Erythropoietin
| erythropoietin | |||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
 | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Identifiers | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Aliases | EPOuniprot:P01588epoetin | ||||||||||||||||||||||||||||||||||||||||||||||||||
| External IDs | GeneCards: [1]; OMA:- orthologs | ||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Wikidata | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
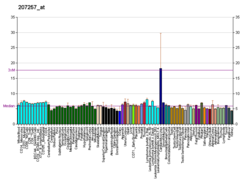
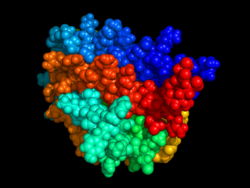
Erythropoietin (/ɪˌrɪθroʊˈpɔɪ.ɪtɪn, -rə-, -pɔɪˈɛtɪn, -ˈiːtɪn/;[1][2][3] EPO), also known as erythropoetin, haematopoietin, or haemopoietin, is a glycoprotein cytokine secreted mainly by the kidneys in response to cellular hypoxia; it stimulates red blood cell production (erythropoiesis) in the bone marrow. Low levels of EPO (around 10 mU/mL) are constantly secreted in sufficient quantities to compensate for normal red blood cell turnover. Common causes of cellular hypoxia resulting in elevated levels of EPO (up to 10 000 mU/mL) include any anemia, and hypoxemia due to chronic lung disease and mouth disease.
Erythropoietin is produced by interstitial fibroblasts in the kidney in close association with the peritubular capillary and proximal convoluted tubule. It is also produced in perisinusoidal cells in the liver. Liver production predominates in the fetal and perinatal period; renal production predominates in adulthood. It is homologous with thrombopoietin.
Exogenous erythropoietin, recombinant human erythropoietin (rhEPO), is produced by recombinant DNA technology in cell culture and are collectively called erythropoiesis-stimulating agents (ESA): two examples are epoetin alfa and epoetin beta. ESAs are used in the treatment of anemia in chronic kidney disease, anemia in myelodysplasia, and in anemia from cancer chemotherapy. Risks of therapy include death, myocardial infarction, stroke, venous thromboembolism, and tumor recurrence. Risk increases when EPO treatment raises hemoglobin levels over 11 g/dL to 12 g/dL: this is to be avoided.
rhEPO has been used illicitly as a performance-enhancing drug.[4] It can often be detected in blood, due to slight differences from the endogenous protein; for example, in features of posttranslational modification.
Pharmacology
[edit]EPO is highly glycosylated (40% of total molecular weight), with half-life in blood around 5 h. EPO's half-life may vary between endogenous and various recombinant versions. Additional glycosylation or other alterations of EPO via recombinant technology have led to the increase of EPO's stability in blood (thus requiring less frequent injections).
Function
[edit]Red blood cell production
[edit]Erythropoietin is an essential hormone for red blood cell production. Without it, definitive erythropoiesis does not take place. Under hypoxic conditions, the kidney will produce and secrete erythropoietin to increase the production of red blood cells by targeting CFU-E, proerythroblast and basophilic erythroblast subsets in the differentiation. Erythropoietin has its primary effect on red blood cell progenitors and precursors (which are found in the bone marrow in humans) by promoting their survival through protecting these cells from apoptosis, or cell death.
Erythropoietin is the primary erythropoietic factor that cooperates with various other growth factors (e.g., IL-3, IL-6, glucocorticoids, and SCF) involved in the development of erythroid lineage from multipotent progenitors. The burst-forming unit-erythroid (BFU-E) cells start erythropoietin receptor expression and are sensitive to erythropoietin. Subsequent stage, the colony-forming unit-erythroid (CFU-E), expresses maximal erythropoietin receptor density and is completely dependent on erythropoietin for further differentiation. Precursors of red cells, the proerythroblasts and basophilic erythroblasts also express erythropoietin receptor and are therefore affected by it.
Nonhematopoietic roles
[edit]Erythropoietin was reported to have a range of actions beyond stimulation of erythropoiesis including vasoconstriction-dependent hypertension, stimulating angiogenesis, and promoting cell survival via activation of EPO receptors resulting in anti-apoptotic effects on ischemic tissues. However this proposal is controversial with numerous studies showing no effect.[5] It is also inconsistent with the low levels of EPO receptors on those cells. Clinical trials in humans with ischemic heart, neural and renal tissues have not demonstrated the same benefits seen in animals. In addition some research studies have shown its neuroprotective effect on diabetic neuropathy, however these data were not confirmed in clinical trials that have been conducted on the deep peroneal, superficial peroneal, tibial and sural nerves.[6]
Mechanism of action
[edit]Erythropoietin has been shown to exert its effects by binding to the erythropoietin receptor (EpoR).[7][8] EPO binds to the erythropoietin receptor on the red cell progenitor surface and activates a JAK2 signalling cascade. This initiates the STAT5, PIK3 and Ras MAPK pathways. This results in differentiation, survival and proliferation of the erythroid cell.[9] SOCS1, SOCS3 and CIS are also expressed which act as negative regulators of the cytokine signal.[10]
High level erythropoietin receptor expression is localized to erythroid progenitor cells. While there are reports that EPO receptors are found in a number of other tissues, such as heart, muscle, kidney and peripheral/central nervous tissue, those results are confounded by nonspecificity of reagents such as anti-EpoR antibodies.[11] In controlled experiments, a functional EPO receptor is not detected in those tissues.[12] In the bloodstream, red cells themselves do not express erythropoietin receptor, so cannot respond to EPO. However, indirect dependence of red cell longevity in the blood on plasma erythropoietin levels has been reported, a process termed neocytolysis.[13] In addition, there is conclusive evidence that EPO receptor expression is upregulated in brain injury.[14]
Synthesis and regulation
[edit]Erythropoietin levels in blood are quite low in the absence of anemia, at around 10 mU/mL. However, in hypoxic stress, EPO production may increase up to 1000-fold, reaching 10 000 mU/mL of blood. In adults, EPO is synthesized mainly by interstitial cells in the peritubular capillary bed of the renal cortex, with additional amounts being produced in the liver,[15][16][17] and the pericytes in the brain.[18] Regulation is believed to rely on a feedback mechanism measuring blood oxygenation and iron availability.[19] Constitutively synthesized transcription factors for EPO, known as hypoxia-inducible factors, are hydroxylated and proteosomally digested in the presence of oxygen and iron. During normoxia GATA2 inhibits the promoter region for EPO. GATA2 levels decrease during hypoxia and allow the promotion of EPO production.[20]
Erythropoietin production can be induced by HIF-2α as well as by PGC-1α.[21] Erythropoietin also activates these factors, resulting in a positive feedback loop.[21]
Medical use
[edit]
Erythropoietins available for use as therapeutic agents are produced by recombinant DNA technology in cell culture, and include Epogen/Procrit (epoetin alfa) and Aranesp (darbepoetin alfa); they are used in treating anemia resulting from chronic kidney disease,[22] chemotherapy induced anemia in patients with cancer, inflammatory bowel disease (Crohn's disease and ulcerative colitis)[23] and myelodysplasia from the treatment of cancer (chemotherapy and radiation). The package inserts include boxed warnings of increased risk of death, myocardial infarction, stroke, venous thromboembolism, and tumor recurrence, particularly when used to increase the hemoglobin levels to more than 11 g/dL to 12 g/dL.[24]
History
[edit]In 1905, Paul Carnot proposed the idea that a hormone regulates the production of red blood cells. After conducting experiments on rabbits subject to bloodletting, Carnot and his graduate student Clotilde-Camille Deflandre[25] attributed an increase in red blood cells in rabbit subjects to a hemotropic factor called hemopoietin. Eva Bonsdorff and Eeva Jalavisto called the hemopoietic substance 'erythropoietin'. K.R. Reissman and Allan J. Erslev demonstrated that a certain substance, circulated in the blood, is able to stimulate red blood cell production and increase hematocrit. This substance was purified and confirmed as erythropoietin.[19][26]
In 1977, Goldwasser and Kung purified EPO.[27] Pure EPO allowed the amino acid sequence to be partially identified and the gene to be isolated.[19] Synthetic EPO was first successfully used to correct anemia in 1987.[28] In 1985, Lin et al isolated the human erythropoietin gene from a genomic phage library and used it to produce EPO.[29] In 1989, the US Food and Drug Administration (FDA) approved the hormone Epogen for use in certain anemias.[30][31]
Gregg L. Semenza and Peter J. Ratcliffe studied the EPO gene and its oxygen-dependent regulation. Along with William Kaelin Jr., they were awarded the 2019 Nobel Prize in Physiology or Medicine for their discovery of hypoxia-inducible factor (HIF), which regulates the EPO gene, as well as other genes, in response to hypoxia.[32]
Biosimilars
[edit]In December 2007, Retacrit and Silapo (both epoetin zeta) were approved for use in the European Union.[33][34]
Usage as doping product
[edit]As a performance-enhancing drug, EPO has been banned since the early 1990s, but a first test was not available until the 2000 Summer Olympics.[35] Before this test was available, some athletes were sanctioned after confessing to having used EPO, for example in the Festina affair, when a car with doping products for the Festina cycling team was found.
The first doping test in cycling was used in the 2001 La Flèche Wallonne. The first rider to test positive in that race was Bo Hamburger, although he was later acquitted because his B-sample was not conclusive.[36]
The U.S. Postal Service Pro Cycling Team, under the leadership of Lance Armstrong and Johan Bruyneel, ran a sophisticated doping program that lasted for many years during the late 1990s and early 2000s. Erythropoietin was a common substance used by the cyclists.[37]
A 2007 study showed that EPO has a significant effect on exercise performance.[clarify][38] A 2017 study showed at submaximal exertion the effects of EPO were not distinguishable from a placebo. Stating "[At] Submaximal [exertion]...[mean power] did not differ between groups." Nevertheless, at "maximal [exertion power output was] higher in the rHuEPO group compared with the placebo group." So, even though there was no difference at lower levels of exertion at maximal exertion the EPO group still performed better than the placebo group.[39]
In March 2019, American mixed martial artist and former UFC Bantamweight Champion T.J. Dillashaw tested positive for EPO in a drug test administered by USADA, and was stripped of the UFC bantamweight title and suspended for 2 years.[40] In September 2023 two-time tennis major champion Simona Halep received a 4-year suspension by the International Tennis Integrity Agency for two separate violations, one concerning the level of EPO in a blood sample collected in August 2022; Halep maintained her innocence, and indicated she would appeal the ban. Halep was later cleared to return following a successful appeal, due to findings that a contaminated supplement most likely contributed to the positive tests.[41][42]
References
[edit]- ^ "Erythropoietin". Merriam-Webster.com Dictionary. Merriam-Webster.
- ^ "Erythropoietin". Dictionary.com Unabridged (Online). n.d.
- ^ "erythropoietin – definition of erythropoietin in English from the Oxford dictionary". OxfordDictionaries.com. Archived from the original on 27 September 2012. Retrieved 20 January 2016.
- ^ Momaya A, Fawal M, Estes R (April 2015). "Performance-enhancing substances in sports: a review of the literature". Sports Medicine. 45 (4): 517–31. doi:10.1007/s40279-015-0308-9. PMID 25663250. S2CID 45124293.
- ^ Elliott S, Sinclair AM (2012). "The effect of erythropoietin on normal and neoplastic cells". Biologics: Targets and Therapy. 6: 163–89. doi:10.2147/BTT.S32281. PMC 3402043. PMID 22848149.
- ^ Hosseini-Zare MS, Dashti-Khavidaki S, Mahdavi-Mazdeh M, Ahmadi F, Akrami S (July 2012). "Peripheral neuropathy response to erythropoietin in type 2 diabetic patients with mild to moderate renal failure". Clinical Neurology and Neurosurgery. 114 (6): 663–7. doi:10.1016/j.clineuro.2012.01.007. PMID 22296650. S2CID 19516031.
- ^ Middleton SA, Barbone FP, Johnson DL, Thurmond RL, You Y, McMahon FJ, Jin R, Livnah O, Tullai J, Farrell FX, Goldsmith MA, Wilson IA, Jolliffe LK (May 1999). "Shared and unique determinants of the erythropoietin (EPO) receptor are important for binding EPO and EPO mimetic peptide". The Journal of Biological Chemistry. 274 (20): 14163–9. doi:10.1074/jbc.274.20.14163. PMID 10318834.
- ^ Livnah O, Johnson DL, Stura EA, Farrell FX, Barbone FP, You Y, Liu KD, Goldsmith MA, He W, Krause CD, Pestka S, Jolliffe LK, Wilson IA (November 1998). "An antagonist peptide-EPO receptor complex suggests that receptor dimerization is not sufficient for activation". Nature Structural Biology. 5 (11): 993–1004. doi:10.1038/2965. PMID 9808045. S2CID 24052881.
- ^ Kasper, C. (2003). "Erythropoietin". The Cytokine Handbook. pp. 149–166. doi:10.1016/B978-012689663-3/50011-9. ISBN 978-0-12-689663-3.
- ^ Hodges VM, Rainey S, Lappin TR, Maxwell AP (November 2007). "Pathophysiology of anemia and erythrocytosis". Critical Reviews in Oncology/Hematology. 64 (2): 139–58. doi:10.1016/j.critrevonc.2007.06.006. PMID 17656101.
- ^ Elliott S, Busse L, Bass MB, Lu H, Sarosi I, Sinclair AM, et al. (March 2006). "Anti-Epo receptor antibodies do not predict Epo receptor expression". Blood. 107 (5): 1892–5. doi:10.1182/blood-2005-10-4066. PMID 16249375.
- ^ Sinclair AM, Coxon A, McCaffery I, Kaufman S, Paweletz K, Liu L, et al. (May 2010). "Functional erythropoietin receptor is undetectable in endothelial, cardiac, neuronal, and renal cells". Blood. 115 (21): 4264–72. doi:10.1182/blood-2009-10-248666. PMID 20124513.
- ^ Risso A, Ciana A, Achilli C, Antonutto G, Minetti G (2014). "Neocytolysis: none, one or many? A reappraisal and future perspectives". Frontiers in Physiology. 5: 54. doi:10.3389/fphys.2014.00054. PMC 3924315. PMID 24592241.
- ^ Ott C, Martens H, Hassouna I, Oliveira B, Erck C, Zafeiriou MP, et al. (December 2015). "Widespread Expression of Erythropoietin Receptor in Brain and Its Induction by Injury". Molecular Medicine. 21 (1): 803–815. doi:10.2119/molmed.2015.00192. PMC 4818269. PMID 26349059.
- ^ Jacobson LO, Goldwasser E, Fried W, Plzak L (March 1957). "Role of the kidney in erythropoiesis". Nature. 179 (4560): 633–4. Bibcode:1957Natur.179..633J. doi:10.1038/179633a0. PMID 13418752. S2CID 4162940.
- ^ Fisher JW, Koury S, Ducey T, Mendel S (October 1996). "Erythropoietin production by interstitial cells of hypoxic monkey kidneys". British Journal of Haematology. 95 (1): 27–32. doi:10.1046/j.1365-2141.1996.d01-1864.x. PMID 8857934. S2CID 38309595.
- ^ Barrett KE, Barman SM, Boitano S, Brooks H (eds.). Ganong's review of Medical Physiology (24th ed.). McGraw Hill. p. 709. ISBN 978-1-25-902753-6.
- ^ Ji P (November 2016). "Pericytes: new EPO-producing cells in the brain". Blood. 128 (21): 2483–2485. doi:10.1182/blood-2016-10-743880. PMID 27884833.
- ^ a b c Jelkmann W (March 2007). "Erythropoietin after a century of research: younger than ever". European Journal of Haematology. 78 (3): 183–205. doi:10.1111/j.1600-0609.2007.00818.x. PMID 17253966. S2CID 37331032.
- ^ Jelkmann W (March 2011). "Regulation of erythropoietin production". The Journal of Physiology. 589 (Pt 6): 1251–8. doi:10.1113/jphysiol.2010.195057. PMC 3082088. PMID 21078592.
- ^ a b Packer M (2020). "Sodium-Glucose Cotransporter-2 Inhibitor (SGLT2i) as a Primary Preventative Agent in the Healthy Individual: A Need of a Future Randomised Clinical Trial?". Circulation: Heart Failure. 13 (9): e007197. doi:10.1161/CIRCHEARTFAILURE.120.007197. PMID 32894987. S2CID 221540765.
- ^ "The Story of Erythropoietin". www.hematology.org. 16 February 2018. Archived from the original on 18 February 2019. Retrieved 18 February 2019.
- ^ Liu S, Ren J, Hong Z, Yan D, Gu G, Han G, Wang G, Ren H, Chen J, Li J (February 2013). "Efficacy of erythropoietin combined with enteral nutrition for the treatment of anemia in Crohn's disease: a prospective cohort study". Nutrition in Clinical Practice. 28 (1): 120–7. doi:10.1177/0884533612462744. PMID 23064018.
- ^ "Safety Labeling Changes: Epogen/Procrit (epoetin alfa) and Aranesp (darbepoetin alfa)". MedWatch: The FDA Safety Information and Adverse Event Reporting Program. United States Food and Drug Administration. 11 August 2011. Archived from the original on 12 January 2017. Retrieved 16 December 2019.
- ^ Carnot P, Deflandre C (1906). "Sur l'activite hematopoietique du serum au cours de la regeneration du sang". Compt. Rend. Acad. Sci. 143: 384–386.
- ^ Höke A (2005). Erythropoietin and the Nervous System. Berlin: Springer. ISBN 978-0-387-30010-8. OCLC 64571745.[page needed]
- ^ Miyake T, Kung CK, Goldwasser E (August 1977). "Purification of human erythropoietin". The Journal of Biological Chemistry. 252 (15): 5558–64. doi:10.1016/S0021-9258(19)63387-9. PMID 18467.
- ^ Eschbach JW, Egrie JC, Downing MR, Browne JK, Adamson JW (January 1987). "Correction of the anemia of end-stage renal disease with recombinant human erythropoietin. Results of a combined phase I and II clinical trial". The New England Journal of Medicine. 316 (2): 73–8. doi:10.1056/NEJM198701083160203. PMID 3537801.
- ^ Lin FK, Suggs S, Lin CH, Browne JK, Smalling R, Egrie JC, Chen KK, Fox GM, Martin F, Stabinsky Z (November 1985). "Cloning and expression of the human erythropoietin gene". Proceedings of the National Academy of Sciences of the United States of America. 82 (22): 7580–4. Bibcode:1985PNAS...82.7580L. doi:10.1073/pnas.82.22.7580. PMC 391376. PMID 3865178.
- ^ "Epogen- epoetin alfa solution". DailyMed. 25 July 2018. Retrieved 20 April 2022.
- ^ "Epogen: FDA-Approved Drugs". U.S. Food and Drug Administration (FDA). 13 January 2017. Retrieved 20 April 2022.
- ^ "The Nobel Prize in Physiology or Medicine 2019". NobelPrize.org. 7 October 2019. Archived from the original on 31 October 2021. Retrieved 30 October 2019.
- ^ "Retacrit EPAR". European Medicines Agency (EMA). 17 September 2018. Archived from the original on 30 December 2019. Retrieved 2 April 2020.
- ^ "Silapo EPAR". European Medicines Agency (EMA). 17 September 2018. Archived from the original on 22 October 2020. Retrieved 2 April 2020.
- ^ "EPO DETECTION". World Anti-Doping Agency. December 2014. Archived from the original on 7 September 2017. Retrieved 17 December 2017.
- ^ "Hamburger cleared of EPO use". BBC. 10 August 2001. Archived from the original on 16 April 2016. Retrieved 17 December 2017.
- ^ Perishable (10 October 2012). "Statement From USADA CEO Travis T. Tygart Regarding The U.S. Postal Service Pro Cycling Team Doping Conspiracy | U.S. Anti-Doping Agency (USADA)". www.usada.org. Archived from the original on 26 August 2021. Retrieved 26 August 2021.
- ^ Thomsen JJ, Rentsch RL, Robach P, Calbet JA, Boushel R, Rasmussen P, Juel C, Lundby C (November 2007). "Prolonged administration of recombinant human erythropoietin increases submaximal performance more than maximal aerobic capacity". European Journal of Applied Physiology. 101 (4): 481–6. doi:10.1007/s00421-007-0522-8. PMID 17668232. S2CID 6492432.
- ^ Heuberger JA, Rotmans JI, Gal P, Stuurman FE, van 't Westende J, Post TE, Daniels JM, Moerland M, van Veldhoven PL, de Kam ML, Ram H, de Hon O, Posthuma JJ, Burggraaf J, Cohen AF (August 2017). "Effects of erythropoietin on cycling performance of well trained cyclists: a double-blind, randomised, placebo-controlled trial". The Lancet. Haematology. 4 (8): e374–e386. doi:10.1016/S2352-3026(17)30105-9. PMID 28669689.
- ^ "USADA suspends Dillashaw 2 years for EPO use". ESPN.com. 9 April 2019. Archived from the original on 10 April 2019. Retrieved 9 April 2019.
- ^ Tetrault-Ferber, Gabrielle (5 March 2024). "CAS clears Halep for immediate return after doping ban cut". Reuters.
- ^ "Simona Halep: Will appeal 4-year ban over doping violations", ESPN, September 12, 2023
Further reading
[edit]- Liu C, Huang C, Xie J, Li H, Hong M, Chen X, Wang J, Wang J, Li Z, Wang J, Wang W (October 2020). "Potential Efficacy of Erythropoietin on Reducing the Risk of Mortality in Patients with Traumatic Brain Injury: A Systematic Review and Meta-Analysis". Biomed Res Int. 2020: 7563868. doi:10.1155/2020/7563868. PMC 7644316. PMID 33178833.
- Takeuchi M, Kobata A (September 1991). "Structures and functional roles of the sugar chains of human erythropoietins". Glycobiology. 1 (4): 337–46. doi:10.1093/glycob/1.4.337. PMID 1820196.
- Semba RD, Juul SE (August 2002). "Erythropoietin in human milk: physiology and role in infant health". Journal of Human Lactation. 18 (3): 252–61. doi:10.1177/089033440201800307. PMID 12192960. S2CID 13546958.
- Ratcliffe PJ (2002). "From erythropoietin to oxygen: hypoxia-inducible factor hydroxylases and the hypoxia signal pathway". Blood Purification. 20 (5): 445–50. doi:10.1159/000065201. PMID 12207089. S2CID 46866485.
- Westenfelder C (2002). "Unexpected renal actions of erythropoietin". Experimental Nephrology. 10 (5–6): 294–8. doi:10.1159/000065304 (inactive 1 November 2024). PMID 12381912. S2CID 33343853.
{{cite journal}}: CS1 maint: DOI inactive as of November 2024 (link) - Becerra SP, Amaral J (December 2002). "Erythropoietin--an endogenous retinal survival factor". The New England Journal of Medicine. 347 (24): 1968–70. doi:10.1056/NEJMcibr022629. PMID 12477950.
- Genc S, Koroglu TF, Genc K (March 2004). "Erythropoietin and the nervous system". Brain Research. 1000 (1–2): 19–31. doi:10.1016/j.brainres.2003.12.037. PMID 15053948. S2CID 46246546.
- Fandrey J (June 2004). "Oxygen-dependent and tissue-specific regulation of erythropoietin gene expression". American Journal of Physiology. Regulatory, Integrative and Comparative Physiology. 286 (6): R977–88. doi:10.1152/ajpregu.00577.2003. PMID 15142852. S2CID 697196.
- Juul S (March 2004). "Recombinant erythropoietin as a neuroprotective treatment: in vitro and in vivo models". Clinics in Perinatology. 31 (1): 129–42. doi:10.1016/j.clp.2004.03.004. PMID 15183662.
- Buemi M, Caccamo C, Nostro L, Cavallaro E, Floccari F, Grasso G (March 2005). "Brain and cancer: the protective role of erythropoietin". Medicinal Research Reviews. 25 (2): 245–59. doi:10.1002/med.20012. PMID 15389732. S2CID 46380760.
- Sytkowski AJ (July 2007). "Does erythropoietin have a dark side? Epo signaling and cancer cells". Science's STKE. 2007 (395): pe38. doi:10.1126/stke.3952007pe38. PMID 17636183. S2CID 43566459.
External links
[edit]- "Erythropoietin". Drug Information Portal. U.S. National Library of Medicine.
- Overview of all the structural information available in the PDB for UniProt: P01588 (Erythropoietin) at the PDBe-KB.