Tafazzin
| Tafazzin | |
|---|---|
| Identifiers | |
| Symbol | TAZ |
| InterPro | IPR000872 |
| Membranome | 459 |
Tafazzin is a protein that in humans is encoded by the TAFAZZIN gene.[5] Tafazzin is highly expressed in cardiac and skeletal muscle, and functions as a phospholipid-lysophospholipid transacylase (it belongs to phospholipid:diacylglycerol acyltransferases).[6][7] It catalyzes remodeling of immature cardiolipin to its mature composition containing a predominance of tetralinoleoyl moieties.[8] Several different isoforms of the tafazzin protein are produced from the TAFAZZIN gene. A long form and a short form of each of these isoforms is produced; the short form lacks a hydrophobic leader sequence and may exist as a cytoplasmic protein rather than being membrane-bound. Other alternatively spliced transcripts have been described but the full-length nature of all these transcripts is not known. Most isoforms are found in all tissues, but some are found only in certain types of cells.[9][5] Mutations in the TAFAZZIN gene have been associated with mitochondrial deficiency, Barth syndrome, dilated cardiomyopathy (DCM), hypertrophic DCM, endocardial fibroelastosis, left ventricular noncompaction (LVNC), breast cancer, papillary thyroid carcinoma, non-small cell lung cancer, glioma, gastric cancer, thyroid neoplasms, and rectal cancer.[5][10][11][12]
It is important to note that the TAZ gene was frequently confused with a protein called TAZ (transcriptional coactivator with PDZ-binding motif, a 50 kDA protein). which is a part of the Hippo pathway and entirely unrelated to the gene of interest. The Hippo pathway TAZ protein has an official gene symbol of WWTR1.
Structure
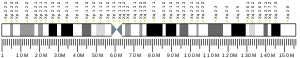
[edit]The TAFAZZIN gene is located on the q arm of chromosome X at position 28 and it spans 10,208 base pairs.[5] The TAFAZZIN gene produces a 21.3 kDa protein composed of 184 amino acids.[13][14] The structure of the encoded protein has been found to differ at their N terminus and the central region, which are two functionally notable regions. A 30 residue hydrophobic stretch at the N terminus may function as a membrane anchor, which does not exist in the shortest forms of tafazzins. The second region is a variable exposed loop located between amino acids 124 and 195 in the central region. This hydrophilic region is known to interact with other proteins. TAZ has no known resemblance to other proteins.[15] The half-life of tafazzin is just 3–6 hours, considerably shorter than most mitochondrial proteins, which may explain research difficulties in studying its structure.[16]
The putative phospholipid-binding site, which is the active site of Tafazzin, is a 57 amino acid cleft with two open ends and positively charged residues.[17] In addition, tafazzin localizes to the membrane leaflets facing the intermembrane space (IMS), which is crucial for remodeling.[18][19] Tafazzin differs from phospholipases in that it contains a conserved histidine residue, His-77, as part of the conserved HX4D motif seen in acyltransferases. This motif is responsible for facilitating the Asp-His dyad mechanism seen in many serine proteases.[20] Many unique forms of tafazzin have been identified, with lengths from 129 to 292 amino acids.[15] Tafazzin has at least four different isoforms. It has a molecular weight around 35 kDa but may also appear in lower molecular weights due to species differences in isoform expression. Seven functional classes of TAFAZZIN mutations have been classified based on the pathogenic loss-of-function mechanisms of each mutation.[21]
The TAFAZZIN gene contains two peptides independent of its active site for directing the protein to the mitochondria, forming residues 84–95 in exon 3 and residues 185–200 in exon 7/8 targets.[22] Tafazzin localizes with peripheral association to membrane leaflets between the inner mitochondrial membrane (IMM) and outer mitochondrial membrane (OMM), facing the intermembrane space (IMS).[18][19] Tafazzin's characteristic interfacial anchoring is achieved by its hydrophobic sequence from residues 215–232.[23] Finally, the translocase of the outer membrane (TOM) and the translocase of the inner membrane (TIM) mediates tafazzin's movement and insertion into the OMM and anchoring to IMM.[23]
Function
[edit]The TAFAZZIN gene provides instructions for producing a protein called tafazzin, which is localized to mitochondria, the energy-producing centers of cells. Tafazzin transacylase activity is responsible for cardiolipin remodeling, critical to maintaining mitochondrial inner membrane structure and function. It also has unique acyl specificity and membrane curvature sensing capabilities.[24]
Transacylase (remodeling)
[edit]After its synthesis, cardiolipin cannot exert its proper functions until it is actively remodeled. Tafazzin, an acyl-specific transferase, catalyzes the acyl transfer reaction between phospholipids and lysophospholipids in a CoA-independent manner. The remodeling process of cardiolipin involves reaching a final acyl composition that is primarily linoleoyl residues.[7][25] TAZ interacts with an immature cardiolipin by adding the fatty acid linoleic acid, which catalyzes the remodeling of the cardiolipin. The remodeling is achieved by transacylation or the deacylation-reacylation cycle. The deacylation-reacylation cycle, also known as the Lands cycle, begins with deacylation mediated by phospholipase Cld1 to form monolysocardiolipin (MLCL).[26] MLCL is reacylated by tafazzin in a single-step reaction which transfers a linoleic acid group from phosphatidylcholine (PC), completing the CL deacylation-reacylation cycle.[7][27] In contrast, transacylation involves the transfer of a linoleic acid group from phosphatidylcholine (PC) to MLCL. Such enzymatic activity forms lyso-PC and CL, and enriches the specific acyl chain of cardiolipin. The process has been shown to be specific for linoleoyl-containing PC. Such remodeling processes converts cardiolipin into a mature composition that contains a predominance of tetralinoleoyl moieties. CL remodeling in mammals requires additional enzymes, such as monolysocardiolipin acyltransferase (MLCLAT), acyl-CoA:lysocardiolipin acyltransferase (ALCAT), and phospholipase.[28] The process enables the proper function of cardiolipin.[8][9][29]
Acyl specificity and sensing curvature
[edit]Tafazzin in CL remodeling has been shown to have a clear preference for linoleoyl-containing PC in forming mature CL.[30] This specificity leads a mature composition of CL that contains a predominance of tetralinoleoyl moieties, which leads to the enrichment of tetralinoleoyl-cardiolipin (CL4).[29] The preference for lineoyl groups has been reported to be ten times greater than that of oleoyl groups and twenty times greater than that of arachidonoyl groups.[7] Conflicting explanations for this preference have included causation from energy minimization with influences by the surrounding microenvironment, known as the thermodynamic remodeling hypothesis,[31] or the inherent enzymatic preference of tafazzin for specific acyl residues.[19]
Tafazzin and cardiolipin in mitochondrial structure and function
[edit]Cardiolipin is a complex glycerophospholipid which contains four acyl groups linked to three glycerol moietie localized in the mitochondrial inner membrane. These acyl groups include oleic acid and linoleic acid. Due to this composition, cardiolipin exhibits a conical structure, which allows for membrane curvature called cristae. Further, CL plays important roles in oxidative phosphorylation by stabilizing the chain complexes with its linkages between acyl chains,[29] binding to the c-rings of ATP synthase for proper function,[32] maintaining respiratory chain supercomplex formation with proteins localized in the inner mitochondrial matrix including ATP/ADP translocase, pyruvate carrier, carnitine carrier, and all of the respiratory chain complexes (I, III, IV, V).[33][34][35] Cardiolipin also facilitates proton trapping in the intermembrane space to aid ATP synthase in channeling protons into the mitochondrial matrix. Properly formed CL is critical in maintaining mitochondrial shape, energy production, and protein transport within cells,[9] and remodeling by tafazzin aids in removing and replacing acyl chains damaged by oxidative stress.[36] During apoptosis and similar processes, CL is known to act as a platform for proteins and other machinery involved with its interactions with members of the Bcl-2 family, caspases, Bid, Bax, and Bak.[37]
Clinical significance
[edit]Mutations in the TAFAZZIN gene have been associated with a number of mitochondrial deficiencies and associated disorders including Barth syndrome, dilated cardiomyopathy (DCM), hypertrophic DCM, endocardial fibroelastosis, and left ventricular noncompaction (LVNC).[5] TAFAZZIN has also been associated with various cancers, including breast cancer, papillary thyroid carcinoma and non-small cell lung cancer, glioma, gastric cancer, thyroid neoplasms, and rectal cancer.[10][11][12]
Barth syndrome
[edit]Barth syndrome (BTHS) is an X-linked disease caused by mutations in the TAFAZZIN gene.[38] More than 160 mutations in the TAFAZZIN gene have been linked to this disease. It is a rare disease, found in 1 out of every 300,000 to 400,000 live births, though it is widely known that the disease is underdiagnosed.[39][40] Although BTHS occurs almost exclusively in males, there has been one identified case of BTHS in a female patient.[41] Tafazzin is responsible for remodeling of a phospholipid cardiolipin (CL),[42] the signature lipid of the mitochondrial inner membrane. TAFAZZIN gene mutations that cause Barth syndrome result in the production of tafazzin proteins with little or no function. As a result, linoleic acid is not added to cardiolipin, which disrupts normal mitochondrial shape and function, including energy production and protein transport. Barth syndrome patients exhibit defects in cardiolipin metabolism, including aberrant cardiolipin fatty acyl composition, accumulation of monolysocardiolipin (MLCL), and reduced total cardiolipin levels.[43][44] This may lead to acute metabolic decompensation and sudden death. Tissues with high energy demands, such as the heart and other muscles, are most susceptible to cell death due to reduced energy production in mitochondria and protein transport.[citation needed]
Additionally, affected white blood cells have abnormally shaped mitochondria, which could impair their ability to grow (proliferate) and mature (differentiate), leading to a weakened immune system and recurrent infections. Dysfunctional mitochondria likely lead to other signs and symptoms of Barth syndrome.[9]
Phenotypes of Barth Syndrome encompass a wide range, with cardiovascular, musculoskeletal, neurological, metabolic, and hematologic consequences.[45][46][47] Common clinical manifestations include:[9][38]
- dilated cardiomyopathy (enlarged and weakened heart)
- muscle weakness
- recurrent infections
- short stature
- endocardial fibroelastosis
- growth retardation
- neutropenia
- organic aciduria (3-methylglutaconic acid)
Additional features include hypertrophic cardiomyopathy, isolated noncompaction of left ventricular myocardium (INVM), ventricular arrhythmia, motor delay, poor appetite, fatigue and exercise intolerance, hypoglycemia, lactic acidosis, hyperammonemia, and dramatic late catch-up growth after growth delay throughout childhood.[38]
A c.348C>T mutation resulted in dilated cardiomyopathy with noncompaction of the ventricular myocardium.[48] A patient with a frame shift mutation of c.227delC displayed symptoms of neutropenia, cardiomegaly, and other common symptoms of Barth syndrome.[49] Another c.C153G mutation resulted in severe metabolic acidosis, cardiomegaly, and other major symptoms of Barth syndrome.[50]
There is no known cure for BTHS, and treatment of BTHS is convoluted and delayed due to the disease's varying phenotypes and its sheer complexity.[40] Thus, many treatments focus on cardiovascular and metabolic disorders, rather than treating the symptom itself. Elamipretide, an agent which protects CL from oxidative damage to maintain mitochondrial cristae and oxidative phosphorylation, is currently being tested in clinical trials.[51][52] Further, dietary fatty acids have been used to enhance bioenergetics and cardiac function in BTHS.[53] However, severe manifestations of the symptoms in BTHS patients require heart transplantation. Statistics show 9 out of 73 (12%) surviving patients who have undergone cardiac transplantation at the last update.[54][47] Heart transplantation in BTHS patients has generally been successful.[47]
Cardiovascular pathology
[edit]Cardiomyopathy is a prominent feature of Barth syndrome. The change in acyl chain composition and lipid peroxidation caused by defective tafazzin can cause defective sarcomeric action, which may lead to an insufficient power stroke, severely weakened tissue, enlarged left ventricle, partial or incomplete contraction, and decreased ejection volume. Such consequences contribute to the cardiomyopathic phenotypes of Barth syndrome, marked by a weakened heart and diminished contractility.[35][55] Alternatively, reactive oxygen species (ROS) has been suggested as the primary cause of cardiovascular impairments in BTHS.[56]
Cardiomyopathy in BTHS is exhibited at varying levels. A cohort study of BTHS patients showed 41.5% of all diagnosed cardiomyopathies in the range from birth to one month of age, and 95% exhibited a history of cardiomyopathy.[54] Furthermore, there have been cases with mild or late-onset cardiomyopathies, such as two infantile patients without cardiomyopathic phenotypes at the time of diagnosis.[57] Cardiomyopathy in Barth syndrome is primarily exhibited in multiple forms, including dilated cardiomyopathy (DCM), left ventricular condition in which the heart becomes weakened and enlarged, and therefore cannot pump blood efficiently. The resulting decrease in blood flow can lead to swelling in the legs and abdomen, fluid in the lungs, and an increased risk of blood clots.[9] Some mutations in the TAFAZZIN gene cause dilated cardiomyopathy without the other features of Barth syndrome. LVNC is a condition in which the left ventricle, characterized by a spongy structure on the ventricular wall, exhibits prominent trabeculations and deep intertrabecular recesses.[58] INVM occurs when the lower left chamber of the heart (left ventricle) does not develop correctly. In INVM, the heart muscle is weakened and cannot pump blood efficiently, frequently causing heart failure.[59][35] Abnormal heart rhythms (arrhythmias) can also occur.[citation needed]
Musculoskeletal pathology
[edit]Musculoskeletal pathology is exhibited in varying forms in BTHS patients. A common phenotype is both generalized and local weakness. Weakness is exhibited as overt muscle weakness and increased exertional fatigue due to skeletal myopathy. It worsens when present with the cardiovascular symptoms of Barth syndrome.[60] Additional symptoms of musculoskeletal pathology include hypotonia, delayed motor development, short stature, and facial dysmorphia in varying degrees.[61] Furthermore, it has been shown that a downshift in weight, length, and height relative to the normal population is exhibited in BTHS patients.[citation needed]
Treatment for developmental delays have included cornstarch supplementation as an alternative source of glucose.[47] Metabolic deficiencies have been treated by oral arginine and carnitine supplementation, which has been shown to ameliorate cardiac function and muscle weakness in some patients.[62][63][64] However, no formal assessment of the utility of carnitine and arginine supplementation has been published, and its uses have only been effective in patients with specific deficiencies.[62][64]
Neurological pathology
[edit]Cognitive impairments are common in BTHS patients in varying degrees. While a higher incidence of cognitive impairment[65] and mild learning and speech difficulties[54] are often manifested, many BTHS patients have also displayed normal cognitive abilities.[61] This shows the limited neurologic involvement in BTHS, despite tafazzin's crucial roles in brain mitochondrial respiration and normal cognitive function.[66] One study has shown that the brain has a distinct CL composition, with more diverse and less tetralinoleoyl-dependent CL. This composition diminishes the need for CL remodeling, resulting in a less tafazzin-dependent composition.[29] Another study found that the brain has a higher concentration of saturated acyl chains.[67] Finally, the brain has a higher ROS scavenging capability, which allows the circumvention of the harmful effects of ROS.[66] These findings explain the neurological phenotypes in BTHS patients.[68]
Metabolic disorders
[edit]Metabolic disorders in BTHS are exhibited in the form of 3-methylglutaconic aciduria (3-MGA), a condition characterized by increased levels of organic acids in urine, including 3‐methylglutaconic acid, 3‐methylglutaric acid, and 2‐ethyl-hydracrylic acid.[69] While 3-MGA is largely excreted in BTHS patients, some patients have been found to have normal levels of organic acids in urine.[70] Treatment of 3-MGA and metabolic deficiencies have included riboflavin or coenzyme Q10, which have shown significant improvement in patients.[69]
Hematologic pathology
[edit]The major hematologic pathology for BTHS patients is neutropenia, a condition characterized by a decline in total number of neutrophils in circulation with an increase in monocytes and eosinophils and no fluctuations in lymphocytes.[47] Presentation of neutropenia varies from mild to severe, cyclical to non-cyclical, and intermittent to chronic.[71] An absolute neutrophil count of < 500/μL, defined as severe chronic neutropenia (SCN), is the most deleterious form.[72]
Cancer
[edit]TAFAZZIN has been found to be highly expressed in gastric cancer cells resistant to cisplatin. This resistance was identified to be due to the acquired ability of the cancer cells to undergo epithelial-mesenchymal transition (EMT). The findings that TAFAZZIN is involved in inducing EMT as well as its high levels in these cancer cells may point to its involvement in gastric cancer.[10][11] TAFAZZIN overexpression has been linked to rectal cancer,[73] prostate cancer,[74] thyroid neoplasm,[75] and cervical cancer.[12] In a study of 140 Swedish rectal cancer patients, TAFAZZIN overexpression was associated with an increase in the expression of oncogenes (FXYD-3 and Livin). It was also found to enhance cell anti-apoptosis response and abnormal cell growth and was even found to be an indicator of rectal cancer's stage, type, and progression.[73] Additionally, the levels of TAFAZZIN were connected to the radiotherapy response of the patients, potentially offering insight into cancer recurrence in patients.[73] A potential link between PI3K and TAFAZZIN indicates a possible association between PI3K signaling and TAFAZZIN as both were highly elevated in PTEN mutant cancer cells.[10] In prostate cancer, CL, which is remodeled by tafazzin, was shown to have high palmitoleic acid content, which was found to have the ability to stimulate prostate cancer cell proliferation and reduce the rate of apoptosis.[74] In thyroid neoplasm, TAFAZZIN allows follicular adenomas to be distinguished from follicular carcinomas,[75] while in cervical cancer tafazzin levels increased from normal tissue, to squamous intraepithelial lesions, to squamous cervical carcinoma. Based on studies of cervical cancer progression, it is believed that TAFAZZIN may induce cancer by inhibiting apoptosis and promoting cancer cell growth, viability, and tumorigenesis.[12]
Interactions
[edit]Tafazzin has been shown to have protein-protein interactions with the following and more.[76][38]
History
[edit]The protein was discovered in 1996 by Italian scientists Silvia Bione et al., after long and intensive work.[15] Owing to the complex procedure required for the identification of tafazzin, the protein was named after Tafazzi, an Italian comedy character played by Giacomo Poretti who enthusiastically beats his groin with a plastic bottle, this as a symbol of masochism for the strenuous will to find it by the group of researchers.[77]
Notes
[edit]
The 2019 version of this article was updated by an external expert under a dual publication model. The corresponding academic peer reviewed article was published in Gene and can be cited as: Anders O Garlid; Calvin T Schaffer; Jaewoo Kim; Hirsh Bhatt; Vladimir Guevara-Gonzalez; Peipei Ping (21 October 2019). "TAZ encodes tafazzin, a transacylase essential for cardiolipin formation and central to the etiology of Barth syndrome". Gene. Gene Wiki Review Series. 726: 144148. doi:10.1016/J.GENE.2019.144148. ISSN 0378-1119. PMC 7646589. PMID 31647997. Wikidata Q81446954. |
References
[edit]- ^ a b c GRCh38: Ensembl release 89: ENSG00000102125 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000009995 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ a b c d e "TAFAZZIN tafazzin, phospholipid-lysophospholipid transacylase [ Homo sapiens (human) ]".
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ Xu Y, Zhang S, Malhotra A, Edelman-Novemsky I, Ma J, Kruppa A, et al. (October 2009). "Characterization of tafazzin splice variants from humans and fruit flies". The Journal of Biological Chemistry. 284 (42): 29230–9. doi:10.1074/jbc.M109.016642. PMC 2781466. PMID 19700766.
- ^ a b c d Xu Y, Malhotra A, Ren M, Schlame M (December 2006). "The enzymatic function of tafazzin". The Journal of Biological Chemistry. 281 (51): 39217–24. doi:10.1074/jbc.M606100200. PMID 17082194.
- ^ a b Acehan D, Vaz F, Houtkooper RH, James J, Moore V, Tokunaga C, et al. (January 2011). "Cardiac and skeletal muscle defects in a mouse model of human Barth syndrome". The Journal of Biological Chemistry. 286 (2): 899–908. doi:10.1074/jbc.M110.171439. PMC 3020775. PMID 21068380.
- ^ a b c d e f "TAZ". Genetics Home Reference. NCBI.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ a b c d Huang W, Lv X, Liu C, Zha Z, Zhang H, Jiang Y, et al. (July 2012). "The N-terminal phosphodegron targets TAZ/WWTR1 protein for SCFβ-TrCP-dependent degradation in response to phosphatidylinositol 3-kinase inhibition". The Journal of Biological Chemistry. 287 (31): 26245–53. doi:10.1074/jbc.M112.382036. PMC 3406709. PMID 22692215.
- ^ a b c Ge L, Li DS, Chen F, Feng JD, Li B, Wang TJ (July 2017). "TAZ overexpression is associated with epithelial-mesenchymal transition in cisplatin-resistant gastric cancer cells". International Journal of Oncology. 51 (1): 307–315. doi:10.3892/ijo.2017.3998. PMID 28534974.
- ^ a b c d Chen M, Zhang Y, Zheng PS (2017). "Tafazzin (TAZ) promotes the tumorigenicity of cervical cancer cells and inhibits apoptosis". PLOS ONE. 12 (5): e0177171. Bibcode:2017PLoSO..1277171C. doi:10.1371/journal.pone.0177171. PMC 5425199. PMID 28489874.
- ^ Zong NC, Li H, Li H, Lam MP, Jimenez RC, Kim CS, et al. (October 2013). "Integration of cardiac proteome biology and medicine by a specialized knowledgebase". Circulation Research. 113 (9): 1043–53. doi:10.1161/CIRCRESAHA.113.301151. PMC 4076475. PMID 23965338.
- ^ "TAZ Tafazzin". Cardiac Organellar Protein Atlas Knowledgebase (COPaKB). Archived from the original on 2018-08-25. Retrieved 2018-08-24.
- ^ a b c Bione S, D'Adamo P, Maestrini E, Gedeon AK, Bolhuis PA, Toniolo D (April 1996). "A novel X-linked gene, G4.5. is responsible for Barth syndrome". Nature Genetics. 12 (4): 385–9. doi:10.1038/ng0496-385. PMID 8630491. S2CID 23539265.
- ^ Xu Y, Malhotra A, Claypool SM, Ren M, Schlame M (March 2015). "Tafazzins from Drosophila and mammalian cells assemble in large protein complexes with a short half-life". Mitochondrion. 21: 27–32. doi:10.1016/j.mito.2015.01.002. PMC 4693151. PMID 25598000.
- ^ Hijikata A, Yura K, Ohara O, Go M (June 2015). "Structural and functional analyses of Barth syndrome-causing mutations and alternative splicing in the tafazzin acyltransferase domain". Meta Gene. 4: 92–106. doi:10.1016/j.mgene.2015.04.001. PMC 4412953. PMID 25941633.
- ^ a b Gawrisch K (October 2012). "Tafazzin senses curvature". Nature Chemical Biology. 8 (10): 811–2. doi:10.1038/nchembio.1068. PMC 3478944. PMID 22987008.
- ^ a b c Abe M, Hasegawa Y, Oku M, Sawada Y, Tanaka E, Sakai Y, Miyoshi H (July 2016). "Mechanism for Remodeling of the Acyl Chain Composition of Cardiolipin Catalyzed by Saccharomyces cerevisiae Tafazzin". The Journal of Biological Chemistry. 291 (30): 15491–502. doi:10.1074/jbc.M116.718510. PMC 4957036. PMID 27268057.
- ^ Tang Y, Xia H, Li D (2018). "Membrane Phospholipid Biosynthesis in Bacteria". In Cao Y (ed.). Advances in Membrane Proteins. Springer Singapore. pp. 77–119. doi:10.1007/978-981-13-0532-0_4. ISBN 9789811305313.
- ^ Whited K, Baile MG, Currier P, Claypool SM (February 2013). "Seven functional classes of Barth syndrome mutation". Human Molecular Genetics. 22 (3): 483–92. doi:10.1093/hmg/dds447. PMC 3606006. PMID 23100323.
- ^ Dinca AA, Chien WM, Chin MT (January 2018). "Identification of novel mitochondrial localization signals in human Tafazzin, the cause of the inherited cardiomyopathic disorder Barth syndrome". Journal of Molecular and Cellular Cardiology. 114: 83–92. doi:10.1016/j.yjmcc.2017.11.005. PMC 5801207. PMID 29129703.
- ^ a b Herndon JD, Claypool SM, Koehler CM (December 2013). "The Taz1p transacylase is imported and sorted into the outer mitochondrial membrane via a membrane anchor domain". Eukaryotic Cell. 12 (12): 1600–8. doi:10.1128/EC.00237-13. PMC 3889572. PMID 24078306.
- ^ Epand RM, D'Souza K, Berno B, Schlame M (January 2015). "Membrane curvature modulation of protein activity determined by NMR". Biochimica et Biophysica Acta (BBA) - Biomembranes. 1848 (1 Pt B): 220–8. doi:10.1016/j.bbamem.2014.05.004. PMID 24835017.
- ^ Minkler PE, Hoppel CL (April 2010). "Separation and characterization of cardiolipin molecular species by reverse-phase ion pair high-performance liquid chromatography-mass spectrometry". Journal of Lipid Research. 51 (4): 856–65. doi:10.1194/jlr.D002857. PMC 2842139. PMID 19965604.
- ^ Beranek A, Rechberger G, Knauer H, Wolinski H, Kohlwein SD, Leber R (April 2009). "Identification of a cardiolipin-specific phospholipase encoded by the gene CLD1 (YGR110W) in yeast". The Journal of Biological Chemistry. 284 (17): 11572–8. doi:10.1074/jbc.M805511200. PMC 2670162. PMID 19244244.
- ^ Schlame M (March 2013). "Cardiolipin remodeling and the function of tafazzin". Biochimica et Biophysica Acta (BBA) - Molecular and Cell Biology of Lipids. 1831 (3): 582–8. doi:10.1016/j.bbalip.2012.11.007. PMID 23200781.
- ^ Ye C, Shen Z, Greenberg ML (April 2016). "Cardiolipin remodeling: a regulatory hub for modulating cardiolipin metabolism and function". Journal of Bioenergetics and Biomembranes. 48 (2): 113–23. doi:10.1007/s10863-014-9591-7. PMC 4449329. PMID 25432572.
- ^ a b c d Houtkooper RH, Turkenburg M, Poll-The BT, Karall D, Pérez-Cerdá C, Morrone A, et al. (October 2009). "The enigmatic role of tafazzin in cardiolipin metabolism". Biochimica et Biophysica Acta (BBA) - Biomembranes. 1788 (10): 2003–14. doi:10.1016/j.bbamem.2009.07.009. PMID 19619503.
- ^ Schlame M, Xu Y, Ren M (March 2017). "The Basis for Acyl Specificity in the Tafazzin Reaction". The Journal of Biological Chemistry. 292 (13): 5499–5506. doi:10.1074/jbc.M116.769182. PMC 5392692. PMID 28202545.
- ^ Schlame M, Acehan D, Berno B, Xu Y, Valvo S, Ren M, et al. (October 2012). "The physical state of lipid substrates provides transacylation specificity for tafazzin". Nature Chemical Biology. 8 (10): 862–9. doi:10.1038/nchembio.1064. PMC 3699345. PMID 22941046.
- ^ Mehdipour AR, Hummer G (August 2016). "Cardiolipin puts the seal on ATP synthase". Proceedings of the National Academy of Sciences of the United States of America. 113 (31): 8568–70. Bibcode:2016PNAS..113.8568M. doi:10.1073/pnas.1609806113. PMC 4978257. PMID 27439859.
- ^ Hoffmann B, Stöckl A, Schlame M, Beyer K, Klingenberg M (January 1994). "The reconstituted ADP/ATP carrier activity has an absolute requirement for cardiolipin as shown in cysteine mutants". The Journal of Biological Chemistry. 269 (3): 1940–4. doi:10.1016/S0021-9258(17)42117-X. PMID 8294444.
- ^ Haines TH, Dencher NA (September 2002). "Cardiolipin: a proton trap for oxidative phosphorylation". FEBS Letters. 528 (1–3): 35–9. doi:10.1016/s0014-5793(02)03292-1. PMID 12297275. S2CID 39841617.
- ^ a b c Barth PG, Valianpour F, Bowen VM, Lam J, Duran M, Vaz FM, Wanders RJ (May 2004). "X-linked cardioskeletal myopathy and neutropenia (Barth syndrome): an update". American Journal of Medical Genetics. Part A. 126A (4): 349–54. doi:10.1002/ajmg.a.20660. PMID 15098233. S2CID 25566280.
- ^ Baile MG, Sathappa M, Lu YW, Pryce E, Whited K, McCaffery JM, et al. (January 2014). "Unremodeled and remodeled cardiolipin are functionally indistinguishable in yeast". The Journal of Biological Chemistry. 289 (3): 1768–78. doi:10.1074/jbc.M113.525733. PMC 3894353. PMID 24285538.
- ^ Schug ZT, Gottlieb E (October 2009). "Cardiolipin acts as a mitochondrial signalling platform to launch apoptosis". Biochimica et Biophysica Acta (BBA) - Biomembranes. 1788 (10): 2022–31. doi:10.1016/j.bbamem.2009.05.004. PMID 19450542.
- ^ a b c d Universal protein resource accession number Q16635 for "TAZ - Tafazzin - Homo sapiens (Human) - TAZ gene & protein" at UniProt. "UniProt: the universal protein knowledgebase". Nucleic Acids Research. 45 (D1): D158–D169. January 2017. doi:10.1093/nar/gkw1099. PMC 5210571. PMID 27899622.
- ^ Cantlay AM, Shokrollahi K, Allen JT, Lunt PW, Newbury-Ecob RA, Steward CG (September 1999). "Genetic analysis of the G4.5 gene in families with suspected Barth syndrome". The Journal of Pediatrics. 135 (3): 311–5. doi:10.1016/s0022-3476(99)70126-5. PMID 10484795.
- ^ a b "Barth Syndrome Foundation : Home". www.barthsyndrome.org. Retrieved 2019-08-04.
- ^ Cosson L, Toutain A, Simard G, Kulik W, Matyas G, Guichet A, et al. (May 2012). "Barth syndrome in a female patient". Molecular Genetics and Metabolism. 106 (1): 115–20. doi:10.1016/j.ymgme.2012.01.015. PMID 22410210.
- ^ Neuwald AF (August 1997). "Barth syndrome may be due to an acyltransferase deficiency". Current Biology. 7 (8): R465-6. Bibcode:1997CBio....7R.462N. doi:10.1016/S0960-9822(06)00237-5. PMID 9259571. S2CID 2763279.
- ^ Barth PG, Wanders RJ, Vreken P, Janssen EA, Lam J, Baas F (June 1999). "X-linked cardioskeletal myopathy and neutropenia (Barth syndrome) (MIM 302060)". Journal of Inherited Metabolic Disease. 22 (4): 555–67. doi:10.1023/A:1005568609936. PMID 10407787. S2CID 11545874.
- ^ Valianpour F, Mitsakos V, Schlemmer D, Towbin JA, Taylor JM, Ekert PG, et al. (June 2005). "Monolysocardiolipins accumulate in Barth syndrome but do not lead to enhanced apoptosis". Journal of Lipid Research. 46 (6): 1182–95. doi:10.1194/jlr.M500056-JLR200. PMID 15805542.
- ^ Barth PG, Scholte HR, Berden JA, Van der Klei-Van Moorsel JM, Luyt-Houwen IE, Van 't Veer-Korthof ET, et al. (December 1983). "An X-linked mitochondrial disease affecting cardiac muscle, skeletal muscle and neutrophil leucocytes". Journal of the Neurological Sciences. 62 (1–3): 327–55. doi:10.1016/0022-510x(83)90209-5. PMID 6142097. S2CID 22790290.
- ^ Aprikyan AA, Khuchua Z (May 2013). "Advances in the understanding of Barth syndrome". British Journal of Haematology. 161 (3): 330–8. doi:10.1111/bjh.12271. PMID 23432031. S2CID 2324502.
- ^ a b c d e Clarke SL, Bowron A, Gonzalez IL, Groves SJ, Newbury-Ecob R, Clayton N, et al. (February 2013). "Barth syndrome". Orphanet Journal of Rare Diseases. 8 (1): 23. doi:10.1186/1750-1172-8-23. PMC 3583704. PMID 23398819.
- ^ Ferri L, Dionisi-Vici C, Taurisano R, Vaz FM, Guerrini R, Morrone A (November 2016). "When silence is noise: infantile-onset Barth syndrome caused by a synonymous substitution affecting TAZ gene transcription". Clinical Genetics. 90 (5): 461–465. doi:10.1111/cge.12756. PMID 26853223. S2CID 3035706.
- ^ Kim GB, Kwon BS, Bae EJ, Noh CI, Seong MW, Park SS (May 2013). "A novel mutation of the TAZ gene in Barth syndrome: acute exacerbation after contrast-dye injection". Journal of Korean Medical Science. 28 (5): 784–7. doi:10.3346/jkms.2013.28.5.784. PMC 3653095. PMID 23678274.
- ^ Yen TY, Hwu WL, Chien YH, Wu MH, Lin MT, Tsao LY, et al. (August 2008). "Acute metabolic decompensation and sudden death in Barth syndrome: report of a family and a literature review". European Journal of Pediatrics. 167 (8): 941–4. doi:10.1007/s00431-007-0592-y. PMID 17846786. S2CID 23471712.
- ^ Clinical trial number NCT02976038 for "Open-Label Extension Trial to Characterize the Long-term Safety and Tolerability of Elamipretide in Subjects With Genetically Confirmed Primary Mitochondrial Myopathy (PMM)" at ClinicalTrials.gov
- ^ Szeto HH (April 2014). "First-in-class cardiolipin-protective compound as a therapeutic agent to restore mitochondrial bioenergetics". British Journal of Pharmacology. 171 (8): 2029–50. doi:10.1111/bph.12461. PMC 3976620. PMID 24117165.
- ^ Monteiro JP, Oliveira PJ, Jurado AS (October 2013). "Mitochondrial membrane lipid remodeling in pathophysiology: a new target for diet and therapeutic interventions". Progress in Lipid Research. 52 (4): 513–28. doi:10.1016/j.plipres.2013.06.002. hdl:10316/25581. PMID 23827885.
- ^ a b c Roberts AE, Nixon C, Steward CG, Gauvreau K, Maisenbacher M, Fletcher M, et al. (November 2012). "The Barth Syndrome Registry: distinguishing disease characteristics and growth data from a longitudinal study". American Journal of Medical Genetics. Part A. 158A (11): 2726–32. doi:10.1002/ajmg.a.35609. PMID 23045169. S2CID 29937658.
- ^ Ikon N, Ryan RO (February 2017). "Barth Syndrome: Connecting Cardiolipin to Cardiomyopathy". Lipids. 52 (2): 99–108. doi:10.1007/s11745-016-4229-7. PMC 5288132. PMID 28070695.
- ^ Wang G, McCain ML, Yang L, He A, Pasqualini FS, Agarwal A, et al. (June 2014). "Modeling the mitochondrial cardiomyopathy of Barth syndrome with induced pluripotent stem cell and heart-on-chip technologies". Nature Medicine. 20 (6): 616–23. doi:10.1038/nm.3545. PMC 4172922. PMID 24813252.
- ^ Woiewodski L, Ezon D, Cooper J, Feingold B (April 2017). "Barth Syndrome with Late-Onset Cardiomyopathy: A Missed Opportunity for Diagnosis". The Journal of Pediatrics. 183: 196–198. doi:10.1016/j.jpeds.2016.12.070. PMID 28108107.
- ^ Shemisa K, Li J, Tam M, Barcena J (September 2013). "Left ventricular noncompaction cardiomyopathy". Cardiovascular Diagnosis and Therapy. 3 (3): 170–5. doi:10.3978/j.issn.2223-3652.2013.05.04. PMC 3839206. PMID 24282766.
- ^ Bleyl SB, Mumford BR, Brown-Harrison MC, Pagotto LT, Carey JC, Pysher TJ, et al. (October 1997). "Xq28-linked noncompaction of the left ventricular myocardium: prenatal diagnosis and pathologic analysis of affected individuals". American Journal of Medical Genetics. 72 (3): 257–65. doi:10.1002/(SICI)1096-8628(19971031)72:3<257::AID-AJMG2>3.0.CO;2-O. PMID 9332651.
- ^ Spencer CT, Byrne BJ, Bryant RM, Margossian R, Maisenbacher M, Breitenger P, et al. (November 2011). "Impaired cardiac reserve and severely diminished skeletal muscle O₂ utilization mediate exercise intolerance in Barth syndrome". American Journal of Physiology. Heart and Circulatory Physiology. 301 (5): H2122-9. doi:10.1152/ajpheart.00479.2010. PMID 21873497.
- ^ a b Adès LC, Gedeon AK, Wilson MJ, Latham M, Partington MW, Mulley JC, et al. (February 1993). "Barth syndrome: clinical features and confirmation of gene localisation to distal Xq28". American Journal of Medical Genetics. 45 (3): 327–34. doi:10.1002/ajmg.1320450309. PMID 8434619.
- ^ a b Ferreira C, Thompson R, Vernon H (1993). Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJ, Stephens K, Amemiya A (eds.). Barth Syndrome. University of Washington, Seattle. PMID 25299040.
{{cite book}}:|work=ignored (help) - ^ Rigaud C, Lebre AS, Touraine R, Beaupain B, Ottolenghi C, Chabli A, et al. (May 2013). "Natural history of Barth syndrome: a national cohort study of 22 patients". Orphanet Journal of Rare Diseases. 8: 70. doi:10.1186/1750-1172-8-70. PMC 3656783. PMID 23656970.
- ^ a b Vernon HJ, Sandlers Y, McClellan R, Kelley RI (June 2014). "Clinical laboratory studies in Barth Syndrome". Molecular Genetics and Metabolism. 112 (2): 143–7. doi:10.1016/j.ymgme.2014.03.007. PMID 24751896.
- ^ Mazzocco MM, Henry AE, Kelly RI (February 2007). "Barth syndrome is associated with a cognitive phenotype". Journal of Developmental and Behavioral Pediatrics. 28 (1): 22–30. doi:10.1097/01.DBP.0000257519.79803.90. PMC 2813702. PMID 17353728.
- ^ a b Cole LK, Kim JH, Amoscato AA, Tyurina YY, Bay RH, Karimi B, et al. (October 2018). "Aberrant cardiolipin metabolism is associated with cognitive deficiency and hippocampal alteration in tafazzin knockdown mice". Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease. 1864 (10): 3353–3367. doi:10.1016/j.bbadis.2018.07.022. PMC 6532065. PMID 30055293.
- ^ Corazzi L, Robert R (2009). "Lipids of Brain Mitochondria". In Lajtha A, Tettamanti G, Goracci G (eds.). Handbook of Neurochemistry and Molecular Neurobiology. Springer US. pp. 199–221. doi:10.1007/978-0-387-30378-9_8. ISBN 9780387303451.
- ^ Starkov AA, Andreyev AY, Zhang SF, Starkova NN, Korneeva M, Syromyatnikov M, Popov VN (December 2014). "Scavenging of H2O2 by mouse brain mitochondria". Journal of Bioenergetics and Biomembranes. 46 (6): 471–7. doi:10.1007/s10863-014-9581-9. PMC 4634880. PMID 25248416.
- ^ a b Wortmann SB, Kluijtmans LA, Engelke UF, Wevers RA, Morava E (January 2012). "The 3-methylglutaconic acidurias: what's new?". Journal of Inherited Metabolic Disease. 35 (1): 13–22. doi:10.1007/s10545-010-9210-7. PMC 3249181. PMID 20882351.
- ^ Schmidt MR, Birkebaek N, Gonzalez I, Sunde L (March 2004). "Barth syndrome without 3-methylglutaconic aciduria". Acta Paediatrica. 93 (3): 419–21. doi:10.1111/j.1651-2227.2004.tb02974.x. PMID 15124852. S2CID 33167027.
- ^ Steward CG, Groves SJ, Taylor CT, Maisenbacher MK, Versluys B, Newbury-Ecob RA, et al. (January 2019). "Neutropenia in Barth syndrome: characteristics, risks, and management". Current Opinion in Hematology. 26 (1): 6–15. doi:10.1097/MOH.0000000000000472. PMC 6392059. PMID 30451719.
- ^ Dale DC, Bolyard AA, Schwinzer BG, Pracht G, Bonilla MA, Boxer L, et al. (July 2006). "The Severe Chronic Neutropenia International Registry: 10-Year Follow-up Report". Supportive Cancer Therapy. 3 (4): 220–31. doi:10.3816/SCT.2006.n.020. PMID 18632498.
- ^ a b c Pathak S, Meng WJ, Zhang H, Gnosa S, Nandy SK, Adell G, et al. (2014). "Tafazzin protein expression is associated with tumorigenesis and radiation response in rectal cancer: a study of Swedish clinical trial on preoperative radiotherapy". PLOS ONE. 9 (5): e98317. Bibcode:2014PLoSO...998317P. doi:10.1371/journal.pone.0098317. PMC 4032294. PMID 24858921.
- ^ a b Sapandowski A, Stope M, Evert K, Evert M, Zimmermann U, Peter D, et al. (December 2015). "Cardiolipin composition correlates with prostate cancer cell proliferation". Molecular and Cellular Biochemistry. 410 (1–2): 175–85. doi:10.1007/s11010-015-2549-1. PMID 26314254. S2CID 10664158.
- ^ a b Chevillard S, Ugolin N, Vielh P, Ory K, Levalois C, Elliott D, et al. (October 2004). "Gene expression profiling of differentiated thyroid neoplasms: diagnostic and clinical implications". Clinical Cancer Research. 10 (19): 6586–97. doi:10.1158/1078-0432.CCR-04-0053. PMID 15475448.
- ^ Mick DU, Dennerlein S, Wiese H, Reinhold R, Pacheu-Grau D, Lorenzi I, et al. (December 2012). "MITRAC links mitochondrial protein translocation to respiratory-chain assembly and translational regulation". Cell. 151 (7): 1528–41. doi:10.1016/j.cell.2012.11.053. hdl:11858/00-001M-0000-000E-DDDF-4. PMID 23260140.
- ^ Schlame, Michael; Xu, Yang (2020-08-21). "The Function of Tafazzin, a Mitochondrial Phospholipid–Lysophospholipid Acyltransferase". Journal of Molecular Biology. Molecular Mechanisms in Integral Membrane Enzymology. 432 (18): 5043–5051. doi:10.1016/j.jmb.2020.03.026. ISSN 0022-2836. PMC 7483898. PMID 32234310.
Further reading
[edit]- "Mouse model of Barth syndrome". SciBX. 3 (47): 1427. 9 December 2010. doi:10.1038/scibx.2010.1427.
- Soustek MS, Falk DJ, Mah CS, Toth MJ, Schlame M, Lewin AS, Byrne BJ (July 2011). "Characterization of a transgenic short hairpin RNA-induced murine model of Tafazzin deficiency". Human Gene Therapy. 22 (7): 865–71. doi:10.1089/hum.2010.199. PMC 3166794. PMID 21091282.
- Takeda A, Sudo A, Yamada M, Yamazawa H, Izumi G, Nishino I, Ariga T (November 2011). "Barth syndrome diagnosed in the subclinical stage of heart failure based on the presence of lipid storage myopathy and isolated noncompaction of the ventricular myocardium". European Journal of Pediatrics. 170 (11): 1481–4. doi:10.1007/s00431-011-1576-5. PMID 21932011. S2CID 23956305.
- Bachou T, Giannakopoulos A, Trapali C, Vazeou A, Kattamis A (2009). "A novel mutation in the G4.5 (TAZ) gene in a Greek patient with Barth syndrome". Blood Cells, Molecules & Diseases. 42 (3): 262–4. doi:10.1016/j.bcmd.2008.11.004. PMID 19261493.
- Gonzalez IL (May 2005). "Barth syndrome: TAZ gene mutations, mRNAs, and evolution". American Journal of Medical Genetics Part A. 134 (4): 409–14. doi:10.1002/ajmg.a.30661. PMID 15793838. S2CID 119636.
- Stelzl U, Worm U, Lalowski M, Haenig C, Brembeck FH, Goehler H, Stroedicke M, Zenkner M, Schoenherr A, Koeppen S, Timm J, Mintzlaff S, Abraham C, Bock N, Kietzmann S, Goedde A, Toksöz E, Droege A, Krobitsch S, Korn B, Birchmeier W, Lehrach H, Wanker EE (September 2005). "A human protein-protein interaction network: a resource for annotating the proteome". Cell. 122 (6): 957–68. doi:10.1016/j.cell.2005.08.029. hdl:11858/00-001M-0000-0010-8592-0. PMID 16169070. S2CID 8235923.
- Zimmerman RS, Cox S, Lakdawala NK, Cirino A, Mancini-DiNardo D, Clark E, Leon A, Duffy E, White E, Baxter S, Alaamery M, Farwell L, Weiss S, Seidman CE, Seidman JG, Ho CY, Rehm HL, Funke BH (May 2010). "A novel custom resequencing array for dilated cardiomyopathy". Genetics in Medicine. 12 (5): 268–78. doi:10.1097/GIM.0b013e3181d6f7c0. PMC 3018746. PMID 20474083.
- Malhotra A, Edelman-Novemsky I, Xu Y, Plesken H, Ma J, Schlame M, Ren M (February 2009). "Role of calcium-independent phospholipase A2 in the pathogenesis of Barth syndrome". Proceedings of the National Academy of Sciences of the United States of America. 106 (7): 2337–41. Bibcode:2009PNAS..106.2337M. doi:10.1073/pnas.0811224106. PMC 2650157. PMID 19164547.
- van Werkhoven MA, Thorburn DR, Gedeon AK, Pitt JJ (October 2006). "Monolysocardiolipin in cultured fibroblasts is a sensitive and specific marker for Barth Syndrome". Journal of Lipid Research. 47 (10): 2346–51. doi:10.1194/jlr.D600024-JLR200. PMID 16873891.
- Acehan D, Xu Y, Stokes DL, Schlame M (January 2007). "Comparison of lymphoblast mitochondria from normal subjects and patients with Barth syndrome using electron microscopic tomography". Laboratory Investigation; A Journal of Technical Methods and Pathology. 87 (1): 40–8. doi:10.1038/labinvest.3700480. PMC 2215767. PMID 17043667.
- Claypool SM, Boontheung P, McCaffery JM, Loo JA, Koehler CM (December 2008). "The cardiolipin transacylase, tafazzin, associates with two distinct respiratory components providing insight into Barth syndrome". Molecular Biology of the Cell. 19 (12): 5143–55. doi:10.1091/mbc.E08-09-0896. PMC 2592642. PMID 18799610.
- Mehrle A, Rosenfelder H, Schupp I, del Val C, Arlt D, Hahne F, Bechtel S, Simpson J, Hofmann O, Hide W, Glatting KH, Huber W, Pepperkok R, Poustka A, Wiemann S (January 2006). "The LIFEdb database in 2006". Nucleic Acids Research. 34 (Database issue): D415–8. doi:10.1093/nar/gkj139. PMC 1347501. PMID 16381901.
- McKenzie M, Lazarou M, Thorburn DR, Ryan MT (August 2006). "Mitochondrial respiratory chain supercomplexes are destabilized in Barth Syndrome patients". Journal of Molecular Biology. 361 (3): 462–9. CiteSeerX 10.1.1.314.3366. doi:10.1016/j.jmb.2006.06.057. PMID 16857210.
- Lu B, Kelher MR, Lee DP, Lewin TM, Coleman RA, Choy PC, Hatch GM (October 2004). "Complex expression pattern of the Barth syndrome gene product tafazzin in human cell lines and murine tissues". Biochemistry and Cell Biology. 82 (5): 569–76. doi:10.1139/o04-055. PMID 15499385.
- Ma L, Vaz FM, Gu Z, Wanders RJ, Greenberg ML (October 2004). "The human TAZ gene complements mitochondrial dysfunction in the yeast taz1Delta mutant. Implications for Barth syndrome". The Journal of Biological Chemistry. 279 (43): 44394–9. doi:10.1074/jbc.M405479200. PMID 15304507.
- Wiemann S, Arlt D, Huber W, Wellenreuther R, Schleeger S, Mehrle A, Bechtel S, Sauermann M, Korf U, Pepperkok R, Sültmann H, Poustka A (October 2004). "From ORFeome to biology: a functional genomics pipeline". Genome Research. 14 (10B): 2136–44. doi:10.1101/gr.2576704. PMC 528930. PMID 15489336.
- Saunders MA, Slatkin M, Garner C, Hammer MF, Nachman MW (November 2005). "The extent of linkage disequilibrium caused by selection on G6PD in humans". Genetics. 171 (3): 1219–29. doi:10.1534/genetics.105.048140. PMC 1456824. PMID 16020776.
- Vaz FM, Houtkooper RH, Valianpour F, Barth PG, Wanders RJ (October 2003). "Only one splice variant of the human TAZ gene encodes a functional protein with a role in cardiolipin metabolism". The Journal of Biological Chemistry. 278 (44): 43089–94. doi:10.1074/jbc.M305956200. PMID 12930833.
External links
[edit]- GeneReviews/NCBI/NIH/UW entry on Dilated Cardiomyopathy Overview
- TAZ+protein,+human at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
This article incorporates text from the United States National Library of Medicine, which is in the public domain.