19:36, 17 September 2013 (UTC)
- We do not edit Wikipedia disruptively, just to make a point.Novangelis (talk) 22:56, 17 September 2013 (UTC)
- I try to keep main disease related article clear of cruft / undue content. No position on creating another page with this content. Doc James (talk · contribs · email) (if I write on your page reply on mine) 23:12, 17 September 2013 (UTC)
- We do not edit Wikipedia disruptively, just to make a point.Novangelis (talk) 22:56, 17 September 2013 (UTC)
NF article should be shorter with more focus in the branches
[edit]Proposal
[edit]"Neurofibromatoses in Clinical Practice" by Ferner, Huson and Evans give a breakdown of neurofibromatoses into NF1, NF2 and NCFC overlaps with NF1. To a large extent NF1 and NF2 are completely different diseases with different and mostly non-intersecting research. How do people feel about shortening this article to show to what extent NF1 and NF2 have common roots, show the diagnostic criteria that differentiate the two conditions, and then push any remaining details into the respective NF1, NF2 and NCFC articles? In particular the NF article has an NF1 picture and this has nothing to do with NF2 which is mostly focussed around hearing loss. I think it would make it easier for people who care about NF1 or NF2 in particular to have a shorter NF article which branches them more quickly to the content they will really care about. Erxnmedia (talk) 23:52, 17 September 2013 (UTC)
Action
[edit]OK, in the absence of any additional comment to the proposal, I have shortened the article so that it briefly describes the main NFs and leads readers to the branches for the details. This is mainly because the bulk of the article describes NF-1 and this will be confusing with someone with NF-2 or Schwannomatosis or something else. So I feel that brevity leads to better information in this case. Most if not all of the elided details in the article are in the branches. For future reference, here is what I ellided, so that it can be restored to the branches in case there are any ellided items that are not already in the branches:
xxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxx
Classification
[edit]Neurofibromatosis type 1 (NF 1)
[edit]Nneurofibromatosis type 1, also known as von Recklinghausen disease is a genetically-inherited disorder in which the nerve tissue grows tumors (neurofibromas) that may be benign and may cause serious damage by compressing nerves and other tissues. The disorder can affect many neural crest cell-derived nerve tissues (e.g., Schwann cells, melanocytes and endoneurial fibroblasts). Cellular elements from these cell types proliferate excessively throughout the body, forming tumors; melanocytes also function abnormally in this disease, resulting in disordered skin pigmentation and café au lait spots. The tumors may cause bumps under the skin, colored spots, skeletal problems, pressure on spinal nerve roots, and other neurological problems.[3][4]
The diagnosis of NF1 is made if any two of the following nine criteria are met:

- Two or more neurofibromas on or under the skin, or one plexiform neurofibroma (a large cluster of tumors involving multiple nerves); neurofibromas are the subcutaneous bumps characteristic of the disease, and increase in number with age.
- Freckling of the groin or the axilla (arm pit).
- Café au lait spots (pigmented, light brown macules located on nerves, with smooth edged, "coast of California"[5] birthmarks). Six or more measuring 5 mm in greatest diameter in prepubertal individuals and over 15 mm in greatest diameter in postpubertal individuals.
- Skeletal abnormalities, such as sphenoid dysplasia or thinning of the cortex of the long bones of the body (i.e. bones of the leg, potentially resulting in bowing of the legs)[3]
- Lisch nodules (hamartomas of iris), freckling in the iris
- Tumors on the optic nerve, also known as an optic glioma
- A first-degree relative (parent, sibling, or child) with NF-1 according to the preceding criteria.
NF-1 is the most common form of NF, accounting for up to 90% of all cases. NF 1 has a disorder frequency of 1 in 4,000, making it more common than neurofibromatosis type 2, with a frequency of 1 in 45,000 people.[6] It occurs following the mutation of neurofibromin 1 on chromosome 17q11.2; the large size of the NF1 gene (286kbp)[1] and presence of many homologous regions may predispose it to mutations. 100,000 Americans have neurofibromatosis. Neurofibromin is a tumor suppressor gene whose function is to inhibit the p21 ras oncoprotein.[6] In absence of this tumor suppressor's inhibitory control on the ras oncoprotein, cellular proliferation is erratic and uncontrolled, resulting in unbalanced cellular proliferation and tumor development.
Other complications that may be seen in individuals with NF-1 are:
- Scoliosis with or without kyphosis
- Macrocephaly in 30–50% of the pediatric population without any hydrocephalus[7]
- Epilepsy (seizures)
- Juvenile posterior lenticular opacity[3]
- Learning disabilities: Children with NF1 may have impaired cognitive skills and/or language difficulties. One common learning disability among children with NF1 is Attention Deficit/Hyperactivity Disorder (ADHD).[8]
- Larger than average head size: Children with NF1 often have a larger head and brain size than average.[9]
NF 1 also increases the risk of tumor development, particularly, gliomas and pheochromocytomas. Unlike NF 2, NF 1 is not associated with an increased risk for meningiomas.[10]
Neurofibromatosis type 2 (NF 2)
[edit]Neurofibromatosis type 2 (also called "central neurofibromatosis"[3]) is the result of mutation of the protein merlin (also known as "Neurofibromin 2" or "schwannomin"[3]) in chromosome 22q12. It accounts for only 10% of all cases of NF, and its frequency is lower than NF1. It is also caused by a mutation in a tumor suppressor gene NF2 (whose gene product is schwannomin or merlin). The normal function of merlin is not well understood.[6] The disorder manifests in the following fashion:
- bilateral acoustic neuromas (tumors of the vestibulocochlear nerve or cranial nerve 8 (CN VIII) also known as schwannoma), often leading to hearing loss. In fact, the hallmark of NF 2 is hearing loss due to acoustic neuromas around the age of twenty.
- The tumors may cause:
- headaches
- balance problems, and peripheral vertigo often due to schwannoma and involvement of the inner ear
- facial weakness/paralysis due to involvement or compression of the facial nerve (cranial nerve 7 or CN VII)
- patients with NF2 may also develop other brain tumors, as well as spinal tumors.
- deafness and tinnitus
NF 2 increases the risk of meningiomas and ependymomas.[6]
Schwannomatosis
[edit]Schwannomatosis — mutation in both chromosomes 17 and 22
- Multiple schwannomas occur.
- The schwannomas develop on cranial, spinal and peripheral nerves.
- Chronic pain, and sometimes numbness, tingling and weakness
- About 1/3 of patients have segmental schwannomatosis, which means the schwannomas are limited to a single part of the body, such as an arm, a leg or the spine.
- Unlike the other forms of NF, the schwannomas do not develop on vestibular nerves, and as a result, no loss of hearing is associated with schwannomatosis.
- Patients with schwannomatosis do not have learning disabilities related to the disorder.
One must keep in mind, however, that neurofibromatosis can occur in or affect any of the organ systems, whether that entails simply compressing them (from tumor growth) or in fact altering the organs in some fundamental way. This disparity in the disorder is one of many factors that makes it difficult to diagnose, and eventually find a prognosis for.
Other variants
[edit]- Neurofibromatosis type 3A: A rare genetic disorder characterized by areas of increased and decreased skin pigmentation and the development of many non-cancerous nerve and skin tumors some of which may eventually become malignant. The skin tumors tend to develop characteristically on the palms of the hands[11]
- Neurofibromatosis type 4 of Riccardi: A rare genetic disorder characterized by areas of increased and decreased skin pigmentation and the development of many non-cancerous nerve and skin tumors some of which may eventually become malignant.[12]
- Neurofibromatosis type 5 [citation needed]
Related disorders
[edit]The Neurofibromatoses are considered as RASopathies and as members of the neurocutaneous syndromes (phakomatoses).[4] In addition to the types of neurofibromatosis, the phakomatoses also include tuberous sclerosis, Sturge-Weber syndrome and von Hippel-Lindau disease. This grouping is an artifact of an earlier time in medicine, before the distinct genetic basis of each of these diseases was understood.
Signs and symptoms
[edit]Patients with neurofibromatosis can be affected in many different ways. Morbidity is often a result of plexiform neuromas, optic gliomas, or acoustic neuromas, but mortality can also be associated with malignant transformation of the neuromas, such as neurofibrosarcomas[3] (often there is a malignant transformation in less than 3% of the cases of NF1[6]). There is a high incidence of learning disabilities or cognitive deficit[3][7] in patients with NF, particularly NF-1, however severe retardation is not part of the syndrome. Because of the tumor generating nature of the disorder and its involvement of the nervous system and also because of early onset macrocephaly in the pediatric population, there is often an increased chance of development of epilepsy in those affected. Neurofibromatosis also increases the risk of leukemia particularly in children; Children with NF-1 have 200 to 500 times the normal risk of developing leukemia compared to the general population.[3] Since the tumors grow where there are nerves, they can also grow in areas that are visible, causing considerable social suffering for those affected. The tumors can also grow in places that can cause other medical issues that may require them to be removed for the patient's safety.[13] Affected individuals may need multiple surgeries (such as reduction surgery, or Gamma knife surgery), depending on where the tumors are located. For instance, those affected with NF 2 might benefit from a surgical decompression of the vestibular tumors to prevent deafness.[4]
Diagnosis
[edit]
Prenatal testing
[edit]Embryo
[edit]For embryos produced via in vitro fertilisation, it is possible via preimplantation genetic diagnosis (PGD) to screen for NF-1.[14]
"PGD has about 95–98% accuracy but requires that the partner with NF2 have a recognizable genetic mutation, which is only the case for about 60% of people with a clinical diagnosis of NF2. Having the initial genetic testing to determine if the mutation is recognizable takes approximately 6 months, and then preparing the probes for the PDG testing takes approximately another 6 months."[15]
PGD can not be used to detect Schwannomatosis, because the gene for it has not yet been identified.[16]
Fetus
[edit]Chorionic villus sampling or amniocentesis can be used:[17]
- To detect Neurofibromatosis type I.
- To detect Neurofibromatosis type II with 95% accuracy.
- Can not be used to detect Schwannomatosis, because the gene for it has not yet been identified.
Genetics
[edit]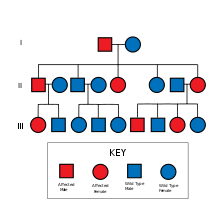
Neurofibromatosis type 1 is caused by mutation on chromosome 17q11.2, the gene product being neurofibromin 1 (a regulator of the GTPase activating enzyme (GAP)).[3][18] Neurofibromatosis type 2 is due to mutation on chromosome 22q, the gene product is merlin, a cytoskeletal protein.[3]
Both NF-1 and NF-2 are autosomal dominant disorders, meaning only one copy of the mutated gene need be inherited to pass the disorder. A child of a parent with NF-1 or NF-2 and an unaffected parent will have a 50–100% chance of inheriting the disorder, depending on whether the affected parent is heterozygous (Aa) or homozygous (AA) for the trait ("A" depicts the affected dominant allele, while "a" depics the recessive allele).
Complicating the question of heritability is the distinction between genotype and phenotype, that is, between the genetics and the actual manifestation of the disorder. In the case of NF1, no clear links between genotype and phenotype have been found, and the severity and the specific nature of the symptoms may vary widely among family members with the disorder. This is a good example of the phenomenon of variable expressivity: the differing severities of disease in different individuals with the same genotype.[19] In the case of NF-2, however, manifestations are similar among family members; a strong genotype-phenotype correlation is believed to exist.[19] Both NF-1 and NF-2 can also appear to be spontaneous de novo mutations, with no family history. These cases account for about one half of neurofibromatosis cases.[19]
Similar to polydactyly, NF is also an autosomally dominant mutation, that is not prevalent in the society. Neurofibromatosis-1 is found in approximately 1 in 2,500–3,000[6] live births (carrier incidence 0.0004, gene frequency 0.0002) and is more common than NF-2.
Pathophysiology
[edit]The gene affected in NF-1, is located on the long arm of the chromosome 17 (q11.2). It encodes for a protein called neurofibromin, otherwise known as a "tumor suppressor" protein. This protein is a negative regulator of the Ras kinase pathway (p21 oncoprotein).[20] Neurofibromatosis alters or weakens this protein (due to deletion, missense mutation, or nonsense mutations,[3]) allowing rapid, radical growth of cells all over the body, especially around the nervous system. The essential problem is the inability to inactivate GTP due to a defective GTP-ase (neurofibromin). This leads to the common symptoms for neurofibromatosis — clumpings of the tumors, called neurofibromas and schwannomas. Less is known about the NF-2 linked gene and its product, merlin. However, it is on the long arm of the chromosome 22q(11.1-13.1[3]) and codes for the protein.
Treatment
[edit]Because there is no cure for the condition itself, the only therapy for patients with neurofibromatosis is a program of treatment by a team of specialists to manage symptoms or complications. Surgery may be needed when the tumors compress organs or other structures. Less than 10% of people with neurofibromatosis develop cancerous growths; in these cases, chemotherapy may be successful.[21]
For families with NF, genetic screening and counselling is available.[22]
History
[edit]Neurofibromatosis (or von Recklinghausen disease[4]) was first described in 1882 by the German pathologist, Friedrich Daniel von Recklinghausen. As a young scientist, Recklinghausen was the student of the renowned Rudolf Virchow in Berlin. Recklinghausen was successful in generating some of the most descriptive medical observations of his time, making him the first person to describe and coin the term "hemachromatosis" (Hämochromatose, Tageblatt der Naturforschenden Versammlung). Recklinghausen is now known for his contributions to staining methods, and most importantly for his important paper on neurofibromatosis published in 1881, to honor Rudolf Virchow’s 25 year jubilee, in which he describes neurofibromatosis. Today he is recognized as a distinguished histopathologist, and a great scientist, he lends his name to the syndrome, which he himself elucidated.[23]
Notable cases
[edit]In May 2011, a case was reported in the United Kingdom in which a 15-month-old child who turned out to have Neurofibromatosis type I was misdiagnosed as being abused under the assumption that the mother had Münchausen syndrome by proxy, because the child gained weight while in the hospital and lost weight while at home.[24] The child was placed in foster care for 6 months and then returned to his parents after he was correctly diagnosed.
In January 2008, 32-year-old Huang Chuncai of China underwent a second operation to remove another 4.5 kg (9.9 lb) of tumor from his face. A previous operation removed 15 kg (33 lb) from what was originally a 23 kg (55.7 lb) tumor.[25][26]
In March 2007, the treatment of 30-year-old neurofibromatosis patient Pascal Coler of France ended after he had received what his doctors call the world's first successful full face transplant.[27][28]
In November 2006, there was an hour-long documentary on the British television network Channel 4 about Facing the World, an organization that helps children with severe facial disfigurements in developing countries. One of the children featured on the documentary was Arianto, an Indonesian boy who suffered from a severe form of neurofibroma resulting in hemifacial giganticism.
Also in that year, another documentary on BBC2 (edge of life) featured a neurofibromatosis case. On that documentary was a young teenager, Amit Ghose, who had decided for himself to have corrective surgery at the age of 14. In this case, the neurofibroma occurred on the face, resulting in the loss of sight in one eye and having to have it removed. This was a case of NF-2, resulting in the disfigurement of the one side of the face, while leaving the other side completely normal.
In 2012, surgeons removed a 200-pound tumor caused by neurofibromatosis from a Vietnamese man's leg; the tumor weighed twice as much as the rest of his body.[29]
Joseph Merrick, the Elephant Man, was once considered to have been affected with neurofibromatosis type I. It is likely, however, that Merrick suffered from the very rare Proteus syndrome. This has produced a common misconception that neurofibromatosis and the "Elephant Man disease" are one and the same.[30]
xxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxx Erxnmedia (talk) 22:35, 21 September 2013 (UTC)
References
[edit]- ^ "Gleevec Holds Potential As First Drug To Successfully Treat Neurofibromatosis, Scientists Report", Science Daily, October 31, 2008
- ^ "Washington University Neurofibromatosis Center receives Department of Defense grant to participate in NF Clinical Trials Consortium", July 1, 2007, Press release
- ^ a b c d e f g h i j k l Raphael Rubin, David S. Strayer (2008 Baltimore). Rubin's Pathology: Clinicopathologic Foundation of Medicine (5 ed.). Wolters Kluwer Health: Lippincot Williams & Wilkins. pp. 201–3. ISBN 978-0-7817-9516-6.
{{cite book}}: Check date values in:|date=(help) - ^ a b c d Conrad Fischer, Farshad Bagheri, Rajpal Manchandani, Richard Pinsker, Sudheer Chauhan, Parenkumar Patel, Mohammad Maruf, Dhaval Satani, Kaushik Doshi, Ayaz Alwani, Naveen Pathak, Craigh Thurm, Mohammad Babury, Mahendra C. Patel, Arthur Shalanov, Samir Sarkar, Sabiha Raouf, Jebun Nahar, Prakashkumar Patel (2010). Master the Board USMLE Step 2 CK. KAPLAN Medical. p. 287. ISBN 978-1-60714-653-7.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ William D James, Raj D Sheth, Nazanin Saedi (Jul 20, 2009). "Cafe Au Lait Spots". eMedicine from WebMD. Retrieved 13 December 2010.
{{cite journal}}: Cite journal requires|journal=(help)CS1 maint: multiple names: authors list (link) - ^ a b c d e f John Barone (2008). USMLE Step 1 Lecture Notes: Pathology. KAPLAN Inc. p. 57.
- ^ a b Steen RG, Taylor JS, Langston JW; et al. (2001). "Prospective evaluation of the brain in asymptomatic children with neurofibromatosis type 1: relationship of macrocephaly to T1 relaxation changes and structural brain abnormalities". AJNR Am J Neuroradiol. 22 (5): 810–7. PMID 11337320.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Mayo Clinic. (2013). Neurofibromatosis: symptoms. Mayoclinic.com Retrieved 13 June 2013.
- ^ Mayo Clinic. (2013). Neurofibromatosis: symptoms. www.mayoclinic.com Retrieved 13 June 2013.
- ^ Goutagny, S (September 2010). "Meningiomas and neurofibromatosis". Journal of neuro-oncology. 99 (3): 341–7. doi:10.1007/s11060-010-0339-x. PMID 20714782.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Health Grades Inc.(2013). "Neurofibfomatosis type 3A". Retrieved 12 June 2013.
- ^ Health Grades Inc. (2013). Neurofibromatosis, type 4, of Riccardi . Retrieved 12 June 2013.
- ^ Hayashi M, Chernov M, Tamura N, Yomo S, Ochiai T, Nagai M, Tamura M, Izawa M, Muragaki Y, Iseki H, Okada Y, Takakura K. (December 2010). "Gamma Knife surgery for abducent nerve schwannoma. Report of 4 cases". Journal of neurosurgery. 113: 136–43. doi:10.3171/2010.8.GKS10947. PMID 21121795.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "British couple successfully screens out genetic disorder using NHS-funded PGD" by Antony Blackburn-Starza, June 9, 2008, BioNews 461
- ^ NF2 Planned Parenthood: Current prenatal testing options
- ^ Schwannomatosis, by Susan Toomey MS, page 4
- ^ "Are there any prenatal tests for the neurofibromatoses?"
- ^ Fauci; et al. Harrison's Principles of Internal Medicine (Small textbook) (16 ed.). p. 2453.
{{cite book}}: Explicit use of et al. in:|author=(help) - ^ a b c Bruce R. Korf, Allan E. Rubenstein (2005). Neurofibromatosis: a handbook for patients, families, and health care professionals (2 ed.). Thieme. ISBN 978-1-58890-301-3.
- ^ Feldkamp MM, Angelov L, Guha A (1999). "Neurofibromatosis type 1 peripheral nerve tumors: aberrant activation of the Ras pathway". Surg Neurol. 51 (2): 211–8. doi:10.1016/S0090-3019(97)00356-X. PMID 10029430.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Janet M. Torpy, Alison E. Burke, MA, Richard M. Glass (2008). "JAMA patient page: Neurofibromatosis". JAMA: the Journal of the American Medical Association. 300 (3): 352–352. doi:10.1001/jama.300.3.352.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Trisha Macnair, Rob Hicks. "Neurofibromatosis". British Broadcasting Company (BBC) — MMX. Retrieved 13 December 2010.
- ^ Friedrich Daniel von Recklinghausen at Who Named It?
- ^ "Billingham mum speaks of joy as baby is returned to her", by Lindsay Bruce, May 10, 2011Evening Gazette (Teesside)
- ^ Dan Childs. "50-Pound Face Tumor: One Man's Nightmare". ACB News. Retrieved 2008-01-23.
- ^ Radford, S. (2008-01-11). "Chinese man has surgery for 10 kg face tumour". The Daily Telegraph. London. Retrieved 2008-01-29.
- ^ Watt, Nick (2008-03-25). "World's First Full Face Transplant Hailed". abcnews.go.com. Retrieved 2008-03-25.
- ^ Franklin, Katie (2008-03-25). "Man has first full-face transplant". London: telegraph.co.uk. Retrieved 2008-03-25.
- ^ "Vietnam surgery removes tumor twice man's weight". CNN. 2012-01-09.
- ^ Legendre CM, Charpentier-Côté C, Drouin R, Bouffard C (2011). "Neurofibromatosis type 1 and the "elephant man's" disease: the confusion persists: an ethnographic study". PLoS ONE. 6 (2): e16409. doi:10.1371/journal.pone.0016409. PMC 3036577. PMID 21347399.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link)
Is there anything from this abandoned draft that would be worth incorporating here? Thanks, Calliopejen1 (talk) 23:51, 20 May 2015 (UTC)
I myself have Neurofibromatosis(NF) and some of the information actually kind of bothers me there is a lot of wrong or not entirely correct information in this article. Maybe research more and find more credible sources to help correct the incorrect information. Cite sources and really add onto the article. It would help improve the article a lot.( TDoubek (talk) 15:35, 6 October 2015 (UTC)TDoubek)
Text
[edit]This text "In NF1 the tumors are neurofibromas (tumors of the peripheral nerves), while in NF2 and schwannomatosis tumors of Schwann cells are more common"
Ref says "The most common nerve-associated tumors in NF1 are neurofibromas (tumors of the peripheral nerves), whereas schwannomas (tumors that begin in Schwann cells that help form the myelin sheath) are most common in NF2 and schwannomatosis."[2]
Not sure what is wrong with this? Doc James (talk · contribs · email) 17:00, 14 April 2018 (UTC)
- Still supported by "The most common nerve-associated tumors in NF1 are neurofibromas (tumors of the peripheral nerves), whereas schwannomas (tumors that begin in Schwann cells that help form the myelin sheath) are most common in NF2 and schwannomatosis. " https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Neurofibromatosis-Fact-Sheet
Video illustration
[edit]A really horribly poignant case of neurofibromatosis, then 47-year-old Shadot Hossain, a married father of three children in Shajadpur, Bangladesh, is shown in a Born Different video sequence. MaynardClark (talk) 00:10, 13 June 2018 (UTC)
- indeed(facebook however cant be used as RS)--Ozzie10aaaa (talk) 01:38, 13 June 2018 (UTC)
- No, but in the talk sectrion, we can have a better idea of how bad that condition can be, since photos of the condition (shown in the article) show a cosmetically and operationally problematic condition, but hardly anything as debilitating as it can become. Maybe the could/should be some sentnence (or section) on the range of gravity of the diagnoses, or (acceptable) documentation the worst cases observed, etc. The Facebook video was drawn from somewhere other than Facebook. MaynardClark (talk) 02:32, 13 June 2018 (UTC) Shadot Hossain was going blind from the tumorous growths, and crowdfunding helped pay for his travel to the National Institute of Neuro-Sciences & Hospital in Dhaka, where one or more surgeons who could do corrective, rehabilitative surgery with this rare, unusual patient.[1]— Preceding unsigned comment added by MaynardClark (talk • contribs)
- well in that case(reference) the answer is yes, it should be incorporated, I agree--Ozzie10aaaa (talk) 10:10, 13 June 2018 (UTC)
- No, but in the talk sectrion, we can have a better idea of how bad that condition can be, since photos of the condition (shown in the article) show a cosmetically and operationally problematic condition, but hardly anything as debilitating as it can become. Maybe the could/should be some sentnence (or section) on the range of gravity of the diagnoses, or (acceptable) documentation the worst cases observed, etc. The Facebook video was drawn from somewhere other than Facebook. MaynardClark (talk) 02:32, 13 June 2018 (UTC) Shadot Hossain was going blind from the tumorous growths, and crowdfunding helped pay for his travel to the National Institute of Neuro-Sciences & Hospital in Dhaka, where one or more surgeons who could do corrective, rehabilitative surgery with this rare, unusual patient.[1]— Preceding unsigned comment added by MaynardClark (talk • contribs)
