Parkinson's disease
Parkinson's disease (PD), or simply Parkinson's, is a neurodegenerative disease of mainly the central nervous system that affects both the motor and non-motor systems of the body. The symptoms usually emerge slowly, and, as the disease progresses, non-motor symptoms become more common. Usually symptoms include tremors, slowness of movement, rigidity, and difficulty with balance, collectively known as parkinsonism. Parkinson's disease dementia, falls and neuropsychiatric problems such as sleep abnormalities, psychosis, mood swings, or behavioral changes may also arise in advanced stages.
Most cases of Parkinson's disease are sporadic, but a few contributing factors have been identified. Pathophysiology is characterized by progressively expanding nerve cell death originating in substantia nigra, a midbrain region that supplies dopamine to the basal ganglia, a system involved in voluntary motor control. The cause of this cell death is poorly understood but involves alpha-synuclein aggregation into Lewy bodies within the neurons. Other possible factors involve genetic and environmental mechanisms, medications, lifestyle, and previous conditions.
Diagnosis is mainly based on signs and symptoms, usually motor-related, found via neurological examination, though medical imaging like neuromelanin MRI can support the diagnosis. Usual onset is in people over 60 years of age, of whom about one percent are affected. In those younger than 50, it is termed "early-onset PD".
No cure is known; treatment aims to lessen symptoms. Initial treatment typically includes L-DOPA, MAO-B inhibitors, or dopamine agonists. As the disease progresses, these medications become less effective and produce a side effect marked by involuntary muscle movements. Diet and certain forms of rehabilitation have shown some effectiveness at improving symptoms. Deep brain stimulation has been used to reduce severe motor symptoms when drugs are ineffective. There is little evidence for treatment of the non-movement-related symptoms, such as sleep disturbances and mood instability. The average life expectancy is near-normal.
Classification and terminology
[edit]Parkinson's disease (PD) is a neurodegenerative disease affecting both the central and peripheral nervous systems, characterized by the loss of dopamine-producing neurons in the substantia nigra region of the brain.[7] It is classified as a synucleinopathy due to the abnormal accumulation of the protein alpha-synuclein, which aggregates into Lewy bodies within affected neurons.[8]
The loss of dopamine-producing neurons in the substantia nigra initially presents as movement abnormalities, leading to Parkinson's further categorization as a movement disorder.[9] In 30% of cases, disease progression leads to the cognitive decline known as Parkinson's disease dementia (PDD).[10] Alongside dementia with Lewy bodies, PDD is one of the two subtypes of Lewy body dementia.[11]
The four cardinal motor symptoms of Parkinson's—bradykinesia (slowed movements), postural instability, rigidity, and tremor—are called parkinsonism.[12][13] These four symptoms are not exclusive to Parkinson's and can occur in many other conditions,[14][15] including HIV infection and recreational drug use.[16][17] Neurodegenerative diseases that feature parkinsonism but have distinct differences are grouped under the umbrella of Parkinson-plus syndromes or, alternatively, atypical parkinsonian disorders.[18][19] Parkinson's disease can result from genetic factors or be idiopathic, in which there is no clearly identifiable cause. The latter, also called sporadic Parkinson's, makes up some 85–90% of cases.[20]
Signs and symptoms
[edit]The defining symptoms affect the motor system and include tremor, bradykinesia, rigidity, and postural instability. Other symptoms may affect the autonomic or sensory nervous system, mood, behavior, sleep patterns, and cognition.[22]
Non-motor symptoms may precede the onset of motor symptoms by up to 20 years. These include constipation, anosmia, mood disorders, and REM sleep behavior disorder among others.[23] In general, motor symptoms such as postural instability and gait abnormalities tend to appear as the disease progresses.[24]
Motor
[edit]Four motor symptoms are considered as cardinal signs in PD: tremor, bradykinesia, rigidity, and postural instability, collectively known as parkinsonism.[22] However, other motor-associated symptoms are common.
Tremor is the most common presenting sign and may appear at rest as well as during intentional movement with a frequency between 4–6 hertz (cycles per second).[25] PD tremor tends to occur in the hands, but can affect other parts of the body, such as legs, arms, tongue, or lips, as well. It is often described as "pill-rolling", the tendency of the index finger and thumb to touch and perform a circular movement that reminds of the early pharmaceutical technique of manually making pills. Despite it being the most noticeable sign, tremor is present in only about 70–90 percent of cases.[26][25]
Bradykinesia is often considered the most important feature of Parkinson's disease and is also present in atypical parkinsonism. It describes difficulties in motor planning, beginning, and executing, resulting in overall slowed movement with reduced amplitude which affects sequential and simultaneous tasks.[27] Hence, it interferes with daily activities such as dressing, feeding and bathing.[28] Facial muscles involved in bradykinesia lead to the characteristic reduced facial expression known as "masked face" or hypomimia.[29]
Rigidity, also referred to as rigor or "stiffness", is the increased resistance during passive mobilization of a limb affecting up to 89 percent of cases.[30] It usually occurs after onset of tremor and bradykinesia on one or both sides of the body and can lead to muscle or joint pain as the disease progresses.[31] As of 2024, it remains unclear whether rigidity is caused by a distinct biomechanical process or if it is the manifestation of another cardinal sign of PD.[32]
Postural instability (PI) is typical in the later stages of the disease, leading to impaired balance and falls, and secondarily to bone fractures, thus, reduced mobility and quality of life. PI is absent in the initial stages and usually occurs 10–15 years after first diagnosis. Within the first three years after disease onset, PI may indicate atypical parkinsonism.[33] Together with bradykinesia and rigidity, it is responsible for the typical gait characterized by short shuffling steps and forward-flexed posture.[34]
Other common motor signs include a slurred and quiet voice, and handwriting that progressively becomes smaller. This latter may occur prior to other typical symptoms, but the exact neurobiological mechanism, and therefore possible connections with other symptoms, remains unknown.[35]
Sensory
[edit]Transformation of the sensory nervous system can lead to changes in sensation that include an impaired sense of smell, disturbed vision, pain, and paresthesia.[36] Problems with visuospatial function may arise and lead to difficulties in facial recognition and perception of the orientation of drawn lines.[37]
Peripheral neuropathy is known to be present in up to 55 percent of PD patients. While it is responsible for most of paresthesia and pain in Parkingson Disease, its role in postural instability and motor impairment is poorly understood.[36]
Autonomic
[edit]Alterations in the autonomic nervous system, known as dysautonomia, are associated with a variety of symptoms such as gastrointestinal dysfunction, orthostatic hypotension, excessive sweating, or urinary incontinence.[38]
Gastrointestinal issues include constipation, impaired stomach emptying, immoderate production of saliva, and swallowing difficulty (prevalence up to 82 percent). Complications resulting from dysphagia include dehydration, malnutrition, weight loss, and aspiration pneumonia.[39] All gastrointestinal features can be severe enough to cause discomfort, endanger health,[40] and complicate disease management.[41] Despite being related to each other, the exact mechanism of these symptoms remains unknown.[42]
Orthostatic hypotension is the sustained drop of blood pressure by at least 20 mmHg systolic or 10 mmHg diastolic within the first three minutes after raising to an upright position that can be seen in 30–50 percent of cases. Low blood pressure can impair the perfusion of organs situated above the heart, particularly the brain, resulting in lightheadedness. This can eventually lead to fainting and is associated with higher morbidity and mortality.[43]
Other autonomic-related symptoms include excessive sweating, urinary incontinence, and sexual dysfunction.[38]
Neuropsychiatric
[edit]Neuropsychiatric symptoms (NPS) are common and range from mild disturbances to severe impairment, comprising abnormalities in cognition, mood, behavior, or thought which can interfere with daily activities, reduce quality of life, and increase the risk for admission to a nursing home. Some of them, such as depression and anxiety, are known to precede characteristic motor signs by up to several years and may herald the development of PD, while most of them worsen as the disease progresses.[44] Research indicates that patients with more severe motor symptoms are at higher risk for any NPS. Conversely, NPS can worsen PD.[45][46]
Depression is the most common NPS and occurs in nearly half of all patients. It features low mood and lack of pleasure and is more prevalent in women. The diagnosis can be challenging since some symptoms of depression such as psychomotor retardation, memory problems, or altered appetite, share similarities with psychiatric signs caused by PD.[45] It may result in suicidal ideation which is more prevalent in PD. Nonetheless, suicidal attempts themselves are lower than in the general population.[47]
Apathy is characterized by emotional indifference and arises in about 46 percent of cases. Diagnosis is difficult, as it may become indistinct from symptoms of depression.[45]
Anxiety disorders develop in around 43 percent of cases.[45] The most common are panic disorder, generalized anxiety disorder, and social anxiety disorder.[44] Anxiety is known to cause deterioration in the symptoms of PD.[46]
Parkinson's disease psychosis (PDP) is present in around 20 percent of cases[48] and comprises hallucinations, illusions and delusions. It is associated with dopaminergic drugs used to treat the motor symptoms, higher morbidity, mortality, a decrease in health-promoting behaviors, and longer nursing home stays. Additionally, it correlates with depression and may herald onset of dementia in advanced stages. Unlike other psychotic forms, PDP typically presents with a clear sensorium.[49] It might overlap with other psychiatric symptoms, making the diagnosis challenging.[50]
Impulse-control disorders (ICD) can be seen in approximately 19 percent of all patients[45] and, in the context of PD, are grouped along with compulsive behavior and dopamine dysregulation syndrome (DDS) within the broader spectrum of impulsive and compulsive behaviors (ICB). They are characterized by impulsivity and difficulty to control impulsive urges and are positively correlated with the use of dopamine agonists.[51]
Cognitive
[edit]Cognitive disturbances can occur in early stages or before diagnosis, and increase in prevalence and severity with duration of the disease. Ranging from mild cognitive impairment to severe Parkinson's disease dementia, they feature executive dysfunction, slowed cognitive processing speed, and disrupted perception and estimation of time.[52]
Sleep
[edit]Sleep disorders are common in PD and affect about two thirds of all patients.[53] They comprise insomnia, excessive daytime sleepiness (EDS), restless legs syndrome (RLS), REM sleep behavior disorder (RBD), and sleep-disordered breathing (SDB), many of which can be worsened by medication. RBD may begin years prior to the initial motor symptoms. Individual presentation of symptoms vary, although most of people affected by PD show an altered circadian rhythm at some point of disease progression.[54][55]
Other
[edit]PD is associated with a variety of skin disorders that include melanoma, seborrheic dermatitis, bullous pemphigoid, and rosacea.[56] Seborrheic dermatitis is recognized as a premotor feature that indicates dysautonomia and demonstrates that PD can be detected not only by changes of nervous tissue, but tissue abnormalities outside the nervous system as well.[57]
Causes and risk factors
[edit]
As of 2024, the underlying cause of PD is unknown,[58] yet is assumed to be influenced primarily by an interaction of genetic and environmental factors.[59] Nonetheless, the most significant risk factor is age with a prevalence of 1 percent in those aged over 65 and approximately 4.3 percent in age over 85.[60] Genetic components comprise SNCA, LRRK2, and PARK2 among others, while environmental risks include exposure to pesticides or heavy metals.[61] Timing of exposure factor may influence the progression or severity of certain stages.[62]: 46 However, caffeine and nicotine exhibit neuroprotective features, hence lowering the risk of PD.[63][64] About 85 percent of cases occur sporadic, meaning that there is no family history.[65]
Genetic
[edit]PD, in a narrow sense, can be seen as a genetic disease; heritability is estimated to lie between 22 and 40 percent,[59] across different ethnicities.[66] Around 15 percent of diagnosed individuals have a family history, from which 5–10 percent can be attributed to a causative risk gene mutation, although harboring one of these mutations may not lead to the disease.[65]
As of 2024, around 90 genetic risk variants across 78 genomic loci have been identified with studies employing next-generation sequencing (NGS) to uncover detailed insights into these genetic factors.[67] Notable risk genes include SNCA,[68] LRRK2, and VPS35 for autosomal dominant inheritance, and PRKN, PINK1, and DJ1 for autosomal recessive inheritance.[59] LRRK2 is estimated to be responsible for 1-2% of all cases of PD and 40% of familial cases.[69] Additionally, mutations in the GBA1 gene, linked to Gaucher's disease, are found in 5–10 percent of PD cases.[70] The GBA1 variant of genetic PD more commonly involves cognitive decline.[69]
Alpha-synuclein (aSyn), a protein encoded by SNCA gene, is thought to be primarily responsible Lewy body aggregation.[71] ASyn activates ATM serine/threonine kinase, a major DNA damage-repair signaling kinase,[72] and non-homologous end joining DNA repair pathway.[72]
Environmental
[edit]Identifying environmental risk factors and causality is difficult due to the disease's often decade-long prodromal period.[62]: 46 Most noteworthy environmental factors include pesticide exposure and contact with heavy metals.
In particular, exposure to pesticides such as paraquat, rotenone, benomyl, and mancozeb causes one in five cases,[73] implying an association with the onset of PD.[62] Risk is increased by co-exposure to, for example, glyphosate and MPTP.[74]
Harmful heavy metals include mainly manganese, iron, lead, mercury,[75] aluminium, and cadmium. On the other hand, magnesium shows neuroprotective features.[76]
Other chemical compounds include trichloroethylene[77] and MPTP.[78]
Other
[edit]Traumatic brain injury is also strongly implicated as a risk factor.[79] Additionally, although the underlying cause is unknown, melanoma is documented to be associated with PD.[80] Low levels of urate in the blood are associated with an increased risk[81] while Helicobacter pylori infection can prevent the absorption of some drugs, including L-DOPA.[82]
Pathophysiology
[edit]Main pathological feature is cell death of dopamine-releasing neurons within, among other regions, the basal ganglia, more precisely pars compacta of substantia nigra and partially striatum, thus impeding nigrostriatal pathway of the dopaminergic system which plays a central role in motor control.[83]
Neuroanatomy
[edit]Three major pathways connect the basal ganglia to other brain areas: direct, indirect, and hyperdirect pathway, all part of the cortico-basal ganglia-thalamo-cortical loop.[84]
The direct pathway projects from the neocortex to putamen or caudate nucleus of the striatum, which sends inhibitory GABAergic signals to substantia nigra pars reticulata (SNpr) and internal globus pallidus (GPi).[84] This inhibition reduces GABAergic signaling to ventral lateral (VL) and ventral anterior (VA) nuclei of the thalamus, thereby promoting their projections to the motor cortex.[85]
The indirect pathway projects inhibition from striatum to external globus pallidus (GPe), reducing its GABAergic inhibition of the subthalamic nucleus, pars reticulata and internal globus pallidus. This reduction in inhibition allows the subthalamic nucleus to excite internal globus pallidus and pars reticulata, which in turn inhibit thalamic activity, thereby suppressing excitatory signals to the motor cortex.[84]
The hyperdirect pathway is an additional glutamatergic pathway that projects from the frontal lobe to subthalamic nucleus, modulating basal ganglia activity with rapid excitatory input.[86]
The striatum and other basal ganglia structures contain D1 and D2 receptor neurons that modulate the previously described pathways. Consequently, dopaminergic dysfunction in these systems can disrupt their respective components—motor, oculomotor, associative, limbic, and orbitofrontal circuits (each named for its primary projection area)—leading to symptoms related to movement, attention, and learning in the disease.[87]
Mechanisms
[edit]Neuronal cell death has been linked to noumerous mechanisms, with the most prominent being the misfolding and aggregation of alpha-synuclein, oxidative stress, neuroinflammation, ferroptosis, mitochondrial dysfunction, and gut dysbiosis.[88]
Alpha-synuclein and Lewy bodies
[edit]Alpha-synuclein (aSyn), a protein involved in synaptic vesicle trafficking, intracellular transport, and neurotransmitter release, is considered one of the primary contributing factors for nigrostriatal neuron death in PD. When overexpressed or misfolded, it can form clumps[89] on axon terminals and other neuronal structures, particularly its typical locations: the cytoplasm, mitochondria and nucleus. These aggregates eventually lead to the formation of Lewy bodies. Their precursors, known as oligomers, along with initial deposits called pale bodies, are believed to play a direct role in neurodegeneration, while Lewy bodies are thought to serve as an indirect marker of disease progression.[90]
A vicious cycle linked to neurodegeneration involves oxidative stress, mitochondria, and neuroimmune function, particularly inflammation. Normal metabolism of dopamine tends to fail, leading to elevated levels of reactive oxygen species (ROS) which is cytotoxic and causes cellular damage to lipids, proteins, DNA, and especially mitochondria.[91] Mitochondrial damage triggers neuroinflammatory responses via damage-associated molecular patterns (DAMPs), resulting in aggregation of neuromelanin, and therefore, fueling further neuroinflammation by activating microglia.[92]
Ferroptosis is suggested as another significant mechanism in disease progression. It is characterized by cell death through high levels of lipid hydroperoxide.[93]
Other mechanisms include proteasomal and lysosomal systems dysfunction and reduced mitochondrial activity.[94] Iron accumulation in the substantia nigra is typically observed in conjunction with the protein inclusions. It may be related to oxidative stress, protein aggregation, and neuronal death, but the mechanisms are obscure.[95]
Neuroimmune interaction
[edit]The neuroimmune interaction is heavily implicated in PD pathology. PD and autoimmune disorders share genetic variations and molecular pathways. Some autoimmune diseases may even increase one's risk of developing PD, up to 33% in one study.[96] Autoimmune diseases linked to protein expression profiles of monocytes and CD4+ T cells are linked to PD. Herpes virus infections can trigger autoimmune reactions to alpha-synuclein, perhaps through molecular mimicry of viral proteins.[97] Alpha-synuclein, and its aggregate form, Lewy bodies, can bind to microglia. Microglia can proliferate and be over-activated by alpha-synuclein binding to MHC receptors on inflammasomes, bringing about a release of proinflammatory cytokines like IL-1β, IFNγ, and TNFα.[98]
Activated microglia influence the activation of astrocytes, converting their neuroprotective phenotype to a neurotoxic one. Astrocytes in healthy brains serve to protect neuronal connections. In Parkinson's disease, astrocytes cannot protect the dopaminergic connections in the striatum. Microglia present antigens via MHC-I and MHC-II to T cells. CD4+ T cells, activated by this process, are able to cross the blood brain barrier (BBB) and release more proinflammatory cytokines, like interferon-γ (IFNγ), TNFα, and IL-1β. Mast cell degranulation and subsequent proinflammatory cytokine release is implicated in BBB breakdown in PD. Another immune cell implicated in PD are peripheral monocytes and have been found in the substantia nigra of people with PD. These monocytes can lead to more dopaminergic connection breakdown. In addition, monocytes isolated from people with Parkinson's disease express higher levels of the PD-associated protein, LRRK2, compared with non-PD individuals via vasodilation.[99] In addition, high levels of pro-inflammatory cytokines, such as IL-6, can lead to the production of C-reactive protein by the liver, another protein commonly found in people with PD, that can lead to an increase in peripheral inflammation.[100][101]
Peripheral inflammation can affect the gut-brain axis, an area of the body highly implicated in PD. People with PD have altered gut microbiota and colon problems years before motor issues arise.[100][101] Alpha-synuclein is produced in the gut and may migrate via the vagus nerve to the brainstem, and then to the substantia nigra.[undue weight? – discuss][better source needed][102]
Diagnosis
[edit]
Physician's initial assessment is typically based on medical history and neurological examination.[103] They assess motor symptoms (bradykinesia, rest tremors, etc.) using clinical diagnostic criteria. The finding of Lewy bodies in the midbrain on autopsy is usually considered final proof that the person had PD. The clinical course of the illness over time may diverge from PD, requiring that presentation is periodically reviewed to confirm the accuracy of the diagnosis.[103][104]
Multiple causes can occur for parkinsonism or diseases that look similar. Stroke, certain medications, and toxins can cause "secondary parkinsonism" and need to be assessed during visit.[105][104] Parkinson-plus syndromes, such as progressive supranuclear palsy and multiple system atrophy, must be considered and ruled out appropriately to begin a different treatment and disease progression (anti-Parkinson's medications are typically less effective at controlling symptoms in Parkinson-plus syndromes).[103] Faster progression rates, early cognitive dysfunction or postural instability, minimal tremor, or symmetry at onset may indicate a Parkinson-plus disease rather than PD itself.[106]
Medical organizations have created diagnostic criteria to ease and standardize the diagnostic process, especially in the early stages of the disease. The most widely known criteria come from the UK Queen Square Brain Bank for Neurological Disorders and the U.S. National Institute of Neurological Disorders and Stroke. The Queen Square Brain Bank criteria require slowness of movement (bradykinesia) plus either rigidity, resting tremor, or postural instability. Other possible causes of these symptoms need to be ruled out. Finally, three or more of the following supportive symptoms are required during onset or evolution: unilateral onset, tremor at rest, progression in time, asymmetry of motor symptoms, response to levodopa for at least five years, the clinical course of at least ten years and appearance of dyskinesias induced by the intake of excessive levodopa.[107] If a suspected case of PD does not respond to levodopa then the diagnosis should be reconsidered.[69] Assessment of sudomotor function through electrochemical skin conductance can be helpful in diagnosing dysautonomia.[108]
When PD diagnoses are checked by autopsy, movement disorders experts are found on average to be 79.6% accurate at initial assessment and 83.9% accurate after refining diagnoses at follow-up examinations. When clinical diagnoses performed mainly by nonexperts are checked by autopsy, the average accuracy is 73.8%. Overall, 80.6% of PD diagnoses are accurate, and 82.7% of diagnoses using the Brain Bank criteria are accurate.[109]
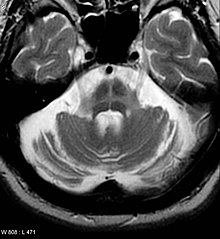
Imaging
[edit]Computed tomography (CT) scans of people with PD usually appear normal.[110] Magnetic resonance imaging has become more accurate in diagnosis of the disease over time, specifically through iron-sensitive T2* and susceptibility weighted imaging sequences at a magnetic field strength of at least 3T, both of which can demonstrate absence of the characteristic 'swallow tail' imaging pattern in the dorsolateral substantia nigra.[111] In a meta-analysis, absence of this pattern was highly sensitive and specific for the disease.[112] A meta-analysis found that neuromelanin-MRI can discriminate individuals with Parkinson's from healthy subjects.[113] Diffusion MRI has shown potential in distinguishing between PD and Parkinson-plus syndromes, as well as between PD motor subtypes,[114] though its diagnostic value is still under investigation.[110] CT and MRI are used to rule out other diseases that can be secondary causes of parkinsonism, most commonly encephalitis and chronic ischemic insults, as well as less-frequent entities such as basal ganglia tumors and hydrocephalus.[110]
The metabolic activity of dopamine transporters in the basal ganglia can be directly measured with positron emission tomography and single-photon emission computed tomography scans. It has shown high agreement with clinical diagnoses of PD.[115] Reduced dopamine-related activity in the basal ganglia can help exclude drug-induced Parkinsonism. This finding is nonspecific and can be seen with both PD and Parkinson-plus disorders.[110] In the United States, DaTSCANs are only FDA approved to distinguish PD or Parkinsonian syndromes from essential tremor.[116]
Iodine-123-meta-iodobenzylguanidine myocardial scintigraphy can help locate denervation of the muscles of the heart which can support a PD diagnosis.[105]
Differential diagnosis
[edit]Secondary parkinsonism – The multiple causes of parkinsonism can be differentiated through careful history, physical examination, and appropriate imaging.[105][117] Other Parkinson-plus syndromes can have similar movement symptoms but have a variety of associated symptoms. Some of these are also synucleinopathies. Lewy body dementia involves motor symptoms with early onset of cognitive dysfunction and hallucinations which precede motor symptoms. Alternatively, multiple systems atrophy or MSA usually has early onset of autonomic dysfunction (such as orthostasis), and may have autonomic predominance, cerebellar symptom predominance, or Parkinsonian predominance.[118]
Other Parkinson-plus syndromes involve tau, rather than alpha-synuclein. These include progressive supranuclear palsy (PSP) and corticobasal syndrome (CBS). PSP predominantly involves rigidity, early falls, bulbar symptoms, and vertical gaze restriction; it can be associated with frontotemporal dementia symptoms. CBS involves asymmetric parkinsonism, dystonia, alien limb, and myoclonic jerking.[119] Presentation timelines and associated symptoms can help differentiate similar movement disorders from idiopathic Parkinson disease.[medical citation needed]
Vascular parkinsonism is the phenomenon of the presence of Parkinson's disease symptoms combined with findings of vascular events (such as a cerebral stroke). The damaging of the dopaminergic pathways is similar in cause for both vascular parkinsonism and idiopathic PD, and so present with similar symptoms. Differentiation can be made with careful bedside examination, history evaluation, and imaging.[120][121]
Parkinson-plus syndrome – Multiple diseases can be considered part of the Parkinson's plus group, including corticobasal syndrome, multiple system atrophy, progressive supranuclear palsy, and dementia with Lewy bodies. Differential diagnosis can be narrowed down with careful history and physical exam (especially focused on the sequential onset of specific symptoms), progression of the disease, and response to treatment.[122][117] Some key symptoms:[123][117]
- Corticobasal syndrome – levodopa-resistance, myoclonus, dystonia, corticosensory loss, apraxia, and non-fluent aphasia
- Dementia with Lewy bodies – levodopa resistance, cognitive predominance before motor symptoms, and fluctuating cognitive symptoms, (visual hallucinations are common in this disease)
- Essential tremor – This can at first look like parkinsonism, but has key differentiators. In essential tremor, the tremor gets worse with action (improves in PD), a lack of other symptoms is common in PD, and normal DatSCAN is seen.[117]
- Multiple system atrophy – levodopa resistance, rapidly progressive, autonomic failure, stridor, present Babinski sign, cerebellar ataxia, and specific MRI findings
- Progressive supranuclear palsy – levodopa resistance, restrictive vertical gaze, specific MRI findings, and early and different postural difficulties
Prevention
[edit]
As of 2024, no disease-modifying therapies exist that reverse or slow neurodegeneration, processes respectively termed neurorestoration and neuroprotection.[124][125] However, several factors have been found to be associated with a decreased risk.[124] The identification and mechanistic analysis of these factors may guide the development of new therapies.[126]
Exercise—one of the most common recommendations to prevent or delay Parkinson's—may exert a neuroprotective effect.[127] In animal studies investigating the cellular basis, exercise has been found to increase neurotrophic growth factor expression and to reduce alpha-synuclein expression, neuroinflammation, and mitochondrial dysfunction.[128]
Tobacco use and smoking is strongly associated with a decreased risk, reducing the chance of developing PD by 40–60%.[129][130] Various tobacco and smoke components have been hypothesized to be neuroprotective, including nicotine, carbon monoxide, and monoamine oxidase B inhibitors.[131][132] Consumption of coffee, tea, or caffeine is also strongly associated with neuroprotection.[133][134] In laboratory models, caffeine has been shown to be neuroprotective due to its antagonistic interaction with the adenosine A2A receptor, which modulates dopaminergic signaling, synaptic plasticity, synapse formation, and inflammation.[131] Prescribed adrenergic antagonists like terazosin may also reduce risk.[133]
Although findings have varied, usage of nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen may be neuroprotective.[135][136] Calcium channel blockers (CCB) may also have a protective effect, with a 22% risk decrease found in a 2024 meta-analysis of almost 3 million CCB users.[137] Higher blood concentrations of urate—a potent antioxidant—have been proposed to be neuroprotective;[131][138] animal and cell studies have shown that urate can prevent dopaminergic neurodegeneration.[138] Although longitudinal studies observe a slight decrease in PD risk among those who consume alcohol—possibly due to alcohol's urate-increasing effect—alcohol abuse may increase risk.[139][140]
Management
[edit]Despite ongoing research efforts, Parkinson's disease has no known cure. Patients are typically managed by a holistic approach that combines lifestyle modifications with physical therapy. Certain medications may also be used to provide symptomatic relief and improve the patient's quality of life. The medications used in Parkinson's disease work by either increasing endogenous dopamine levels or by directly mimicking dopamine's effect on the patient's brain. Levodopa (L-dopa) is the most effective for motor symptoms and is often combined with a dopa decarboxylase inhibitor (such as carbidopa or benserazide).[141] Other agents include COMT inhibitors, dopamine agonists, and MAO-B inhibitors. The patient's age at disease onset as well as the stage of the disease often help determine which of the aforementioned drug groups is most effective.
Braak staging classifies the degree of pathology in patients with Parkinson's disease into six stages that correlate with early, middle, and late presentations of the disease.[142] Treatment in the first stage aims for an optimal trade-off between symptom control and medication side effects. For example, the administration of levodopa in this stage may be delayed in favor of other agents, such as MAO-B inhibitors and dopamine agonists, due to its notable risk of complications.[143] However, levodopa-related dyskinesias still correlate more strongly with the duration and severity of the disease than the duration of levodopa treatment.[144] A careful consideration of the risks and benefits of starting treatment is crucial to optimize patient outcomes. In the middle stages of Parkinson's disease, the primary aim is to reduce patient symptoms. Episodes of medication overuse or any sudden withdrawals from medication must be promptly managed.[143] If medications prove ineffective, surgery (such as deep brain stimulation or high-intensity focused ultrasound[145]), subcutaneous waking-day apomorphine infusion, and enteral dopa pumps may be useful.[146] Late-stage Parkinson's disease presents challenges requiring a variety of treatments, including those for psychiatric symptoms particularly depression, orthostatic hypotension, bladder dysfunction, and erectile dysfunction.[146] In the final stages of the disease, palliative care is provided to improve a person's quality of life.[147]
A 2020 Cochrane review found no certain evidence that cognitive training is beneficial for people with Parkinson's disease, dementia or mild cognitive impairment.[148] The findings are based on low certainty evidence of seven studies.
No standard treatment for PD-associated anxiety exists.[149][page needed]
Medications
[edit]
Levodopa
[edit]Levodopa (L-DOPA) is usually the first drug of choice when treating Parkinson's disease and has been the most widely used PD treatment since the 1980s.[143][150] The motor symptoms of PD are the result of reduced dopamine production in the brain's basal ganglia. Dopamine fails to cross the blood–brain barrier so it cannot be taken as a medicine to boost the brain's depleted levels of dopamine. A precursor of dopamine, levodopa, can pass through to the brain where it is readily converted to dopamine. Administration of levodopa temporarily diminishes the motor symptoms of PD.
Only 5–10% of levodopa crosses the blood–brain barrier. Much of the remainder is metabolized to dopamine elsewhere in the body, causing a variety of side-effects, including nausea, vomiting, and orthostatic hypotension.[151] Carbidopa and benserazide are dopa decarboxylase inhibitors that fail to cross the blood–brain barrier and inhibit the conversion of levodopa to dopamine outside the brain, reducing side-effects and improving the availability of levodopa for passage into the brain. One of these drugs is usually taken along with levodopa and is available combined with levodopa in the same pill.[152]
Prolonged use of levodopa is associated with the development of complications, such as involuntary movements (dyskinesias) and fluctuations in the impact of the medication.[143] When fluctuations occur, a person can cycle through phases with good response to medication and reduced PD symptoms ("on state"), and phases with poor response to medication and increased PD symptoms ("off state").[143][153] Using lower doses of levodopa may reduce the risk and severity of these levodopa-induced complications.[154] A former strategy, called "drug holidays", to reduce levodopa-related dyskinesia and fluctuations was to withdraw levodopa medication for some time,[150] which can bring on dangerous side-effects such as neuroleptic malignant syndrome and is discouraged.[143] Most people with PD eventually need levodopa and later develop levodopa-induced fluctuations and dyskinesias.[143] Adverse effects of levodopa, including dyskinesias, may mistakenly influence people affected by the disease and sometimes their healthcare professionals to delay treatment, which reduces potential for optimal results.[medical citation needed]
Levodopa is available in oral, inhalation, and infusion form; inhaled levodopa can be used when oral levodopa therapy has reached a point where "off" periods have increased in length.[155][156]
The fixed-dose combination foscarbidopa/foslevodopa (Vyalev) is approved for medical use in Canada,[157] in Australia,[158] and in the United States.[159][160] It is a fixed-dose combination of foscarbidopa, an aromatic amino acid decarboxylation inhibitor and prodrug for carbidopa; and foslevodopa, an aromatic amino acid and prodrug for levodopa.[159]
COMT inhibitors
[edit]
During the course of PD, affected people can experience a wearing-off phenomenon, where a recurrence of symptoms occurs after a dose of levodopa, but right before their next dose.[105] Catechol-O-methyltransferase (COMT) is a protein that degrades levodopa before it can cross the blood–brain barrier and COMT inhibitors allow for more levodopa to cross.[162] They are normally used in the management of later symptoms, but can be used in conjunction with levodopa/carbidopa when a person is experiencing the wearing off-phenomenon with their motor symptoms.[105][150]
Three COMT inhibitors are used to treat adults with PD and end-of-dose motor fluctuations – opicapone, entacapone, and tolcapone.[105] Tolcapone has been available for but its usefulness is limited by possible liver damage complications requiring liver-function monitoring.[163][105][162][123] Entacapone and opicapone cause little alteration to liver function.[162][164][165] Licensed preparations of entacapone contain entacapone alone or in combination with carbidopa and levodopa.[166][123][167] Opicapone is a once-daily COMT inhibitor.[168][105]
Dopamine agonists
[edit]Dopamine agonists that bind to dopamine receptors in the brain have similar effects to levodopa.[143] These were initially used as a complementary therapy to levodopa for individuals experiencing levodopa complications (on-off fluctuations and dyskinesias); they are mainly used on their own as first therapy for the motor symptoms of PD with the aim of delaying the initiation of levodopa therapy, thus delaying the onset of levodopa's complications.[143][169] Dopamine agonists include bromocriptine, pergolide, pramipexole, ropinirole, piribedil, cabergoline, apomorphine, and lisuride.
Though dopamine agonists are less effective than levodopa at controlling PD motor symptoms, they are effective enough to manage these symptoms in the first years of treatment.[170] Dyskinesias due to dopamine agonists are rare in younger people who have PD, but along with other complications, become more common with older age at onset.[170] Thus, dopamine agonists are the preferred initial treatment for younger-onset PD, and levodopa is preferred for older-onset PD.[170]
Dopamine agonists produce side effects, including drowsiness, hallucinations, insomnia, nausea, and constipation.[143][150] Side effects appear with minimal clinically effective doses giving the physician reason to search for a different drug.[143] Agonists have been related to impulse-control disorders (such as increased sexual activity, eating, gambling, and shopping) more strongly than other antiparkinson medications.[171][150]
Apomorphine, a dopamine agonist, may be used to reduce off periods and dyskinesia in late PD.[143] It is administered only by intermittent injections or continuous subcutaneous infusions.[143] Secondary effects such as confusion and hallucinations are common, individuals receiving apomorphine treatment should be closely monitored.[143] Two dopamine agonists administered through skin patches (lisuride and rotigotine) are useful for people in the initial stages and possibly to control off states in those in advanced states.[172][page needed] Due to an increased risk of cardiac fibrosis with ergot-derived dopamine agonists (bromocriptine, cabergoline, dihydroergocryptine, lisuride, and pergolide), they should only be considered for adjunct therapy to levodopa.[150]
MAO-B inhibitors
[edit]MAO-B inhibitors (safinamide, selegiline and rasagiline) increase the amount of dopamine in the basal ganglia by inhibiting the activity of monoamine oxidase B, an enzyme that breaks down dopamine.[143] They have been found to help alleviate motor symptoms when used as monotherapy (on their own); when used in conjunction with levodopa, time spent in the off phase is reduced.[173][150] Selegiline has been shown to delay the need for beginning levodopa, suggesting that it might be neuroprotective and slow the progression of the disease.[174] An initial study indicated that selegiline in combination with levodopa increased the risk of death, but this has been refuted.[175]
Common side effects are nausea, dizziness, insomnia, sleepiness, and (in selegiline and rasagiline) orthostatic hypotension.[174][105] MAO-Bs are known to increase serotonin and cause a potentially dangerous condition known as serotonin syndrome.[174]
Other drugs
[edit]Treatments for non-motor symptoms of PD have not been well studied and many medications are used off-label.[69] Drugs such as amantadine may be useful as treatment of motor symptoms, but evidence for use is lacking.[143][176] Anticholinergics should not be used for dyskinesia or motor fluctuations but may be considered topically for drooling.[150] A diverse range of symptoms beyond those related to motor function can be treated pharmaceutically.[177] Examples are the use of quetiapine or clozapine for psychosis, cholinesterase inhibitors (such as rivastigmine) or memantine for dementia, and modafinil for excessive daytime sleepiness.[177][178][150][179] In 2016, pimavanserin was approved for the management of PD psychosis.[180] Doxepin and rasagline may reduce physical fatigue in PD.[181] Fludrocortisone, midodrine and droxidopa are commonly used off label for orthostatic hypotension related to autonomic dysfunction.[69] Sublingual atropine or botulinum toxin injections may be used off-label for drooling. SSRIs, SNRIs and cognitive behavior therapy are often used for depression related to PD, but there is a risk of serotonin syndrome with the SSRI or SNRI antidepressants.[69]
Surgery
[edit]
Treating motor symptoms with surgery was once a common practice but the discovery of levodopa has decreased the amount of procedures.[182] Studies have led to great improvements in surgical techniques, so surgery can be used in people with advanced PD for whom drug therapy is no longer sufficient.[182] Surgery for PD can be divided in two main groups – lesional and deep brain stimulation (DBS). Target areas for DBS or lesions include the thalamus, globus pallidus, or subthalamic nucleus.[182] DBS involves the implantation of a medical device called a neurostimulator, which sends electrical impulses to specific parts of the brain. DBS is recommended for people who have PD with motor fluctuations and tremor inadequately controlled by medication, or to those who are intolerant to medication lacking severe neuropsychiatric problems.[183] Other less common surgical therapies involve intentional formation of lesions to suppress overactivity of specific subcortical areas. For example, pallidotomy involves surgical destruction of the globus pallidus to control dyskinesia.[182]
Four areas of the brain have been treated with neural stimulators in PD.[184] These are the globus pallidus interna, thalamus, subthalamic nucleus, and pedunculopontine nucleus. DBS of the globus pallidus interna improves motor function, while DBS of the thalamic DBS improves tremor, but has little impact on bradykinesia or rigidity. DBS of the subthalamic nucleus is usually avoided if a history of depression or neurocognitive impairment is present. DBS of the subthalamic nucleus is associated with a reduction in medication. Pedunculopontine nucleus DBS remains experimental at present. Generally, DBS is associated with 30–60% improvement in motor score evaluations.[184]
Rehabilitation
[edit]Exercise programs are recommended in people with PD and recent reviews (2024) have demonstrated their efficacy.[185][186] Some evidence shows that speech or mobility problems can improve with rehabilitation, although studies are scarce and of low quality.[187][188] Regular physical exercise with or without physical therapy can be beneficial to maintain and improve mobility, flexibility, strength, gait speed, and quality of life.[188] When an exercise program is performed under the supervision of a physiotherapist, more improvements occur in motor symptoms, mental and emotional functions, daily living activities, and quality of life compared with a self-supervised exercise program at home.[189] Clinical exercises may be an effective intervention targeting overall well-being of individuals with Parkinson's. Improvement in motor function and depression may happen.[190]
In improving flexibility and range of motion for people experiencing rigidity, generalized relaxation techniques such as gentle rocking have been found to decrease excessive muscle tension. Other effective techniques to promote relaxation include slow rotational movements of the extremities and trunk, rhythmic initiation, diaphragmatic breathing, and meditation techniques.[191] As for gait and addressing the challenges associated with the disease such as hypokinesia, shuffling, and decreased arm swing, physiotherapists have a variety of strategies to improve functional mobility and safety. Areas of interest concerning gait during rehabilitation programs focus on improving gait speed, the base of support, stride length, and trunk and arm-swing movement. Strategies include using assistive equipment (pole walking and treadmill walking), verbal cueing (manual, visual, and auditory), exercises (marching and PNF patterns), and altering environments (surfaces, inputs, open vs. closed).[192] Strengthening exercises have shown improvements in strength and motor function for people with primary muscular weakness and weakness related to inactivity with mild to moderate PD, but reports show an interaction between strength and the time the medications were taken. Therefore, people with PD should perform exercises 45 minutes to one hour after medications when they are capable.[193] Deep diaphragmatic breathing exercises are beneficial in improving chest-wall mobility and vital capacity decreased by a forward flexed posture and respiratory dysfunctions in advanced PD.[194] Exercise may improve constipation.[195] Whether exercise reduces physical fatigue in PD remains unclear.[181]
Strength training exercise has been shown to increase manual dexterity in people with PD after exercising with manual putty. Improvements in both manual dexterity and strength can have a favorable impact on people with Parkinson's disease, fostering increased independence in daily activities that require grasping objects.[196]
The Lee Silverman voice treatment (LSVT) is one of the most widely practiced treatments for speech disorders associated with PD.[187][197] Speech therapy and specifically LSVT may improve speech.[187] Occupational therapy (OT) aims to promote health and quality of life by helping people with the disease to participate in a large percentage of their daily living activities.[187] Few studies have been conducted on the effectiveness of OT, and their quality is poor, although with some indication that it may improve motor skills and quality of life for the duration of the therapy.[187][198]
Palliative care
[edit]The goal of palliative care is to improve quality of life for both the patient and family by providing relief from the symptoms and stress of illnesses.[199] As Parkinson's is uncurable, treatments focus on slowing decline and improving quality of life and are therefore palliative.[200]
Palliative care should be involved earlier, rather than later, in the disease course.[201][202] Palliative care specialists can help with physical symptoms, emotional factors such as loss of function and jobs, depression, fear, and existential concerns.[201][202][203]
Along with offering emotional support to both the affected person and family, palliative care addresses goals of care. People with PD may have difficult decisions to make as the disease progresses, such as wishes for feeding tube, noninvasive ventilator or tracheostomy, wishes for or against cardiopulmonary resuscitation, and when to use hospice care.[200] Palliative-care team members can help answer questions and guide people with PD on these complex and emotional topics to help them make decisions based on values.[202][204]
Muscles and nerves that control the digestive process may be affected by PD, resulting in constipation and gastroparesis (prolonged emptying of stomach contents).[195] A balanced diet, based on periodical nutritional assessments, is recommended, and should be designed to avoid weight loss or gain and minimize the consequences of gastrointestinal dysfunction.[195] As the disease advances, swallowing difficulties (dysphagia) may appear. Using thickening agents for liquid intake and an upright posture when eating may be useful; both measures reduce the risk of choking. Gastrostomy can be used to deliver food directly into the stomach.[195]
Levodopa and proteins use the same transportation system in the intestine and the blood–brain barrier, thereby competing for access.[195] Taking them together results in reduced effectiveness of the drug.[195] Therefore, when levodopa is introduced, excessive protein consumption is discouraged in favour of a well-balanced Mediterranean diet. In advanced stages, additional intake of low-protein products such as bread or pasta is recommended for similar reasons.[195] To minimize interaction with proteins, levodopa should be taken 30 minutes before meals.[195] At the same time, regimens for PD restrict proteins during breakfast and lunch, allowing protein intake in the evening.[195]
Prognosis
[edit]| Parkinson's subtype | Mean years post-diagnosis until: | |
|---|---|---|
| Severe cognitive or movement abnormalities[note 1] | Death | |
| Mild-motor predominant | 14.3 | 20.2 |
| Intermediate | 8.2 | 13.1 |
| Diffuse malignant | 3.5 | 8.1 |
As Parkinson's is a heterogeneous condition with multiple etiologies, prognistication can be difficult and prognoses can be highly variable.[205][207] On average, life expectancy is reduced in those with Parkinson's, with younger age of onset resulting in greater life expectancy decreases.[208] Although PD subtype categorization is controversial, the 2017 Parkinson's Progression Markers Initiative study identified three broad scorable subtypes of increasing severity and more rapid progression: mild-motor predominant, intermediate, and diffuse malignant. Mean years of survival post diagnosis were 20.2, 13.1, and 8.1.[205]
Around 30% of Parkinson's patients develop dementia, and is 12 times more likely to occur in elderly patients of those with severe PD.[209] Dementia is less likely to arise in patients with tremor-dominant PD.[210] Parkinson's disease dementia is associated with a reduced quality of life in people with PD and their caregivers, increased mortality, and a higher probability of needing nursing home care.[211]
The incidence rate of falls in Parkinson's patients is approximately 45 to 68%, thrice that of healthy individuals, and half of such falls result in serious secondary injuries. Falls increase morbidity and mortality.[212] Around 90% of those with PD develop hypokinetic dysarthria, which worsens with disease progession and can hinder communication.[213] Additionally, over 80% of PD patients develop dysphagia: consequent inhalation of gastric and oropharyngeal secretions can lead to aspiration pneumonia.[214] Aspiration pneumonia is responsible for 70% of deaths in those with PD.[215]
Epidemiology
[edit]
As of 2024, Parkinson's is the second most common neurodegenerative disease and the fastest-growing in total number of cases.[216][217] As of 2023, global prevalence was estimated to be 1.51 per 1000.[218] Although it is around 40% more common in men,[219] age is the dominant predeterminant of Parkinson's.[220] Consequently, as global life expectancy has increased, Parkinson's disease prevalence has also risen, with an estimated increase in cases by 74% from 1990 to 2016.[221] The total number is predicted to rise to over 12 million patients by 2040.[222] Some label this a pandemic.[221]
This increase may be due to a number of global factors, including prolonged life expectancy, increased industrialisation, and decreased smoking.[221] Although genetics is the sole factor in a minority of cases, most cases of Parkinson's are likely a result of gene-environment interactions: concordance studies with twins have found Parkinson's heritability to be just 30%.[219] The influence of multiple genetic and environmental factors complicates epidemiological efforts.[223]
Relative to Europe and North America, disease prevalence is lower in Africa—especially sub-Saharan Africa—but similar in Latin America.[224] Although China is predicted to have nearly half of the global Parkinson's population by 2030,[225] estimates of prevalence in Asia have varied.[224] Potential explanations for these geographic differences include genetic variation, environmental factors, health care access, and life expectancy.[224] Although PD incidence and prevalence may vary by race and ethnicity, significant disparities in care, diagnosis, and study participation limit generalizability and lead to conflicting results.[224][223] Within the United States, high rates of PD have been identified in the Midwest and South, as well as agricultural regions of California, Florida, Pennsylvania, and Texas: collectively termed the "PD belt".[226] The association between rural residence and Parkinson's has been hypothesized to be caused by environmental factors like herbicides, pesticides, and industrial waste.[226][227]
History
[edit]In 1817, English physician James Parkinson published the first full medical description of the disease as a neurological syndrome in his monograph An Essay on the Shaking Palsy.[229][230] He presented six clinical cases, including three he had observed on the streets near Hoxton Square in London.[231] Parkinson described three cardinal symptoms: tremor, postural instability and "paralysis" (undistinguished from rigidity or bradykinesia), and speculated that the disease was caused by trauma to the spinal cord.[232][233]
There was little discussion or investigation of the "shaking palsy" until 1861, when Frenchman Jean-Martin Charcot—regarded as the father of neurology—began expanding Parkinson's description, adding bradykinesia as one of the four cardinal symptoms.[232][231][233] In 1877, Charcot renamed the disease after Parkinson, as not all patients displayed the tremor suggested by "shaking palsy".[231][233] Subsequent neurologists who made early advances to the understanding of Parkinson's include Armand Trousseau, William Gowers, Samuel Kinnier Wilson, and Wilhelm Erb.[234]

Although Parkinson is typically credited with the first detailed description of PD, many previous texts reference some of the disease's clinical signs.[235] In his essay, Parkinson himself acknowledged partial descriptions by Galen, William Cullen, Johann Juncker, and others.[233] Possible earlier but incomplete descriptions include a Nineteenth Dynasty Egyptian papyrus, the ayurvedic text Charaka Samhita, Ecclesiastes 12:3, and a discussion of tremors by Leonardo da Vinci.[233][236] Multiple traditional Chinese medicine texts may include references to PD, including a discussion in the Yellow Emperor's Internal Classic (c. 425–221 BC) of a disease with symptoms of tremor, stiffness, staring, and stooped posture.[236] In 2009, a systematic description of PD was found in the Hungarian medical text Pax corporis written by Ferenc Pápai Páriz in 1690, some 120 years before Parkinson. Although Páriz correctly described all four cardinal signs, it was only published in Hungarian and was not widely distributed.[237][238]
In 1912, Frederic Lewy described microscopic particles in affected brains, later named Lewy bodies.[239] In 1919, Konstantin Tretiakoff reported that the substantia nigra was the main brain structure affected, corroborated by Rolf Hassler in 1938.[240] The underlying changes in dopamine signaling were identified in the 1950s, largely by Arvid Carlsson and Oleh Hornykiewicz.[241] In 1997, Polymeropoulos and colleagues at the NIH discovered the first gene for PD,[68] SNCA, which encodes alpha-synuclein. Alpha-synuclein was in turn found to be the main component of Lewy bodies by Spillantini, Trojanowski, Goedert, and others.[242] Anticholinergics and surgery were the only treatments until the use of levodopa,[243][244] which, although first synthesized by Casimir Funk in 1911,[245] did not enter clinical use until 1967.[246] By the late 1980s deep brain stimulation introduced by Alim Louis Benabid and colleagues at Grenoble, France, emerged as an additional treatment.[247]
Society and culture
[edit]Social impact
[edit]For some people with PD, masked facial expressions and difficulty moderating facial expressions of emotion or recognizing other people's facial expressions can impact social well-being.[248] As the condition progresses, tremor, other motor symptoms, difficulty communicating, or issues with mobility may interfere with social engagement, causing individuals with PD to feel isolated.[249] Public perception and awareness of PD symptoms such as shaking, hallucinating, slurring speech, and being off balance is lacking in some countries and can lead to stigma.[249]
Cost
[edit]Parts of this article (those related to this subsection) need to be updated. (August 2020) |
The costs of PD to society are high; in 2007, the largest share of direct cost came from inpatient care and nursing homes, while the share coming from medication was substantially lower.[250] Indirect costs are high, due to reduced productivity and the burden on caregivers.[250] In addition to economic costs, PD reduces quality of life of those with the disease and their caregivers.[250]
A study based on 2017 data estimated the US economic PD burden at $51.9 billion, including direct medical costs of $25.4 billion and $26.5 billion in indirect and non-medical costs. The projected total economic burden surpasses $79 billion by 2037. These findings highlight the need for interventions to reduce PD incidence, delay disease progression, and alleviate symptom burden that may reduce the future economic burden of PD.[251]
Advocacy
[edit]
The birthday of James Parkinson, 11 April, has been designated as World Parkinson's Day.[252] A red tulip was chosen by international organizations as the symbol of the disease in 2005; it represents the 'James Parkinson' tulip cultivar, registered in 1981 by a Dutch horticulturalist.[253]
Advocacy organizations include the National Parkinson Foundation, which has provided more than $180 million in care, research, and support services since 1982,[254] Parkinson's Disease Foundation, which has distributed more than $115 million for research and nearly $50 million for education and advocacy programs since its founding in 1957 by William Black;[255][256] the American Parkinson Disease Association, founded in 1961;[257] and the European Parkinson's Disease Association, founded in 1992.[258]
Notable cases
[edit]
In the 21st century, the diagnosis of Parkinson's among notable figures has increased the public's understanding of the disorder.[259] Actor Michael J. Fox was diagnosed with PD at 29 years old,[260] and has used his diagnosis to increase awareness of the disease.[261] To illustrate the effects of the disease, Fox has appeared without medication in television roles and before the United States Congress without medication.[262] The Michael J. Fox Foundation, which he founded in 2000, has raised over $2 billion for Parkinson's research.[263]
Boxer Muhammad Ali showed signs of PD when he was 38, but was undiagnosed until he was 42, and has been called the "world's most famous Parkinson's patient".[264] Whether he had PD or parkinsonism related to boxing is unresolved.[265][266] Cyclist and Olympic medalist Davis Phinney, diagnosed with Parkinson's at 40, started the Davis Phinney Foundation in 2004 to support PD research.[267][268]
Several historical figures have been theorized to have had Parkinson's, often framed in the industriousness and inflexibility of the so-called "Parkinsonian personality".[269][270] For instance, English philosopher Thomas Hobbes was diagnosed with "shaking palsy"—assumed to have been Parkinson's—but continued writing works such as Leviathan.[271][272][273] Adolf Hitler is widely believed to have had Parkinson's, and the condition may have influenced his decision making.[274][275][276] Mao Zedong was also reported to have died from the disorder.[277]
Clinical research
[edit]Parts of this article (those related to this subsection) need to be updated. (July 2020) |

As of 2022[update], no disease-modifying drugs (drugs that target the causes or damage) are approved for Parkinson's, so this is a major focus of Parkinson's research.[278][279] Active research directions include the search for new animal models of the disease and studies of the potential usefulness of gene therapy, stem cell transplants, and neuroprotective agents.[280] To aid in earlier diagnosis, research criteria for identifying prodromal biomarkers of the disease have been established.[281]
Gene therapy
[edit]Gene therapy typically involves the use of a noninfectious virus[282] to shuttle genetic material into a part of the brain. Approaches have involved the expression of growth factors to prevent damage (Neurturin – a GDNF-family growth factor), and enzymes such as glutamic acid decarboxylase (GAD – the enzyme that produces GABA), tyrosine hydroxylase (the enzyme that produces L-DOPA) and catechol-O-methyl transferase (COMT metabolizes levodopa to 3-O-methyldopa). No safety concerns have been reported but the approaches have largely failed in phase two clinical trials.[280] The delivery of GAD showed promise in phase two trials in 2011, but while effective at improving motor function, was inferior to DBS. Follow-up studies in the same cohort have suggested persistent improvement.[283]
Neuroprotective treatments
[edit]A vaccine that primes the human immune system to destroy alpha-synuclein, PD01A, entered clinical trials and a phase one report in 2020 suggested safety and tolerability.[284][285] In 2018, an antibody, PRX002/RG7935, showed preliminary safety evidence in stage I trials supporting continuation to stage II trials.[286]
Cell-based therapies
[edit]In contrast to other neurodegenerative disorders, many Parkinson's symptoms can be attributed to the loss of a single cell type: mesencephalic dopaminergic (DA) neurons. Consequently, DA neuron regeneration is a promising therapeutic approach.[287] Although most initial research sought to generate DA neuron precursor cells from fetal brain tissue,[288] pluripotent stem cells—particularly induced pluripotent stem cells (iPSCs)—have become an increasingly popular tissue source.[289][290]
Both fetal and iPSC-derived DA neurons have been transplanted into patients in clinical trials.[291][292]: 1926 Although some patients see improvements, the results are highly variable. Adverse effects, such as dyskinesia arising from excess dopamine release by the transplanted tissues, have also been observed.[293][294]
Pharmaceutical
[edit]Antagonists of adenosine receptors (specifically A2A) have been explored for Parkinson's.[295] Of these, istradefylline has emerged as the most successful medication and was approved for medical use in the United States in 2019.[296] It is approved as an add-on treatment to the levodopa/carbidopa regime.[296] LRRK2 kinase inhibitors are also of interest.[297]
Pathophysiology
[edit]Neurodegeneration is proposed to originate in the brainstem and olfactory bulb.[298]
Notes and references
[edit]Notes
[edit]Citations
[edit]- ^ a b c "Parkinson's Disease Information Page". NINDS. 30 June 2016. Retrieved 18 July 2016.
- ^ Truong & Bhidayasiri 2016, p. 188.
- ^ Ferri 2010, Chapter P.
- ^ Koh J, Ito H (January 2017). "Differential diagnosis of Parkinson's disease and other neurodegenerative disorders". Nihon Rinsho. Japanese Journal of Clinical Medicine. 75 (1): 56–62. PMID 30566295.
- ^ Sveinbjornsdottir S (October 2016). "The clinical symptoms of Parkinson's disease". Journal of Neurochemistry. 139 (Suppl 1): 318–324. doi:10.1111/jnc.13691. PMID 27401947.
- ^ Ou Z, Pan J, Tang S, Duan D, Yu D, Nong H, et al. (7 December 2021). "Global Trends in the Incidence, Prevalence, and Years Lived With Disability of Parkinson's Disease in 204 Countries/Territories From 1990 to 2019". Frontiers in Public Health. 9: 776847. doi:10.3389/fpubh.2021.776847. PMC 8688697. PMID 34950630.
- ^ Ramesh & Arachchige 2023, pp. 200–201, 203.
- ^ Calabresi et al. 2023, pp. 1, 5.
- ^ National Institute of Neurological Disorders and Stroke.
- ^ Wallace et al. 2021, p. 149.
- ^ Hansen et al. 2019, p. 635.
- ^ Bhattacharyya 2017, p. 7.
- ^ Stanford University School Medicine.
- ^ Bologna, Truong & Jankovic 2022, pp. 1–6.
- ^ Limphaibool et al. 2019, pp. 1–2.
- ^ Leta et al. 2022, p. 1122.
- ^ Langston 2017, p. S11.
- ^ Prajjwal et al. 2024, pp. 1–3.
- ^ Olfatia, Shoeibia & Litvanb 2019, p. 101.
- ^ Dolgacheva, Zinchenko & Goncharov 2022, p. 2.
- ^ Connie T, Aderinola TB, Ong TS, Goh MKO, Erfianto B, Purnama B (12 December 2022). "Pose-Based Gait Analysis for Diagnosis of Parkinson's Disease". Algorithms. 15 (12). MDPI AG: 474. doi:10.3390/a15120474.
- ^ a b "Parkinson's disease - Symptoms". National Health Service. 3 November 2022. Retrieved 28 April 2024.
- ^ Leite Silva AB, Gonçalves de Oliveira RW, Diógenes GP, de Castro Aguiar MF, Sallem CC, Lima MP, et al. (February 2023). "Premotor, nonmotor and motor symptoms of Parkinson's Disease: A new clinical state of the art". Ageing Research Reviews. 84: 101834. doi:10.1016/j.arr.2022.101834. PMID 36581178.
- ^ De Carolis L, Galli S, Bianchini E, Rinaldi D, Raju M, Caliò B, et al. (January 2023). "Age at Onset Influences Progression of Motor and Non-Motor Symptoms during the Early Stage of Parkinson's Disease: A Monocentric Retrospective Study". Brain Sciences. 13 (2): 157. doi:10.3390/brainsci13020157. PMC 9954489. PMID 36831700.
- ^ a b Abusrair AH, Elsekaily W, Bohlega S (13 September 2022). "Tremor in Parkinson's Disease: From Pathophysiology to Advanced Therapies". Tremor and Other Hyperkinetic Movements. 12 (1): 29. doi:10.5334/tohm.712. PMC 9504742. PMID 36211804.
- ^ "Tremor". Parkinson's Foundation. Retrieved 28 April 2024.
- ^ Bologna M, Paparella G, Fasano A, Hallett M, Berardelli A (March 2020). "Evolving concepts on bradykinesia". Brain. 143 (3): 727–750. doi:10.1093/brain/awz344. PMC 8205506. PMID 31834375.
- ^ "What Is Bradykinesia?". Cleveland Clinic. 30 November 2023. Retrieved 2 May 2024.
- ^ "Facial Masking". Parkinson's Foundation. Retrieved 28 April 2024.
- ^ Ferreira-Sánchez MD, Moreno-Verdú M, Cano-de-la-Cuerda R (February 2020). "Quantitative Measurement of Rigidity in Parkinson´s Disease: A Systematic Review". Sensors. 20 (3): 880. Bibcode:2020Senso..20..880F. doi:10.3390/s20030880. PMC 7038663. PMID 32041374.
- ^ "Rigidity". Parkinson's Foundation. Retrieved 28 April 2024.
- ^ Asci F, Falletti M, Zampogna A, Patera M, Hallett M, Rothwell J, et al. (September 2023). "Rigidity in Parkinson's disease: evidence from biomechanical and neurophysiological measures". Brain. 146 (9): 3705–3718. doi:10.1093/brain/awad114. PMC 10681667. PMID 37018058.
- ^ Becker D, Maric A, Schreiner SJ, Büchele F, Baumann CR, Waldvogel D (2 December 2022). Ahmed S (ed.). "Onset of Postural Instability in Parkinson's Disease Depends on Age rather than Disease Duration". Parkinson's Disease. 2022: 6233835. doi:10.1155/2022/6233835. PMC 9734006. PMID 36506486.
- ^ "Postural Instability (Balance & Falls)". Parkinson's Foundation. Retrieved 29 April 2024.
- ^ Eklund M, Nuuttila S, Joutsa J, Jaakkola E, Mäkinen E, Honkanen EA, et al. (July 2022). "Diagnostic value of micrographia in Parkinson's disease: a study with [123I]FP-CIT SPECT". Journal of Neural Transmission. 129 (7): 895–904. doi:10.1007/s00702-022-02517-1. PMC 9217822. PMID 35624405.
- ^ a b Corrà MF, Vila-Chã N, Sardoeira A, Hansen C, Sousa AP, Reis I, et al. (January 2023). "Peripheral neuropathy in Parkinson's disease: prevalence and functional impact on gait and balance". Brain. 146 (1): 225–236. doi:10.1093/brain/awac026. PMC 9825570. PMID 35088837.
- ^ França M, Parada Lima J, Oliveira A, Rosas MJ, Vicente SG, Sousa C (September 2023). "Visuospatial memory profile of patients with Parkinson's disease". Applied Neuropsychology. Adult: 1–9. doi:10.1080/23279095.2023.2256918. hdl:10216/141606. PMID 37695259.
- ^ a b Palma JA, Kaufmann H (March 2018). "Treatment of autonomic dysfunction in Parkinson disease and other synucleinopathies". Movement Disorders. 33 (3): 372–390. doi:10.1002/mds.27344. PMC 5844369. PMID 29508455.
- ^ Winiker K, Kertscher B (March 2023). "Behavioural interventions for swallowing in subjects with Parkinson's disease: A mixed methods systematic review". International Journal of Language & Communication Disorders. 58 (4): 1375–1404. doi:10.1111/1460-6984.12865. PMID 36951546.
- ^ Warnecke T, Schäfer KH, Claus I, Del Tredici K, Jost WH (March 2022). "Gastrointestinal involvement in Parkinson's disease: pathophysiology, diagnosis, and management". npj Parkinson's Disease. 8 (1): 31. doi:10.1038/s41531-022-00295-x. PMC 8948218. PMID 35332158.
- ^ Han MN, Finkelstein DI, McQuade RM, Diwakarla S (January 2022). "Gastrointestinal Dysfunction in Parkinson's Disease: Current and Potential Therapeutics". Journal of Personalized Medicine. 12 (2): 144. doi:10.3390/jpm12020144. PMC 8875119. PMID 35207632.
- ^ Skjærbæk C, Knudsen K, Horsager J, Borghammer P (January 2021). "Gastrointestinal Dysfunction in Parkinson's Disease". Journal of Clinical Medicine. 10 (3): 493. doi:10.3390/jcm10030493. PMC 7866791. PMID 33572547.
- ^ Palma JA, Kaufmann H (February 2020). "Orthostatic Hypotension in Parkinson Disease". Clinics in Geriatric Medicine. 36 (1): 53–67. doi:10.1016/j.cger.2019.09.002. PMC 7029426. PMID 31733702.
- ^ a b Hinkle JT, Perepezko K, Gonzalez LL, Mills KA, Pontone GM (January 2021). "Apathy and Anxiety in De Novo Parkinson's Disease Predict the Severity of Motor Complications". Movement Disorders Clinical Practice. 8 (1): 76–84. doi:10.1002/mdc3.13117. PMC 7780944. PMID 33426161.
- ^ a b c d e Macías-García P, Rashid-López R, Cruz-Gómez ÁJ, Lozano-Soto E, Sanmartino F, Espinosa-Rosso R, et al. (9 May 2022). Aasly J (ed.). "Neuropsychiatric Symptoms in Clinically Defined Parkinson's Disease: An Updated Review of Literature". Behavioural Neurology. 2022: 1213393. doi:10.1155/2022/1213393. PMC 9110237. PMID 35586201.
- ^ a b Khatri DK, Choudhary M, Sood A, Singh SB (November 2020). "Anxiety: An ignored aspect of Parkinson's disease lacking attention". Biomedicine & Pharmacotherapy. 131: 110776. doi:10.1016/j.biopha.2020.110776. PMID 33152935.
- ^ Weintraub D, Mamikonyan E (September 2019). "The Neuropsychiatry of Parkinson Disease: A Perfect Storm". The American Journal of Geriatric Psychiatry. 27 (9): 998–1018. doi:10.1016/j.jagp.2019.03.002. PMC 7015280. PMID 31006550.
- ^ Chendo I, Silva C, Duarte GS, Prada L, Voon V, Ferreira JJ (21 January 2022). "Frequency and Characteristics of Psychosis in Parkinson's Disease: A Systematic Review and Meta-Analysis". Journal of Parkinson's Disease. 12 (1): 85–94. doi:10.3233/JPD-212930. PMID 34806620.
- ^ Zhang S, Ma Y (September 2022). "Emerging role of psychosis in Parkinson's disease: From clinical relevance to molecular mechanisms". World Journal of Psychiatry. 12 (9): 1127–1140. doi:10.5498/wjp.v12.i9.1127. PMC 9521528. PMID 36186499.
- ^ Pahwa R, Isaacson SH, Small GW, Torres-Yaghi Y, Pagan F, Sabbagh M (December 2022). "Screening, Diagnosis, and Management of Parkinson's Disease Psychosis: Recommendations From an Expert Panel". Neurology and Therapy. 11 (4): 1571–1582. doi:10.1007/s40120-022-00388-y. PMC 9362468. PMID 35906500.
- ^ De Wit LE, Wilting I, Souverein PC, van der Pol P, Egberts TC (May 2022). "Impulse control disorders associated with dopaminergic drugs: A disproportionality analysis using vigibase". European Neuropsychopharmacology. 58: 30–38. doi:10.1016/j.euroneuro.2022.01.113. PMID 35189453.
- ^ Gonzalez-Latapi P, Bayram E, Litvan I, Marras C (May 2021). "Cognitive Impairment in Parkinson's Disease: Epidemiology, Clinical Profile, Protective and Risk Factors". Behavioral Sciences. 11 (5): 74. doi:10.3390/bs11050074. PMC 8152515. PMID 34068064.
- ^ "Parkinson's Disease Sleep Problems". Cleveland Clinic. Retrieved 1 May 2024.
- ^ Bollu PC, Sahota P (2017). "Sleep and Parkinson Disease". Missouri Medicine. 114 (5): 381–386. PMC 6140184. PMID 30228640.
- ^ Dodet P, Houot M, Leu-Semenescu S, Corvol JC, Lehéricy S, Mangone G, et al. (February 2024). "Sleep disorders in Parkinson's disease, an early and multiple problem". npj Parkinson's Disease. 10 (1): 46. doi:10.1038/s41531-024-00642-0. PMC 10904863. PMID 38424131.
- ^ Niemann N, Billnitzer A, Jankovic J (January 2021). "Parkinson's disease and skin". Parkinsonism & Related Disorders. 82: 61–76. doi:10.1016/j.parkreldis.2020.11.017. PMID 33248395.
- ^ Almikhlafi MA (January 2024). "A review of the gastrointestinal, olfactory, and skin abnormalities in patients with Parkinson's disease". Neurosciences. 29 (1): 4–9. doi:10.17712/nsj.2024.1.20230062 (inactive 1 November 2024). PMC 10827020. PMID 38195133.
{{cite journal}}: CS1 maint: DOI inactive as of November 2024 (link) - ^ Vertes AC, Beato MR, Sonne J, Khan Suheb MZ (June 2023). "Parkinson-Plus Syndrome". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 36256760. Retrieved 2 May 2024.
- ^ a b c Morris HR, Spillantini MG, Sue CM, Williams-Gray CH (January 2024). "The pathogenesis of Parkinson's disease". Lancet. 403 (10423): 293–304. doi:10.1016/s0140-6736(23)01478-2. PMID 38245249.
- ^ Coleman C, Martin I (16 December 2022). "Unraveling Parkinson's Disease Neurodegeneration: Does Aging Hold the Clues?". Journal of Parkinson's Disease. 12 (8): 2321–2338. doi:10.3233/JPD-223363. PMC 9837701. PMID 36278358.
- ^ Jaaffar FS, Aizuddin AN, Ahmad N (21 February 2024). "Environmental Risk Factors of Parkinson's Disease: A Scoping Review". International Journal of Public Health Research. 14 (1): 1823–1831. doi:10.17576/ijphr/1401.2024.10.
- ^ a b c De Miranda BR, Goldman SM, Miller GW, Greenamyre JT, Dorsey ER (2022). "Preventing Parkinson's Disease: An Environmental Agenda". Journal of Parkinson's Disease. 12 (1): 45–68. doi:10.3233/JPD-212922. PMC 8842749. PMID 34719434. S2CID 240235393.
- ^ Zhao Y, Yunjia L, Hilde K (23 April 2024). "Association of Coffee Consumption and Prediagnostic Caffeine Metabolites With Incident Parkinson Disease in a Population-Based Cohort". Neurology. 102 (8): e209201. doi:10.1212/WNL.0000000000209201. PMC 11175631. PMID 38513162.
- ^ Rose, Schwarzschild & Gomperts 2024.
- ^ a b Salles PA, Tirapegui JM, Chaná-Cuevas P (22 March 2024). "Genetics of Parkinson's disease: Dominant forms and GBA". Neurology Perspectives. 4 (3): 100153. doi:10.1016/j.neurop.2024.100153.
- ^ Khani M, Cerquera-Cleves C, Kekenadze M, Wild Crea P, Singleton AB, Bandres-Ciga S (May 2024). "Towards a Global View of Parkinson's Disease Genetics". Annals of Neurology. 95 (5): 831–842. doi:10.1002/ana.26905. PMC 11060911. PMID 38557965.
- ^ Zhang Y, Wu X, Johnson E, National Institutes of Health (October 2024). "Whole-genome sequencing reveals novel variants in Parkinson's disease-related genes". Neurogenetics Research. 34 (7): 501–510. doi:10.1038/s41531-024-00659-5. PMC 10899198. PMID 38413607.
- ^ a b Polymeropoulos MH, Lavedan C, Leroy E, Ide SE, Dehejia A, Dutra A, et al. (27 June 1997). "Mutation in the α-Synuclein Gene Identified in Families with Parkinson's Disease". Science. 276 (5321): 2045–2047. doi:10.1126/science.276.5321.2045. ISSN 0036-8075. PMID 9197268.
- ^ a b c d e f Tanner CM, Ostrem JL (August 2024). "Parkinson's Disease". New England Journal of Medicine. 391 (5): 442–452. doi:10.1056/NEJMra2401857. PMID 39083773.
- ^ Smith L, Schapira AH (April 2022). "GBA Variants and Parkinson Disease: Mechanisms and Treatments". Cells. 11 (8): 1261. doi:10.3390/cells11081261. PMC 9029385. PMID 35455941.
- ^ Lashuel HA (July 2020). "Do Lewy bodies contain alpha-synuclein fibrils? and Does it matter? A brief history and critical analysis of recent reports". Neurobiology of Disease. 141: 104876. doi:10.1016/j.nbd.2020.104876. PMID 32339655.
- ^ a b Abugable AA, Morris JL, Palminha NM, Zaksauskaite R, Ray S, El-Khamisy SF (September 2019). "DNA repair and neurological disease: From molecular understanding to the development of diagnostics and model organisms". DNA Repair. 81: 102669. doi:10.1016/j.dnarep.2019.102669. PMID 31331820.
- ^ Santos-Lobato BL (April 2024). "Towards a methodological uniformization of environmental risk studies in Parkinson's disease". npj Parkinson's Disease. 10 (1): 86. doi:10.1038/s41531-024-00709-y. PMC 11024193. PMID 38632283.
- ^ Bloem BR, Boonstra TA (December 2023). "The inadequacy of current pesticide regulations for protecting brain health: the case of glyphosate and Parkinson's disease". The Lancet. Planetary Health. 7 (12): e948–e949. doi:10.1016/s2542-5196(23)00255-3. PMID 37949088.
- ^ Torrey EF, Simmons W (16 September 2023). "Mercury and Parkinson's Disease: Promising Leads, but Research Is Needed". Parkinson's Disease. 2023: 4709322. doi:10.1155/2023/4709322. PMC 10517869. PMID 37744289.
- ^ Zhao Y, Ray A, Portengen L, Vermeulen R, Peters S (July 2023). "Metal Exposure and Risk of Parkinson Disease: A Systematic Review and Meta-Analysis". American Journal of Epidemiology. 192 (7): 1207–1223. doi:10.1093/aje/kwad082. PMC 10326611. PMID 37022311.
- ^ Dorsey ER, Zafar M, Lettenberger SE, Pawlik ME, Kinel D, Frissen M, et al. (2023). "Trichloroethylene: An Invisible Cause of Parkinson's Disease?". Journal of Parkinson's Disease. 13 (2): 203–218. doi:10.3233/JPD-225047. PMC 10041423. PMID 36938742.
- ^ Kaya I, Nilsson A, Luptáková D, He Y, Vallianatou T, Bjärterot P, et al. (July 2023). "Spatial lipidomics reveals brain region-specific changes of sulfatides in an experimental MPTP Parkinson's disease primate model". npj Parkinson's Disease. 9 (1): 118. doi:10.1038/s41531-023-00558-1. PMC 10372136. PMID 37495571.
- ^ Delic V, Beck KD, Pang KC, Citron BA (April 2020). "Biological links between traumatic brain injury and Parkinson's disease". Acta Neuropathologica Communications. 8 (1): 45. doi:10.1186/s40478-020-00924-7. PMC 7137235. PMID 32264976.
- ^ Koros C, Simitsi AM, Bougea A, Papagiannakis N, Antonelou R, Pachi I, et al. (July 2023). "Double Trouble: Association of Malignant Melanoma with Sporadic and Genetic Forms of Parkinson's Disease and Asymptomatic Carriers of Related Genes: A Brief Report". Medicina. 59 (8): 1360. doi:10.3390/medicina59081360. PMC 10456316. PMID 37629650.
- ^ Fazlollahi A, Zahmatyar M, Alizadeh H, Noori M, Jafari N, Nejadghaderi SA, et al. (October 2022). "Association between gout and the development of Parkinson's disease: a systematic review and meta-analysis". BMC Neurology. 22 (1): 383. doi:10.1186/s12883-022-02874-0. PMC 9552480. PMID 36221048.
- ^ Nyholm D, Hellström PM (2 February 2021). "Effects of Helicobacter pylori on Levodopa Pharmacokinetics". Journal of Parkinson's Disease. 11 (1): 61–69. doi:10.3233/JPD-202298. PMC 7990449. PMID 33164946.
- ^ Zhou ZD, Yi LX, Wang DQ, Lim TM, Tan EK (September 2023). "Role of dopamine in the pathophysiology of Parkinson's disease". Translational Neurodegeneration. 12 (1): 44. doi:10.1186/s40035-023-00378-6. PMC 10506345. PMID 37718439.
- ^ a b c Rocha GS, Freire MA, Britto AM, Paiva KM, Oliveira RF, Fonseca IA, et al. (August 2023). "Basal ganglia for beginners: the basic concepts you need to know and their role in movement control". Frontiers in Systems Neuroscience. 17: 1242929. doi:10.3389/fnsys.2023.1242929. PMC 10435282. PMID 37600831.
- ^ Young CB, Reddy V, Sonne J (July 2023). "Neuroanatomy, Basal Ganglia". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 30725826. Retrieved 21 May 2024.
- ^ Bingham CS, Petersen MV, Parent M, McIntyre CC (March 2023). "Evolving characterization of the human hyperdirect pathway". Brain Structure & Function. 228 (2): 353–365. doi:10.1007/s00429-023-02610-5. PMC 10716731. PMID 36708394.
- ^ Ramesh & Arachchige 2023.
- ^ Dong-Chen X, Yong C, Yang X, Chen-Yu S, Li-Hua P (February 2023). "Signaling pathways in Parkinson's disease: molecular mechanisms and therapeutic interventions". Signal Transduction and Targeted Therapy. 8 (1): 1–18. doi:10.1038/s41392-023-01353-3. ISSN 2059-3635. PMC 9944326. PMID 36810524.
- ^ Chen R, Gu X, Wang X (April 2022). "α-Synuclein in Parkinson's disease and advances in detection". Clinica Chimica Acta; International Journal of Clinical Chemistry. 529: 76–86. doi:10.1016/j.cca.2022.02.006. PMID 35176268.
- ^ Menšíková K, Matěj R, Colosimo C, Rosales R, Tučková L, Ehrmann J, et al. (January 2022). "Lewy body disease or diseases with Lewy bodies?". npj Parkinson's Disease. 8 (1): 1–11. doi:10.1038/s41531-021-00273-9. ISSN 2373-8057. PMC 8748648. PMID 35013341.
- ^ Zamanian MY, Parra RM, Soltani A, Kujawska M, Mustafa YF, Raheem G, et al. (June 2023). "Targeting Nrf2 signaling pathway and oxidative stress by resveratrol for Parkinson's disease: an overview and update on new developments". Molecular Biology Reports. 50 (6): 5455–5464. doi:10.1007/s11033-023-08409-1. PMID 37155008.
- ^ Chakrabarti S, Bisaglia M (April 2023). "Oxidative Stress and Neuroinflammation in Parkinson's Disease: The Role of Dopamine Oxidation Products". Antioxidants. 12 (4): 955. doi:10.3390/antiox12040955. PMC 10135711. PMID 37107329.
- ^ Cardozo C (September 2023). "Editor's evaluation: Lipid hydroperoxides promote sarcopenia through carbonyl stress". Ageing Research Reviews. doi:10.7554/elife.85289.sa0.
- ^ Obeso JA, Rodriguez-Oroz MC, Goetz CG, Marin C, Kordower JH, Rodriguez M, et al. (June 2010). "Missing pieces in the Parkinson's disease puzzle". Nature Medicine. 16 (6): 653–661. doi:10.1038/nm.2165. PMID 20495568. S2CID 3146438.
- ^ Hirsch EC (December 2009). "Iron transport in Parkinson's disease". Parkinsonism & Related Disorders. 15 (Suppl 3): S209–S211. doi:10.1016/S1353-8020(09)70816-8. PMID 20082992.
- ^ Li X, Sundquist J, Sundquist K (23 December 2011). "Subsequent risks of Parkinson disease in patients with autoimmune and related disorders: a nationwide epidemiological study from Sweden". Neuro-Degenerative Diseases. 10 (1–4): 277–284. doi:10.1159/000333222. PMID 22205172. S2CID 39874367.
- ^ Lai SW, Lin CH, Lin HF, Lin CL, Lin CC, Liao KF (February 2017). "Herpes zoster correlates with increased risk of Parkinson's disease in older people: A population-based cohort study in Taiwan". Medicine. 96 (7): e6075. doi:10.1097/MD.0000000000006075. PMC 5319504. PMID 28207515.
- ^ Tan EK, Chao YX, West A, Chan LL, Poewe W, Jankovic J (June 2020). "Parkinson disease and the immune system - associations, mechanisms and therapeutics". Nature Reviews. Neurology. 16 (6): 303–318. doi:10.1038/s41582-020-0344-4. PMID 32332985. S2CID 216111568.
- ^ Raj T, Rothamel K, Mostafavi S, Ye C, Lee MN, Replogle JM, et al. (May 2014). "Polarization of the effects of autoimmune and neurodegenerative risk alleles in leukocytes". Science. 344 (6183): 519–523. Bibcode:2014Sci...344..519R. doi:10.1126/science.1249547. PMC 4910825. PMID 24786080.
- ^ a b Du G, Dong W, Yang Q, Yu X, Ma J, Gu W, et al. (2020). "Altered Gut Microbiota Related to Inflammatory Responses in Patients With Huntington's Disease". Frontiers in Immunology. 11: 603594. doi:10.3389/fimmu.2020.603594. PMC 7933529. PMID 33679692.
- ^ a b Gamborg M, Hvid LG, Dalgas U, Langeskov-Christensen M (3 October 2021). "Review for "Parkinson's disease and intensive exercise therapy — An updated systematic review and meta-analysis"". Acta Neurologica Scandinavica. doi:10.1111/ane.13579/v1/review2.
- ^ [non-primary source needed]Kim S, Kwon SH, Kam TI, Panicker N, Karuppagounder SS, Lee S, et al. (August 2019). "Transneuronal Propagation of Pathologic α-Synuclein from the Gut to the Brain Models Parkinson's Disease". Neuron. 103 (4): 627–641.e7. doi:10.1016/j.neuron.2019.05.035. PMC 6706297. PMID 31255487.
- ^ a b c Jankovic J (April 2008). "Parkinson's disease: clinical features and diagnosis". Journal of Neurology, Neurosurgery, and Psychiatry. 79 (4): 368–376. doi:10.1136/jnnp.2007.131045. PMID 18344392. Archived from the original on 19 August 2015.
- ^ a b The National Collaborating Centre for Chronic Conditions, ed. (2006). "Diagnosing Parkinson's Disease". Parkinson's Disease. London: Royal College of Physicians. pp. 29–47. ISBN 978-1-8601-6283-1. Archived from the original on 24 September 2010.
- ^ a b c d e f g h i Armstrong MJ, Okun MS (February 2020). "Diagnosis and Treatment of Parkinson Disease: A Review". JAMA. 323 (6): 548–560. doi:10.1001/jama.2019.22360. PMID 32044947. S2CID 211079287.
- ^ Poewe W, Wenning G (November 2002). "The differential diagnosis of Parkinson's disease". European Journal of Neurology. 9 (Suppl 3): 23–30. doi:10.1046/j.1468-1331.9.s3.3.x. PMID 12464118.
- ^ Gibb WR, Lees AJ (June 1988). "The relevance of the Lewy body to the pathogenesis of idiopathic Parkinson's disease". Journal of Neurology, Neurosurgery, and Psychiatry. 51 (6): 745–752. doi:10.1136/jnnp.51.6.745. PMC 1033142. PMID 2841426.
- ^ Mustafa HI, Fessel JP, Barwise J, Shannon JR, Raj SR, Diedrich A, et al. (January 2012). "Dysautonomia: perioperative implications". Anesthesiology. 116 (1): 205–215. doi:10.1097/ALN.0b013e31823db712. PMC 3296831. PMID 22143168.
- ^ Rizzo G, Copetti M, Arcuti S, Martino D, Fontana A, Logroscino G (February 2016). "Accuracy of clinical diagnosis of Parkinson disease: A systematic review and meta-analysis". Neurology. 86 (6): 566–576. doi:10.1212/WNL.0000000000002350. PMID 26764028. S2CID 207110404.
- ^ a b c d Brooks DJ (April 2010). "Imaging approaches to Parkinson disease". Journal of Nuclear Medicine. 51 (4): 596–609. doi:10.2967/jnumed.108.059998. PMID 20351351.
- ^ Schwarz ST, Afzal M, Morgan PS, Bajaj N, Gowland PA, Auer DP (2014). "The 'swallow tail' appearance of the healthy nigrosome - a new accurate test of Parkinson's disease: a case-control and retrospective cross-sectional MRI study at 3T". PLOS ONE. 9 (4): e93814. Bibcode:2014PLoSO...993814S. doi:10.1371/journal.pone.0093814. PMC 3977922. PMID 24710392.
- ^ Mahlknecht P, Krismer F, Poewe W, Seppi K (April 2017). "Meta-analysis of dorsolateral nigral hyperintensity on magnetic resonance imaging as a marker for Parkinson's disease". Movement Disorders. 32 (4): 619–623. doi:10.1002/mds.26932. PMID 28151553. S2CID 7730034.
- ^ Cho SJ, Bae YJ, Kim JM, Kim D, Baik SH, Sunwoo L, et al. (March 2021). "Diagnostic performance of neuromelanin-sensitive magnetic resonance imaging for patients with Parkinson's disease and factor analysis for its heterogeneity: a systematic review and meta-analysis". European Radiology. 31 (3): 1268–1280. doi:10.1007/s00330-020-07240-7. PMID 32886201. S2CID 221478854.
- ^ Boonstra JT, Michielse S, Temel Y, Hoogland G, Jahanshahi A (February 2021). "Neuroimaging Detectable Differences between Parkinson's Disease Motor Subtypes: A Systematic Review". Movement Disorders Clinical Practice. 8 (2): 175–192. doi:10.1002/mdc3.13107. PMC 7853198. PMID 33553487.
- ^ Suwijn SR, van Boheemen CJ, de Haan RJ, Tissingh G, Booij J, de Bie RM (2015). "The diagnostic accuracy of dopamine transporter SPECT imaging to detect nigrostriatal cell loss in patients with Parkinson's disease or clinically uncertain parkinsonism: a systematic review". EJNMMI Research. 5: 12. doi:10.1186/s13550-015-0087-1. PMC 4385258. PMID 25853018.
- ^ "DaTSCAN Approval Letter" (PDF). FDA.gov. Food and Drug Administration. Retrieved 22 March 2019.
- ^ a b c d Greenland & Barker 2018.
- ^ McCann H, Stevens CH, Cartwright H, Halliday GM (January 2014). "α-Synucleinopathy phenotypes". Parkinsonism & Related Disorders. 20 (Suppl 1): S62–S67. doi:10.1016/S1353-8020(13)70017-8. hdl:1959.4/53593. PMID 24262191.
- ^ Ganguly J, Jog M (5 November 2020). "Tauopathy and Movement Disorders-Unveiling the Chameleons and Mimics". Frontiers in Neurology. 11: 599384. doi:10.3389/fneur.2020.599384. PMC 7674803. PMID 33250855.
- ^ Gupta D, Kuruvilla A (December 2011). "Vascular parkinsonism: what makes it different?". Postgraduate Medical Journal. 87 (1034): 829–836. doi:10.1136/postgradmedj-2011-130051. PMID 22121251. S2CID 29227069.
- ^ Miguel-Puga A, Villafuerte G, Salas-Pacheco J, Arias-Carrión O (22 September 2017). "Therapeutic Interventions for Vascular Parkinsonism: A Systematic Review and Meta-analysis". Frontiers in Neurology. 8: 481. doi:10.3389/fneur.2017.00481. PMC 5614922. PMID 29018399.
- ^ Levin J, Kurz A, Arzberger T, Giese A, Höglinger GU (February 2016). "The Differential Diagnosis and Treatment of Atypical Parkinsonism". Deutsches Ärzteblatt International. 113 (5): 61–69. doi:10.3238/arztebl.2016.0061. PMC 4782269. PMID 26900156.
- ^ a b c Simon, Greenberg & Aminoff 2017, p. page number needed.
- ^ a b Crotty & Schwarzschild 2020, p. 1.
- ^ Fabbri et al. 2024, p. 2.
- ^ Rose, Schwarzschild & Gomperts 2024, p. 1267.
- ^ Crotty & Schwarzschild 2020, pp. 1–2.
- ^ Crotty & Schwarzschild 2020, pp. 4.
- ^ Ascherio & Schwarzschild 2016, p. 1262.
- ^ Grotewolda & Albina 2024, pp. 1–2.
- ^ a b c Grotewolda & Albina 2024, p. 2.
- ^ Rose, Schwarzschild & Gomperts 2024, pp. 268–269.
- ^ a b Grotewolda & Albina 2024, p. 3.
- ^ Ren & Chen 2020, p. 1.
- ^ Singh, Tripathi & Singh 2021, p. 10.
- ^ Ascherio & Schwarzschild 2016, pp. 1265–1266.
- ^ Lin et al. 2024, p. 1.
- ^ a b Ascherio & Schwarzschild 2016, p. 1263.
- ^ Ascherio & Schwarzschild 2016, p. 1261.
- ^ Kamal et al. 2020, p. 8.
- ^ Connolly BS, Lang AE (30 April 2014). "Pharmacological treatment of Parkinson disease: a review". JAMA. 311 (16): 1670–1683. doi:10.1001/jama.2014.3654. PMID 24756517. S2CID 205058847.
- ^ Olanow CW, Stocchi F, Lang AE (2011). "The non-motor and non-dopaminergic features of PD". Parkinson's Disease: Non-Motor and Non-Dopaminergic Features. Wiley-Blackwell. ISBN 978-1-4051-9185-2. OCLC 743205140.
- ^ a b c d e f g h i j k l m n o p The National Collaborating Centre for Chronic Conditions, ed. (2006). "Symptomatic pharmacological therapy in Parkinson's disease". Parkinson's Disease (Technical report). London: Royal College of Physicians. pp. 59–100. ISBN 978-1-8601-6283-1. Archived from the original on 24 September 2010. Retrieved 14 March 2023.
- ^ Zhang J, Tan LC (2016). "Revisiting the Medical Management of Parkinson's Disease: Levodopa versus Dopamine Agonist". Current Neuropharmacology. 14 (4): 356–363. doi:10.2174/1570159X14666151208114634. PMC 4876591. PMID 26644151.
- ^ Moosa S, Martínez-Fernández R, Elias WJ, Del Alamo M, Eisenberg HM, Fishman PS (September 2019). "The role of high-intensity focused ultrasound as a symptomatic treatment for Parkinson's disease". Movement Disorders. 34 (9): 1243–1251. doi:10.1002/mds.27779. PMID 31291491. S2CID 195879250.
- ^ a b Pedrosa DJ, Timmermann L (2013). "Review: management of Parkinson's disease". Neuropsychiatric Disease and Treatment (Review). 9: 321–340. doi:10.2147/NDT.S32302. PMC 3592512. PMID 23487540.
- ^ The National Collaborating Centre for Chronic Conditions, ed. (2006). "Palliative care in Parkinson's disease". Parkinson's Disease. London: Royal College of Physicians. pp. 147–151. ISBN 978-1-8601-6283-1. Archived from the original on 24 September 2010.
- ^ Orgeta V, McDonald KR, Poliakoff E, Hindle JV, Clare L, Leroi I (February 2020). "Cognitive training interventions for dementia and mild cognitive impairment in Parkinson's disease". The Cochrane Database of Systematic Reviews. 2020 (2): CD011961. doi:10.1002/14651858.cd011961.pub2. PMC 7043362. PMID 32101639.
- ^ Dissanayaka 2021, pp. 139–156.
- ^ a b c d e f g h i "Recommendations Parkinson's disease in adults Guidance NICE". NICE. 2006. Retrieved 16 March 2023.
- ^ Maria N (2017). Levodopa pharmacokinetics – from stomach to brain: A study on patients with Parkinson's disease. Linköping: Linköping University Electronic Press. p. 10. ISBN 978-9-1768-5557-7. OCLC 993068595.
- ^ Oertel WH (13 March 2017). "Recent advances in treating Parkinson's disease". F1000Research (Review). 6: 260. doi:10.12688/f1000research.10100.1. PMC 5357034. PMID 28357055.
- ^ Binde et al. 2018, p. missing.
- ^ Aquino CC, Fox SH (January 2015). "Clinical spectrum of levodopa-induced complications". Movement Disorders. 30 (1): 80–89. doi:10.1002/mds.26125. PMID 25488260. S2CID 22301199.
- ^ Yan Z, Wang W, Tao X, Cheng W, Zuo G, Chen Z, et al. (November 2022). "High-dose versus low-dose inhaled levodopa (CVT-301) in patients with Parkinson disease for the treatment of OFF episodes: a meta-analysis of randomized controlled trials". Neurological Sciences. 43 (11): 6233–6241. doi:10.1007/s10072-022-06298-z. PMID 35907110. S2CID 251162631.
- ^ Paik J (June 2020). "Levodopa Inhalation Powder: A Review in Parkinson's Disease". Drugs. 80 (8): 821–828. doi:10.1007/s40265-020-01307-x. PMID 32319076. S2CID 216033034.
- ^ "Regulatory Decision Summary for Vyalev". Health Canada. 3 May 2023. Retrieved 4 April 2024.
- ^ "Vyalev foslevodopa 2400 mg/10 mL and foscarbidopa 120 mg/10 mL solution for subcutaneous infusion vial (372902)". Therapeutic Goods Administration (TGA). 28 March 2024. Retrieved 4 April 2024.
- ^ a b "U.S. FDA Approves Vyalev (foscarbidopa and foslevodopa) for Adults Living with Advanced Parkinson's Disease". AbbVie (Press release). 17 October 2024. Retrieved 18 October 2024.
- ^ https://www.accessdata.fda.gov/drugsatfda_docs/appletter/2024/216962Orig1s000ltr.pdf
- ^ Tambasco N, Romoli M, Calabresi P (2018). "Levodopa in Parkinson's Disease: Current Status and Future Developments". Current Neuropharmacology. 16 (8): 1239–1252. doi:10.2174/1570159X15666170510143821. PMC 6187751. PMID 28494719.
- ^ a b c Akhtar MJ, Yar MS, Grover G, Nath R (January 2020). "Neurological and psychiatric management using COMT inhibitors: A review". Bioorganic Chemistry. 94: 103418. doi:10.1016/j.bioorg.2019.103418. PMID 31708229.
- ^ "Tasmar 100 mg Tablets – Summary of Product Characteristics (SmPC) – (emc)". www.medicines.org.uk. Archived from the original on 6 August 2020. Retrieved 7 January 2021.
- ^ Scott LJ (September 2016). "Opicapone: A Review in Parkinson's Disease". Drugs. 76 (13): 1293–1300. doi:10.1007/s40265-016-0623-y. PMID 27498199. S2CID 5787752.
- ^ Watkins P (2000). "COMT inhibitors and liver toxicity". Neurology. 55 (11 Suppl 4): S51–52, discussion S53–56. PMID 11147510.
- ^ "Comtess 200 mg film-coated Tablets – Summary of Product Characteristics (SmPC) – (emc)". www.medicines.org.uk. Retrieved 7 January 2021.
- ^ "Stalevo 150 mg/37.5 mg/200 mg Film-coated Tablets – Summary of Product Characteristics (SmPC) – (emc)". www.medicines.org.uk. Retrieved 7 January 2021.
- ^ "Ongentys 50 mg hard capsules – Summary of Product Characteristics (SmPC) – (emc)". www.medicines.org.uk. Retrieved 7 January 2021.
- ^ Goldenberg MM (October 2008). "Medical management of Parkinson's disease". P & T. 33 (10): 590–606. PMC 2730785. PMID 19750042.
- ^ a b c Samii A, Nutt JG, Ransom BR (May 2004). "Parkinson's disease". Lancet. 363 (9423): 1783–1793. doi:10.1016/S0140-6736(04)16305-8. PMID 15172778. S2CID 35364322.
- ^ Ceravolo R, Frosini D, Rossi C, Bonuccelli U (December 2009). "Impulse control disorders in Parkinson's disease: definition, epidemiology, risk factors, neurobiology and management". Parkinsonism & Related Disorders. 15 (Suppl 4): S111–S115. doi:10.1016/S1353-8020(09)70847-8. PMID 20123548.
- ^ Tolosa & Katzenschlager 2007, pp. 110–145.
- ^ Binde et al. 2018, p. 1924.
- ^ a b c Alborghetti M, Nicoletti F (2019). "Different Generations of Type-B Monoamine Oxidase Inhibitors in Parkinson's Disease: From Bench to Bedside". Current Neuropharmacology. 17 (9): 861–873. doi:10.2174/1570159X16666180830100754. PMC 7052841. PMID 30160213.
- ^ Ives NJ, Stowe RL, Marro J, Counsell C, Macleod A, Clarke CE, et al. (September 2004). "Monoamine oxidase type B inhibitors in early Parkinson's disease: meta-analysis of 17 randomised trials involving 3525 patients". BMJ. 329 (7466): 593. doi:10.1136/bmj.38184.606169.AE. PMC 516655. PMID 15310558.
- ^ Crosby N, Deane KH, Clarke CE (2003). "Amantadine in Parkinson's disease". The Cochrane Database of Systematic Reviews. 2003 (1): CD003468. doi:10.1002/14651858.CD003468. PMC 8715353. PMID 12535476.
- ^ a b The National Collaborating Centre for Chronic Conditions, ed. (2006). "Non-motor features of Parkinson's disease". Parkinson's Disease. London: Royal College of Physicians. pp. 113–133. ISBN 978-1-8601-6283-1. Archived from the original on 24 September 2010.
- ^ Hasnain M, Vieweg WV, Baron MS, Beatty-Brooks M, Fernandez A, Pandurangi AK (July 2009). "Pharmacological management of psychosis in elderly patients with parkinsonism". The American Journal of Medicine. 122 (7): 614–622. doi:10.1016/j.amjmed.2009.01.025. PMID 19559160.
- ^ Seppi K, Ray Chaudhuri K, Coelho M, Fox SH, Katzenschlager R, Perez Lloret S, et al. (February 2019). "Update on treatments for nonmotor symptoms of Parkinson's disease—an evidence-based medicine review". Movement Disorders. 34 (2): 180–198. doi:10.1002/mds.27602. PMC 6916382. PMID 30653247.
- ^ "FDA approves first drug to treat hallucinations and delusions associated with Parkinson's disease". FDA (Press release). 29 April 2016. Retrieved 12 October 2018.
- ^ a b Elbers RG, Verhoef J, van Wegen EE, Berendse HW, Kwakkel G (October 2015). "Interventions for fatigue in Parkinson's disease". The Cochrane Database of Systematic Reviews (Review). 2015 (10): CD010925. doi:10.1002/14651858.CD010925.pub2. PMC 9240814. PMID 26447539.
- ^ a b c d The National Collaborating Centre for Chronic Conditions, ed. (2006). "Surgery for Parkinson's disease". Parkinson's Disease. London: Royal College of Physicians. pp. 101–111. ISBN 978-1-8601-6283-1. Archived from the original on 24 September 2010.
- ^ Bronstein JM, Tagliati M, Alterman RL, Lozano AM, Volkmann J, Stefani A, et al. (February 2011). "Deep brain stimulation for Parkinson disease: an expert consensus and review of key issues". Archives of Neurology. 68 (2): 165. doi:10.1001/archneurol.2010.260. PMC 4523130. PMID 20937936.
- ^ a b Dallapiazza et al. 2018.
- ^ Ernst M, Folkerts AK, Gollan R, Lieker E, Caro-Valenzuela J, Adams A, et al. (April 2024). "Physical exercise for people with Parkinson's disease: a systematic review and network meta-analysis". The Cochrane Database of Systematic Reviews. 2024 (4): CD013856. doi:10.1002/14651858.CD013856.pub3. PMC 11001292. PMID 38588457.
- ^ Ahlskog JE (July 2011). "Does vigorous exercise have a neuroprotective effect in Parkinson disease?". Neurology. 77 (3): 288–294. doi:10.1212/wnl.0b013e318225ab66. PMC 3136051. PMID 21768599.
- ^ a b c d e The National Collaborating Centre for Chronic Conditions, ed. (2006). "Other key interventions". Parkinson's Disease. London: Royal College of Physicians. pp. 135–146. ISBN 978-1-8601-6283-1. Archived from the original on 24 September 2010.
- ^ a b Goodwin VA, Richards SH, Taylor RS, Taylor AH, Campbell JL (April 2008). "The effectiveness of exercise interventions for people with Parkinson's disease: a systematic review and meta-analysis". Movement Disorders. 23 (5): 631–640. doi:10.1002/mds.21922. hdl:10871/17451. PMID 18181210. S2CID 3808899.
- ^ Dereli EE, Yaliman A (April 2010). "Comparison of the effects of a physiotherapist-supervised exercise programme and a self-supervised exercise programme on quality of life in patients with Parkinson's disease". Clinical Rehabilitation. 24 (4): 352–362. doi:10.1177/0269215509358933. PMID 20360152. S2CID 10947269.
- ^ Jin X, Wang L, Liu S, Zhu L, Loprinzi PD, Fan X (December 2019). "The Impact of Mind-body Exercises on Motor Function, Depressive Symptoms, and Quality of Life in Parkinson's Disease: A Systematic Review and Meta-analysis". International Journal of Environmental Research and Public Health. 17 (1): 31. doi:10.3390/ijerph17010031. PMC 6981975. PMID 31861456.
- ^ O'Sullivan & Schmitz 2007, pp. 873, 876.
- ^ O'Sullivan & Schmitz 2007, p. 879.
- ^ O'Sullivan & Schmitz 2007, p. 877.
- ^ O'Sullivan & Schmitz 2007, p. 880.
- ^ a b c d e f g h i Barichella M, Cereda E, Pezzoli G (October 2009). "Major nutritional issues in the management of Parkinson's disease". Movement Disorders. 24 (13): 1881–1892. doi:10.1002/mds.22705. hdl:2434/67795. PMID 19691125. S2CID 23528416.
- ^ Ramazzina I, Bernazzoli B, Costantino C (31 March 2017). "Systematic review on strength training in Parkinson's disease: an unsolved question". Clinical Interventions in Aging. 12: 619–628. doi:10.2147/CIA.S131903. PMC 5384725. PMID 28408811.
- ^ Fox CM, Ramig LO, Ciucci MR, Sapir S, McFarland DH, Farley BG (November 2006). "The science and practice of LSVT/LOUD: neural plasticity-principled approach to treating individuals with Parkinson disease and other neurological disorders". Seminars in Speech and Language. 27 (4): 283–299. doi:10.1055/s-2006-955118. PMID 17117354. S2CID 260320960.
- ^ Dixon L, Duncan D, Johnson P, Kirkby L, O'Connell H, Taylor H, et al. (July 2007). "Occupational therapy for patients with Parkinson's disease". The Cochrane Database of Systematic Reviews. 2007 (3): CD002813. doi:10.1002/14651858.CD002813.pub2. PMC 6991932. PMID 17636709.
- ^ Ferrell B, Connor SR, Cordes A, Dahlin CM, Fine PG, Hutton N, et al. (June 2007). "The national agenda for quality palliative care: the National Consensus Project and the National Quality Forum". Journal of Pain and Symptom Management. 33 (6): 737–744. doi:10.1016/j.jpainsymman.2007.02.024. PMID 17531914.
- ^ a b Lorenzl S, Nübling G, Perrar KM, Voltz R (2013). "Palliative treatment of chronic neurologic disorders". Ethical and Legal Issues in Neurology. Handbook of Clinical Neurology. Vol. 118. Elsevier. pp. 133–139. doi:10.1016/B978-0-444-53501-6.00010-X. ISBN 978-0-4445-3501-6. PMID 24182372.
- ^ a b Ghoche R (December 2012). "The conceptual framework of palliative care applied to advanced Parkinson's disease". Parkinsonism & Related Disorders. 18 (Suppl 3): S2–S5. doi:10.1016/j.parkreldis.2012.06.012. PMID 22771241.
- ^ a b c Wilcox SK (January 2010). "Extending palliative care to patients with Parkinson's disease". British Journal of Hospital Medicine. 71 (1): 26–30. doi:10.12968/hmed.2010.71.1.45969. PMID 20081638.
- ^ Moens K, Higginson IJ, Harding R (October 2014). "Are there differences in the prevalence of palliative care-related problems in people living with advanced cancer and eight non-cancer conditions? A systematic review". Journal of Pain and Symptom Management. 48 (4): 660–677. doi:10.1016/j.jpainsymman.2013.11.009. PMID 24801658.
- ^ Casey G (August 2013). "Parkinson's disease: a long and difficult journey". Nursing New Zealand. 19 (7): 20–24. PMID 24195263.
- ^ a b c d Corcoran & Kluger 2021, p. 956.
- ^ Fereshtehnejad et al. 2017, p. 1967.
- ^ Tolosa et al. 2021, p. 385.
- ^ Dommershuijsen et al. 2023, pp. 2–3.
- ^ Murueta-Goyena, Muiño & Gómez-Esteban 2017, p. 26.
- ^ Murueta-Goyena, Muiño & Gómez-Esteban 2017, p. 27.
- ^ Caballol, Martí & Tolosa 2007, p. S358.
- ^ Murueta-Goyena, Muiño & Gómez-Esteban 2024, p. 395.
- ^ Atalar, Oguz & Genc 2023, p. 163.
- ^ Chua et al. 2024, p. 1.
- ^ Won JH, Byun SJ, Oh BM, Park SJ, Seo HG (23 March 2021). "Risk and mortality of aspiration pneumonia in Parkinson's disease: a nationwide database study". Scientific Reports. 11 (1): 6597. Bibcode:2021NatSR..11.6597W. doi:10.1038/s41598-021-86011-w. PMC 7988066. PMID 33758213.
- ^ Ben-Shlomo et al. 2024, p. 283.
- ^ Varden, Walker & O'Callaghan 2024, p. 1.
- ^ Zhu et al. 2024, p. e464.
- ^ a b Ben-Shlomo et al. 2024, p. 286.
- ^ Deliz, Tanner & Gonzalez-Latapi 2024, p. 166.
- ^ a b c Ben-Shlomo et al. 2024, p. 284.
- ^ Dorsey et al. 2018, p. S4.
- ^ a b Deliz, Tanner & Gonzalez-Latapi 2024, p. 165.
- ^ a b c d Ben-Shlomo et al. 2024, p. 285.
- ^ Li et al. 2019, p. 1.
- ^ a b Deliz, Tanner & Gonzalez-Latapi 2024, pp. 164–165.
- ^ Huang et al. 2024, pp. 1–2.
- ^ Lewis et al. 2020, p. 389.
- ^ Goetz 2011, pp. 1–2.
- ^ Lees 2007, p. S327.
- ^ a b c Goetz 2011, p. 2.
- ^ a b Louis 1997, p. 1069.
- ^ a b c d e Lees 2007, p. S328.
- ^ Lees 2007, p. S329.
- ^ Bereczki 2010, p. 290.
- ^ a b Blonder 2018, pp. 3–4.
- ^ Bereczki 2010, pp. 290–293.
- ^ Blonder 2018, p. 3.
- ^ Sousa-Santos, Pozzobon & Teixeira 2024, pp. 1–2.
- ^ Lees 2007, p. S331.
- ^ Fahn 2008, p. S500—S501, S504–S505.
- ^ Schulz-Schaeffer 2010, p. 131.
- ^ Lanska 2010, p. 507.
- ^ Guridi & Lozano 1997, pp. 1180–1183.
- ^ Fahn 2008, p. S497.
- ^ Fahn 2008, p. S501.
- ^ Coffey 2009, pp. 209–210.
- ^ Prenger MT, Madray R, Van Hedger K, Anello M, MacDonald PA (2020). "Social Symptoms of Parkinson's Disease". Parkinson's Disease. 2020: 8846544. doi:10.1155/2020/8846544. PMC 7790585. PMID 33489081.
- ^ a b Crooks S, Carter G, Wilson CB, Wynne L, Stark P, Doumas M, et al. (2023). "Exploring public perceptions and awareness of Parkinson's disease: A scoping review". PLOS ONE. 18 (9): e0291357. Bibcode:2023PLoSO..1891357C. doi:10.1371/journal.pone.0291357. PMC 10503766. PMID 37713383.
- ^ a b c Findley LJ (September 2007). "The economic impact of Parkinson's disease". Parkinsonism & Related Disorders. 13 (Suppl): S8–S12. doi:10.1016/j.parkreldis.2007.06.003. PMID 17702630.
- ^ Yang W, Hamilton JL, Kopil C, Beck JC, Tanner CM, Albin RL, et al. (2020). "Current and projected future economic burden of Parkinson's disease in the U.S". npj Parkinson's Disease. 6: 15. doi:10.1038/s41531-020-0117-1. PMC 7347582. PMID 32665974. Material was copied from this source, which is available under a Creative Commons Attribution 4.0 International License.
- ^ Lees 2007, pp. S327–S334
- ^ "Parkinson's – 'the shaking palsy'". GlaxoSmithKline. 1 April 2009. Archived from the original on 14 May 2011.
- ^ "National Parkinson Foundation – Mission". Archived from the original on 21 December 2010. Retrieved 28 March 2011.
- ^ "Education: Joy in Giving". Time. 18 January 1960. Archived from the original on 20 February 2011. Retrieved 2 April 2011.
- ^ "About PDF". Parkinson's Disease Foundation. Archived from the original on 15 May 2011. Retrieved 24 July 2016.
- ^ "American Parkinson Disease Association: Home". American Parkinson Disease Association. Archived from the original on 10 May 2012. Retrieved 9 August 2010.
- ^ "About EPDA". European Parkinson's Disease Association. 2010. Archived from the original on 15 August 2010. Retrieved 9 August 2010.
- ^ "Notable Figures with Parkinson's". Parkinson's Foundation. Retrieved 22 November 2023.
- ^ "Michael's Story". The Michael J. Fox Foundation for Parkinson's Research. Retrieved 7 May 2023.
- ^ Davis P (3 May 2007). "Michael J. Fox". The Time 100. New York: Time. Archived from the original on 25 April 2011. Retrieved 2 April 2011.
- ^ Brockes E (11 April 2009). "'It's the gift that keeps on taking'". The Guardian. Archived from the original on 8 October 2013. Retrieved 25 October 2010.
- ^ Burleson 2023.
- ^ Brey RL (April 2006). "Muhammad Ali's Message: Keep Moving Forward". Neurology Now. 2 (2): 8. doi:10.1097/01222928-200602020-00003. Archived from the original on 27 September 2011. Retrieved 22 August 2020.
- ^ Matthews W (April 2006). "Ali's Fighting Spirit". Neurology Now. 2 (2): 10–23. doi:10.1097/01222928-200602020-00004. S2CID 181104230.
- ^ Tauber 1988.
- ^ Macur J (26 March 2008). "For the Phinney Family, a Dream and a Challenge". The New York Times. Archived from the original on 6 November 2014. Retrieved 25 May 2013.
About 1.5 million Americans have received a diagnosis of Parkinson's disease, but only 5 to 10 percent learn of it before age 40, according to the National Parkinson Foundation. Davis Phinney was among the few.
- ^ "Who We Are". Davis Phinney Foundation. Archived from the original on 11 January 2012. Retrieved 18 January 2012.
- ^ Luca A, Nicoletti A, Mostile G, Zappia M (2018). "The Parkinsonian Personality: More Than Just a "Trait"". Frontiers in Neurology. 9 (1191): 1–2. PMID 30697187.
- ^ Gerstenbrand 2007, p. 121.
- ^ McCrum R (20 November 2017). "The 100 best nonfiction books: No 94 – Leviathan by Thomas Hobbes (1651)". The Guardian. Retrieved 23 November 2023.
- ^ Kinsley M (21 April 2014). "Have You Lost Your Mind?". The New Yorker. Retrieved 23 November 2023.
- ^ Raudino F (2011). "The Parkinson disease before James Parkinson". History of Neurology. 33: 945–949.
- ^ Gupta R, Kim C, Agarwal N, Lieber B, Monaco EA (2015). "Understanding the Influence of Parkinson Disease on Adolf Hitler's Decision-Making during World War II". World Neurosurgery. 84 (5): 1447–1452. doi:10.1016/j.wneu.2015.06.014. PMID 26093359.
- ^ Boettcher L, Bonney P, Smitherman A, Sughrue M (2015). "Hitler's parkinsonism". Neurosurgical Focus. 39 (1): E8. doi:10.3171/2015.4.FOCUS1563.
- ^ Gerstenbrand 2007, pp. 121–125.
- ^ Glass 2016.
- ^ Mari Z, Mestre TA (2022). "The Disease Modification Conundrum in Parkinson's Disease: Failures and Hopes". Frontiers in Aging Neuroscience. 14: 810860. doi:10.3389/fnagi.2022.810860. PMC 8920063. PMID 35296034.
- ^ McFarthing K, Rafaloff G, Baptista M, Mursaleen L, Fuest R, Wyse RK, et al. (24 May 2022). "Parkinson's Disease Drug Therapies in the Clinical Trial Pipeline: 2022 Update". Journal of Parkinson's Disease. 12 (4): 1073–1082. doi:10.3233/JPD-229002. PMC 9198738. PMID 35527571.
- ^ a b Poewe W, Seppi K, Tanner CM, Halliday GM, Brundin P, Volkmann J, et al. (March 2017). "Parkinson disease". Nature Reviews. Disease Primers. 3 (1): 17013. doi:10.1038/nrdp.2017.13. PMID 28332488. S2CID 11605091.
- ^ Heinzel S, Berg D, Gasser T, Chen H, Yao C, Postuma RB (October 2019). "Update of the MDS research criteria for prodromal Parkinson's disease". Movement Disorders. 34 (10): 1464–1470. doi:10.1002/mds.27802. PMID 31412427. S2CID 199663713.
- ^ Sudhakar V, Richardson RM (January 2019). "Gene Therapy for Neurodegenerative Diseases". Neurotherapeutics. 16 (1): 166–175. doi:10.1007/s13311-018-00694-0. PMC 6361055. PMID 30542906.
- ^ Hitti FL, Yang AI, Gonzalez-Alegre P, Baltuch GH (September 2019). "Human gene therapy approaches for the treatment of Parkinson's disease: An overview of current and completed clinical trials". Parkinsonism & Related Disorders. 66: 16–24. doi:10.1016/j.parkreldis.2019.07.018. PMID 31324556. S2CID 198132349.
- ^ Volc D, Poewe W, Kutzelnigg A, Lührs P, Thun-Hohenstein C, Schneeberger A, et al. (July 2020). "Safety and immunogenicity of the α-synuclein active immunotherapeutic PD01A in patients with Parkinson's disease: a randomised, single-blinded, phase 1 trial". The Lancet. Neurology. 19 (7): 591–600. doi:10.1016/S1474-4422(20)30136-8. PMID 32562684. S2CID 219947651.
- ^ "World's first Parkinson's vaccine is trialled". New Scientist. London. 7 June 2012. Archived from the original on 23 April 2015.
- ^ Jankovic J, Goodman I, Safirstein B, Marmon TK, Schenk DB, Koller M, et al. (October 2018). "Safety and Tolerability of Multiple Ascending Doses of PRX002/RG7935, an Anti-α-Synuclein Monoclonal Antibody, in Patients With Parkinson Disease: A Randomized Clinical Trial". JAMA Neurology. 75 (10): 1206–1214. doi:10.1001/jamaneurol.2018.1487. PMC 6233845. PMID 29913017.
- ^ Parmar, Grealish & Henchcliffe 2020, pp. 103.
- ^ Parmar, Grealish & Henchcliffe 2020, pp. 103–104.
- ^ Parmar, Grealish & Henchcliffe 2020, pp. 106.
- ^ Henchcliffe & Parmar 2018, pp. 134.
- ^ Parmar, Grealish & Henchcliffe 2020, pp. 106, 108.
- ^ Schweitzer JS, Song B, Herrington TM, Park TY, Lee N, Ko S, et al. (May 2020). "Personalized iPSC-Derived Dopamine Progenitor Cells for Parkinson's Disease". The New England Journal of Medicine. 382 (20): 1926–1932. doi:10.1056/NEJMoa1915872. PMC 7288982. PMID 32402162.
- ^ Parmar, Grealish & Henchcliffe 2020, pp. 105, 109.
- ^ Henchcliffe & Parmar 2018, pp. 132.
- ^ Jenner P (2014). "An overview of adenosine A2A receptor antagonists in Parkinson's disease". International Review of Neurobiology. 119: 71–86. doi:10.1016/B978-0-12-801022-8.00003-9. ISBN 978-0-1280-1022-8. PMID 25175961.
- ^ a b Office of the Commissioner (20 February 2020). "FDA approves new add-on drug to treat off episodes in adults with Parkinson's disease". FDA. Retrieved 23 February 2020.
- ^ Blauwendraat, Nalls & Singleton 2020, pp. 2.
- ^ Torres-Pasillas G, Chi-Castañeda D, Carrillo-Castilla P, Marín G, Hernández-Aguilar ME, Aranda-Abreu GE, et al. (5 June 2023). "Olfactory Dysfunction in Parkinson's Disease, Its Functional and Neuroanatomical Correlates". NeuroSci. 4 (2): 134–151. doi:10.3390/neurosci4020013. PMC 11523736. PMID 39483318.
Works cited
[edit]Books
[edit]- Bhattacharyya KB (2017). "Chapter One - Hallmarks of Clinical Aspects of Parkinson's Disease Through Centuries". In Bhatia KP, Chaudhuri KR, Stamelou M (eds.). Parkinson's Disease. International Review of Neurobiology. pp. 1–23.
- Cooper G, Eichhorn G, Rodnitzky RL (2008). "Parkinson's disease". In Conn PM (ed.). Neuroscience in medicine. Humana Press. ISBN 978-1-6032-7454-8.
- Dissanayaka NN (8 March 2021). "Chapter 9: Anxiety in Parkinson's Disease". In Byrne GJ, Panchana NA (eds.). Anxiety in Older People: Clinical and Research Perspectives. Cambridge University Press. pp. 139–156. doi:10.1017/9781139087469.009. ISBN 978-1-1088-2636-5. S2CID 87250745.
- Ferri FF (2010). "Chapter P". Ferri's differential diagnosis: a practical guide to the differential diagnosis of symptoms, signs, and clinical disorders (2nd ed.). Elsevier/Mosby. ISBN 978-0-3230-7699-9.
- Lanska DJ (2010). "Chapter 33: The history of movement disorders". Handbook of Clinical Neurology. 3. Vol. 95. History of Neurology. pp. 501–546. doi:10.1016/S0072-9752(08)02133-7. ISBN 978-0-444-52009-8. PMID 19892136.
- O'Sullivan SB, Schmitz TJ (2007). "Parkinson's Disease". Physical Rehabilitation (5th ed.). F.A. Davis. ISBN 978-0-8036-1247-1.
- Simon RP, Greenberg D, Aminoff MJ (2017). Lange Clinical Neurology (10th ed.). McGraw-Hill. ISBN 978-1-2598-6172-7.
- Stoker TB, Greenland JC, eds. (December 2018). Parkinson's Disease: Pathogenesis and Clinical Aspects. Codon Publications. ISBN 978-0-9944-3816-4.
- Dallapiazza RF, De Vloo PD, Fomenko A, Lee DJ, Hamani C, Munhoz RP, et al. (2018). "Chapter 8: Considerations for Patient and Target Selection in Deep Brain Stimulation surgery for Parkinson's disease". In Stoker TB, Greenland JC (eds.). Parkinson's disease: Pathogenesis and Clinical Aspects. Codon Publications. doi:10.15586/codonpublications.parkinsonsdisease.2018.ch8. ISBN 978-0-9944-3816-4. PMID 30702838. S2CID 81155324.
- Greenland JC, Barker RA (2018). "Chapter 6: The Differential Diagnosis of Parkinson's Disease". In Stoker TB, Greenland JC (eds.). Parkinson's disease: Pathogenesis and Clinical Aspects. Codon Publications. pp. 109–128. doi:10.15586/codonpublications.parkinsonsdisease.2018.ch6. ISBN 978-0-9944-3816-4. PMID 30702839. S2CID 80908095.
- Stoker TB, Torsney KM, Barker RA (2018). "Chapter 3: Pathological mechanisms and clinical aspects of GBA1 mutation-associated Parkinson's disease". In Stoker TB, Greenland JC (eds.). Parkinson's Disease: Pathogenesis and clinical aspects. pp. 45–64. doi:10.15586/codonpublications.parkinsonsdisease.2018.ch3. ISBN 978-0-9944-3816-4. PMID 30702840. S2CID 92170834.
- Tolosa E, Jankovic E, eds. (2007). Parkinson's disease and movement disorders. Lippincott Williams & Wilkins. ISBN 978-0-7817-7881-7.
- Dickson DV (2007). "Neuropathology of movement disorders". In Tolosa E, Jankovic JJ (eds.). Parkinson's disease and movement disorders. Lippincott Williams & Wilkins. ISBN 978-0-7817-7881-7.
- Fung VS, Thompson PD (2007). "Rigidity and spasticity". In Tolosa E, Jankovic E (eds.). Parkinson's disease and movement disorders. Lippincott Williams & Wilkins. ISBN 978-0-7817-7881-7.
- Tolosa E, Katzenschlager R (2007). "Pharmacological management of Parkinson's disease". In Tolosa E, Jankovic JJ (eds.). Parkinson's disease and movement disorders. Lippincott Williams & Wilkins. ISBN 978-0-7817-7881-7.
- Truong DD, Bhidayasiri R (2016). "50: Parkinson's disease". In Lisak RP, Truong DD, Carroll WM, Bhidayasiri R (eds.). International Neurology. John Wiley & Sons. ISBN 978-1-1187-7736-7.
Journal articles
[edit]- Binde CD, Tvete IF, Gåsemyr J, Natvig B, Klemp M (September 2018). "A multiple treatment comparison meta-analysis of monoamine oxidase type B inhibitors for Parkinson's disease". British Journal of Clinical Pharmacology. 84 (9): 1917–1927. doi:10.1111/bcp.13651. PMC 6089809. PMID 29847694.
- Caballol N, Martí MJ, Tolosa E (September 2007). "Cognitive dysfunction and dementia in Parkinson disease". Mov. Disord. 22 (Suppl 17): S358–66. doi:10.1002/mds.21677. PMID 18175397. S2CID 3229727.
- Henchcliffe C, Parmar M (2018). "Repairing the Brain: Cell Replacement Using Stem Cell-Based Technologies". Journal of Parkinson's Disease. 8 (s1): S131–S137. doi:10.3233/JPD-181488. PMC 6311366. PMID 30584166.
- Panicker N, Ge P, Dawson VL, Dawson TM (April 2021). "The cell biology of Parkinson's disease". The Journal of Cell Biology. 220 (4). doi:10.1083/jcb.202012095. PMC 8103423. PMID 33749710.
- Parmar M, Grealish S, Henchcliffe C (February 2020). "The future of stem cell therapies for Parkinson disease". Nature Reviews. Neuroscience. 21 (2): 103–115. doi:10.1038/s41583-019-0257-7. PMID 31907406.
- Tolosa E, Garrido A, Scholz SW, Poewe W (May 2021). "Challenges in the diagnosis of Parkinson's disease". The Lancet. Neurology. 20 (5): 385–397. doi:10.1016/S1474-4422(21)00030-2. PMC 8185633. PMID 33894193.
- Blauwendraat C, Nalls MA, Singleton AB (February 2020). "The genetic architecture of Parkinson's disease". The Lancet. Neurology. 19 (2): 170–178. doi:10.1016/S1474-4422(19)30287-X. PMC 8972299. PMID 31521533.
- Winiker K, Kertscher B (2023). "Behavioural interventions for swallowing in subjects with Parkinson's disease: A mixed methods systematic review". International Journal of Language & Communication Disorders. 58 (4): 1375–1404. doi:10.1111/1460-6984.12865. PMID 36951546.
 This article incorporates text from this source, which is available under the CC BY 4.0 license.
This article incorporates text from this source, which is available under the CC BY 4.0 license. - Islam MS, Azim F, Saju H, Zargaran A, Shirzad M, Kamal M, et al. (September 2021). "Pesticides and Parkinson's disease: Current and future perspective". Journal of Chemical Neuroanatomy. 115: 101966. doi:10.1016/j.jchemneu.2021.101966. PMC 8842749. PMID 33991619.
- Hansen D, Ling H, Lashley T, Holton JL, Warner TT (April 2019). "Review: Clinical, neuropathological and genetic features of Lewy body dementias". Neuropathology and Applied Neurobiology. 45 (7): 635–654. doi:10.1111/nan.12554. PMID 30977926.
- Wallace ER, Segerstrom SC, van Horne CG, Schmitt FA, Koehl LM (2022). "Meta-Analysis of Cognition in Parkinson's Disease Mild Cognitive Impairment and Dementia Progression". Neuropsychology Review. 32 (1): 149–160. doi:10.1007/s11065-021-09502-7. PMID 33860906.
- Dolgacheva LP, Zinchenko VP, Goncharov NV (2022). "Molecular and Cellular Interactions in Pathogenesis of Sporadic Parkinson Disease". International Journal of Molecular Sciences. 23 (21): 13043. doi:10.3390/ijms232113043. PMC 9657547. PMID 36361826.
- Leta V, Urso D, Batzu L, Lau YH, Mathew D, Boura I, et al. (2022). "Viruses, parkinsonism and Parkinson's disease: the past, present and future". Journal of Neural Transmission. 129 (9): 1119–1132. doi:10.1007/s00702-022-02536-y. PMC 9422946. PMID 36036863.
- Langston JW (2017). "The MPTP Story". Journal of Parkinson's Disease. 7 (S1): S11–S19. doi:10.3233/JPD-179006. PMC 5345642. PMID 28282815.
- Limphaibool N, Iwanowski P, Holstad MJ, Kobylarek D, Kozubski W (2019). "Infectious Etiologies of Parkinsonism: Pathomechanisms and Clinical Implications". Frontiers in Neurology. 10: 652. doi:10.3389/fneur.2019.00652. PMC 6593078. PMID 31275235.
- Bologna M, Truong D, Jankovic J (2022). "The etiopathogenetic and pathophysiological spectrum of parkinsonism". Journal of the Neurological Sciences. 433: 1–8. doi:10.1016/j.jns.2021.120012. PMID 34642022.
- Prajjwal P, Kolanu ND, Reddy YB, Ahmed A, Marsool MD, Santoshi K, et al. (2024). "Association of Parkinson's disease to Parkinson's plus syndromes, Lewy body dementia, and Alzheimer's dementia". Health Science Reports. 7 (4): e2019. doi:10.1002/hsr2.2019. PMC 10982460. PMID 38562616.
- Olfatia N, Shoeibia A, Litvanb I (2019). "Progress in the treatment of Parkinson-Plus syndromes". Parkinsonism & Related Disorders. 59: 101–110. doi:10.1016/j.parkreldis.2018.10.006. PMID 30314846.
- Calabresi P, Mechelli A, Natale G, Volpicelli-Daley L, Di Lazzaro G, Ghiglieri V (2023). "Alpha-synuclein in Parkinson's disease and other synucleinopathies: from overt neurodegeneration back to early synaptic dysfunction". Cell Death & Disease. 14 (3): 176. doi:10.1038/s41419-023-05672-9. PMC 9977911. PMID 36859484.
- Ramesh SD, Arachchige AS (2023). "Depletion of dopamine in Parkinson's disease and relevant therapeutic options: A review of the literature". AIMS Neuroscience. 10 (3): 200–231. doi:10.3934/Neuroscience.2023017. PMC 10567584. PMID 37841347.
- Ascherio A, Schwarzschild MA (2016). "The epidemiology of Parkinson's disease: risk factors and prevention". Lancet Neurology. 15 (12): 1257–1272. doi:10.1016/S1474-4422(16)30230-7. PMID 27751556.
- Crotty GF, Schwarzschild MA (2020). "Chasing Protection in Parkinson's Disease: Does Exercise Reduce Risk and Progression?". Frontiers in Aging Neuroscience. 12: 186. doi:10.3389/fnagi.2020.00186. PMC 7318912. PMID 32636740.
- Singh A, Tripathi P, Singh S (2021). "Neuroinflammatory responses in Parkinson's disease: relevance of Ibuprofen in therapeutics". Inflammopharmacology. 29 (1): 5–14. doi:10.1007/s10787-020-00764-w. PMID 33052479.
- Fabbri M, Rascol O, Foltynie T, Carroll C, Postuma RB, Porcher R, et al. (2024). "Advantages and Challenges of Platform Trials for Disease Modifying Therapies in Parkinson's Disease". Movement Disorders. 39 (9): 1468–1477. doi:10.1002/mds.29899. PMID 38925541.
- Kamal H, Tan GC, Ibrahim SF, Shaikh MF, Mohamed IN, Mohamed RM, et al. (2020). "Alcohol Use Disorder, Neurodegeneration, Alzheimer's and Parkinson's Disease: Interplay Between Oxidative Stress, Neuroimmune Response and Excitotoxicity". Frontiers in Cellular Neuroscience. 14: 282. doi:10.3389/fncel.2020.00282. PMC 7488355. PMID 33061892.
- Lin J, Pang D, Li C, Ou R, Yu Y, Cui Y, et al. (2024). "Calcium channel blockers and Parkinson's disease: a systematic review and meta-analysis". Therapeutic Advances in Neurological Disorders. 17: 1–8. doi:10.1177/17562864241252713. PMC 11104025. PMID 38770432.
- Grotewolda N, Albina RL (2024). "Update: Protective and risk factors for Parkinson disease". Parkinsonism and Related Disorders. 125: 1–12. doi:10.1016/j.parkreldis.2024.107026. PMID 38879999.
- Rose KN, Schwarzschild MS, Gomperts SN (2024). "Clearing the Smoke: What Protects Smokers from Parkinson's Disease?". Movement Disorders. 39 (2): 267–272. doi:10.1002/mds.29707. PMC 10923097. PMID 38226487.
- Ren X, Chen J (2020). "Caffeine and Parkinson's Disease: Multiple Benefits and Emerging Mechanisms". Frontiers in Neuroscience. 14: 1–12. doi:10.3389/fnins.2020.602697. PMC 7773776. PMID 33390888.
- Ben-Shlomo Y, Darweesh S, Llibre-Guerra J, Marras C, Luciano MS, Tanner C (2024). "The epidemiology of Parkinson's disease". The Lancet. 403 (10423): 283–292. doi:10.1016/S0140-6736(23)01419-8. PMC 11123577. PMID 38245248.
- Deliz JR, Tanner CM, Gonzalez-Latapi P (2024). "Epidemiology of Parkinson's Disease: An Update". Current Neurology and Neuroscience Reports. 24 (6): 163–179. doi:10.1007/s11910-024-01339-w. PMID 38642225.
- Dorsey ER, Sherer T, Okun MS, Bloem BR (2018). "The Emerging Evidence of the Parkinson Pandemic". Journal of Parkinson's Disease. 8 (s1): S3–S8. doi:10.3233/JPD-181474. PMC 6311367. PMID 30584159.
- Li G, Ma J, Cui S, He Y, Xiao Q, Liu J, et al. (2019). "Parkinson's disease in China: a forty-year growing track of bedside work". Translational Neurodegeneration. 8 (1): 22. doi:10.1186/s40035-019-0162-z. PMC 6668186. PMID 31384434.
- Varden R, Walker R, O'Callaghan A (2024). "No trend to rising rates: A review of Parkinson's prevalence studies in the United Kingdom". Parkinsonism & Related Disorders. 128: 1–6. doi:10.1016/j.parkreldis.2024.107015. PMID 38876845.
- Zhu J, Cui Y, Zhang J, Yan R, Su D, Zhao D, et al. (2024). "Temporal trends in the prevalence of Parkinson's disease from 1980 to 2023: a systematic review and meta-analysis". The Lancet: Healthy Longetivity. 5: e464–e479. doi:10.1016/j.parkreldis.2024.107015. PMID 38876845.
- Goetz CG (2011). "The history of Parkinson's disease: early clinical descriptions and neurological therapies". Cold Spring Harbor Perspectives in Medicine. 1 (1): a008862. doi:10.1101/cshperspect.a008862. PMC 3234454. PMID 22229124.
- Lees AJ (2007). "Unresolved issues relating to the shaking palsy on the celebration of James Parkinson's 250th birthday". Movement Disorders. 22 (S17): S327–S334. doi:10.1002/mds.21684. PMID 18175393.
- Louis ED (1997). "The shaking palsy, the first forty-five years: a journey through the British literature". Movement Disorders. 12 (6): 1068–1072. doi:10.1002/mds.870120638. PMID 9399240.
- Lewis PA, Plun-Favreau H, Rowley M, Spillane J (2020). "Pierre D. and the first photographs of Parkinson's disease". Movement Disorders. 35 (3): 389–391. doi:10.1002/mds.27965. PMC 7155099. PMID 31975439.
- Bereczki D (2010). "The description of all four cardinal signs of Parkinson's disease in a Hungarian medical text published in 1690". Parkinsonism & Related Disorders. 16 (4): 290–293. doi:10.1016/j.parkreldis.2009.11.006. PMID 19948422.
- Blonder LX (2018). "Historical and cross-cultural perspectives on Parkinson's disease". Journal of Complementary and Integrative Medicine. 15 (3): 1–15. doi:10.1515/jcim-2016-0065. PMID 29738310.
- Coffey RJ (2009). "Deep brain stimulation devices: a brief technical history and review". Artificial Organs. 33 (3): 208–220. doi:10.1111/j.1525-1594.2008.00620.x. PMID 18684199.
- Sousa-Santos PE, Pozzobon PM, Teixeira IL (2024). "Frederic Lewy: how the two World Wars changed his life, work, and name". Arquivos de Neuro-Psiquiatri. 82 (3): 001–002. doi:10.1055/s-0044-1779692. PMC 10927365. PMID 38467394.
- Fahn S (2008). "The history of dopamine and levodopa in the treatment of Parkinson's disease". Movement Disorders. 23 (S3): S497–S508. doi:10.1002/mds.22028. PMID 18781671.
- Schulz-Schaeffer WJ (2010). "The synaptic pathology of alpha-synuclein aggregation in dementia with Lewy bodies, Parkinson's disease and Parkinson's disease dementia". Acta Neuropathologica. 120 (2): 131–143. doi:10.1007/s00401-010-0711-0. PMC 2892607. PMID 20563819.
- Guridi J, Lozano AM (1997). "A brief history of pallidotomy". Neurosurgery. 41 (5): 1169–1180. doi:10.1097/00006123-199711000-00029. PMID 9361073.
- Tolosa E, Garrido A, Scholz SW, Poewe W (May 2021). "Challenges in the diagnosis of Parkinson's disease". Lancet Neurology. 20 (5): 385–397. doi:10.1016/S1474-4422(21)00030-2. PMC 8185633. PMID 33894193.
- Corcoran J, Kluger BM (September 2023). "Prognosis in chronic progressive neurologic disease: a narrative review". Annals of Palliative Medicine. 12 (5): 952–962. doi:10.21037/apm-22-1338. PMID 37691335.
- Fereshtehnejad SM, Zeighami Y, Dagher A, Postuma RB (July 2017). "Clinical criteria for subtyping Parkinson's disease: biomarkers and longitudinal progression". Brain. 140 (7): 1959–1976. doi:10.1093/brain/awx118. PMID 28549077.
- Dommershuijsen LJ, Darweesh SK, Ben-Shlomo Y, Kluger BM, Bloem BR (October 2023). "The elephant in the room: critical reflections on mortality rates among individuals with Parkinson's disease". npj Parkinson's Disease. 9 (1): 145. doi:10.1038/s41531-023-00588-9. PMC 10587193. PMID 37857675.
- Murueta-Goyena A, Muiño O, Gómez-Esteban JC (April 2024). "Prognostic factors for falls in Parkinson's disease: a systematic review". Acta Neurologica Belgica. 124 (2): 395–406. doi:10.1007/s13760-023-02428-2. PMC 10965733. PMID 38015306.
- Murueta-Goyena A, Muiño O, Gómez-Esteban JC (March 2017). "Dementia in Parkinson's disease". Journal of the Neurological Sciences. 374: 26–31. doi:10.1016/j.jns.2017.01.012. PMID 28088312.
- Chua WY, Wang JD, Chan CK, Chan L, Tan E (September 2024). "Risk of aspiration pneumonia and hospital mortality in Parkinson disease: A systematic review and meta-analysis". European Journal of Neurology. 31 (12): e16449. doi:10.1111/ene.16449. PMC 11555015. PMID 39236309.
- Won JH, Byun SJ, Oh B, Park SJ, Seo HG (September 2007). "Cognitive dysfunction and dementia in Parkinson disease". Scientific Reports. 22 (S17): S358–S366. doi:10.1002/mds.21677. PMID 18175397.
- Corcoran J, Kluger BM (2021). "Risk and mortality of aspiration pneumonia in Parkinson's disease: a nationwide database study". Scientific Reports. 11 (1): 6597. Bibcode:2021NatSR..11.6597W. doi:10.1038/s41598-021-86011-w. PMC 7988066. PMID 33758213.
- Atalar MS, Oguz O, Genc G (2023). "Hypokinetic Dysarthria in Parkinson's Disease: A Narrative Review". The Medical Bulletin of Sisle Etfal Hospital. 57 (2): 163–170. doi:10.14744/SEMB.2023.29560. PMC 10600629. PMID 37899809.
- Huang M, Bargues-Carot A, Riaz Z, Wickham H, Zenitsky G, Jin H, et al. (September 2022). "Impact of Environmental Risk Factors on Mitochondrial Dysfunction, Neuroinflammation, Protein Misfolding, and Oxidative Stress in the Etiopathogenesis of Parkinson's Disease". International Journal of Molecular Sciences. 23 (10808): 1–30. PMID 36142718.
- Gerstenbrand F, Karamat E (2007). "Adolf Hitler's Parkinson's disease and an attempt to analyse his personality structure". European Journal of Neurology. 6 (2): 121–127. doi:10.1111/j.1468-1331.1999.tb00003.x.
- Luca A, Nicoletti A, Mostile G, Zappia M (2018). "The Parkinsonian Personality: More Than Just a "Trait"". Frontiers in Neurology. 9 (1191): 1–2. PMID 30697187.
Web sources
[edit]- "Parkinson's Disease". National Institute of Neurological Disorders and Stroke. Retrieved 2 September 2024.
- "Symptoms of PD". Stanford Parkinson's Community Outreach. Stanford University School Medicine. Retrieved 2 September 2024.
News publications
[edit]- Burleson N, Breen K (9 November 2023). "Michael J. Fox talks funding breakthrough research for Parkinson's disease". CBS News. Retrieved 23 November 2023.
- Glass A (9 September 2016). "Mao Zedong dies in Beijing at age 82, Sept. 9, 1976". Politico. Retrieved 30 October 2023.
- Tauber P (17 July 1988). "Ali: Still Magic". The New York Times. Archived from the original on 17 November 2016. Retrieved 2 April 2011.











