User:Typicalmarco/sandbox
Wooden Chest Syndrome
[edit]Abstract
[edit]
Wooden Chest Syndrome (WCS) is a very rare but sometimes severe complication that is primarily associated with the administration of fentanyl, a synthetic opioid. This disease is typically characterized by a profound rigidity of the chest wall and the diaphragm. Wooden Chest Syndrome (WCS) can become fatal if left untreated. We will review the clinical presentation, mechanisms, diagnostic approaches , and management strategies.[1][2][3]
Signs and symptoms
[edit]
Wooden Chest Syndrome (WCS) is characterized by a sudden and severe rigidity of the chest wall muscles, diaphragm and upper airways. This unfortunately leads to difficulty breathing and can be life threatening if left untreated. Most patients present with the following symptoms: hypoxia, cyanosis, and elevated pressures during mechanical ventilation[1][4]. In various cases, the symptoms of WCS can be confused with other conditions (ex. Acute respiratory distress syndrome (ARDS))[4].
Cause
[edit]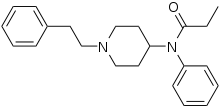
The primary cause of wooden chest syndrome (WCS) is the administration of fentanyl. This is a synthetic opioid that is widely used in the medical field. It is known for its rapid onset effects, however, in rare circumstances can lead to WCS which would include severe muscle rigidity regardless of dosage. There are actually cases where a minimal amount of fentanyl is administered to the patient and they still seem to negatively react to this medication. [1][2].
Pathophysiology
[edit]
The pathophysiology of WCS involves the binding of fentanyl to the mu-opioid receptors in the central nervous system. This, unfortunately, triggers a multitude of events leading to muscle rigidity. Furthering this point, noradrenergic and cholinergic pathways are activated resulting in a decreased in chest wall function and an increase in rigidity resulting in ineffective ventilation[1][3][5]. As a result, lung expansion is reduced and oxygen intake is tampered.In the brainstem of the human body, the effect of fentanyl on the respiratory centers likely contributes to a decreased neural output to the respiratory muscles leading to the infamous rigidity.[1] This, however, is still being investigated.
Diagnosis
[edit]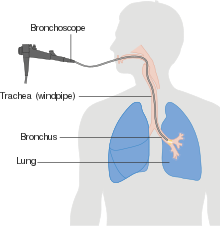
Diagnosis of Wooden Chest Syndrome (WCS) is typically made in a healthcare setting by a doctor (non-emergency or emergency). This syndrome is diagnosed when a patient begins exhibiting a rapid-onset of respiratory distress, typically after fentanyl administration. Key diagnostic indicators that a patient may be suffering from this syndrome are as follows: sudden onset of elevated airway pressures, hypoxia, and even resistance to ventilation despite no apparent airway obstruction[1][3]. Diagnosis, however, can be difficult to establish as it requires a rapid identification of symptoms and opioid knowledge. Although a bronchoscopy and chest X-ray can help rule out any other causes, there are no specific tests (laboratory or imaging) that can totally confirm WCS[1].[5]
Treatment
[edit]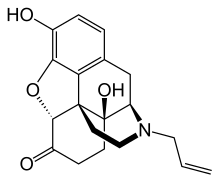
Management of Wooden Chest Syndrome (WCS) involves an immediate cease to fentanyl administration followed by the administration of an opioid receptor antogonist such as Naloxone[1][3]. Naloxone, although able to reduce the opioid effects, may not be able to reduce muscle rigidity. This is where respiratory support, such as ventilation is introduced to the patient to help counteract restricted breathing. Neuromuscular blocking agents such as Rucuronium can also be used to alleviate muscle rigidity.[1][3] There are also non-medical measures that can be initiated while the pharmacological agents are taking effect such as manual ventilation and body positioning to increase breathing capabilities.[1]
Prognosis
[edit]The prognosis for Wooden Chest Syndrome (WCS) varies by individual case-to-case basis. If promptness and efficacy are taken into account, patients can recover without long-term complications. However, if treatment and diagnosis are delayed, potential fatal outcomes can arise. This syndrome has a higher reoccurrence rate among individuals with opioid-dependence (recreational use) or those undergoing medical treatment that requires repeated administration of fentanyl.[1] There is currently no genetic risk factors, however prognosis does worsen with age[1]. Older adults are at higher risk for severe respiratory complications more so than younger individuals.[1]
Epidemiology
[edit]Wooden Chest Syndrome (WCS) is a rare condition that is becoming more prevalent with the increased use of fentanyl, both in a medical and recreational setting[1]. Although demographic data is currently scarce, evidence does suggest there is no correlation between geographic or ethnic predispositions.[1]
Research Directions
[edit]Recent research has explored fentanyl’s neuromuscular effects. As mentioned in a 2020 case by Dasgupta, there are cases that were reviewed to better understand the mechanisms underlying opioid -induced rigidity[5]. Future research on this syndrome, however, should focus on improving the understanding of the mechanisms that underlie this condition and aid in development of more effective treatment strategies.
References
[edit]- ^ a b c d e f g h i j k l m n o Rosal, N.; Thelmo, Franklin L.; Tzarnas, Stephanie; DiCalvo, L.; Tariq, S.; Grossman, C. (2021). "Wooden Chest Syndrome: A Case Report of Fentanyl-Induced Chest Wall Rigidity". Journal of Investigative Medicine High Impact Case Reports. 9. doi:10.1177/23247096211034036.
- ^ a b Torralva, Randy; Janowsky, A. (2019). "Noradrenergic Mechanisms in Fentanyl-Mediated Rapid Death Explain Failure of Naloxone in the Opioid Crisis". The Journal of Pharmacology and Experimental Therapeutics. 371: 453–475. doi:10.1124/jpet.119.258566.
- ^ a b c d e UL HUSNA, ASHMA; NEUPANE, RASIK; HOWSARE, MOLLY M; NIRAULA, NIRAJ (2023-10). "WOODEN CHEST SYNDROME: A RARE COMPLICATION OF FENTANYL INFUSION". CHEST. 164 (4): A2759. doi:10.1016/j.chest.2023.07.1820. ISSN 0012-3692.
{{cite journal}}: Check date values in:|date=(help) - ^ a b Zoorob, Ronza; Uptegrove, Logan; Park, Benjamin L. (2023). "Case Report of Very-Low-Dose Fentanyl Causing Fentanyl-Induced Chest Wall Rigidity". Cureus. 15. doi:10.7759/cureus.43788.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c Cite error: The named reference
:4was invoked but never defined (see the help page).
- ^ Cite error: The named reference
:0was invoked but never defined (see the help page). - ^ Cite error: The named reference
:1was invoked but never defined (see the help page). - ^ Cite error: The named reference
:3was invoked but never defined (see the help page). - ^ Cite error: The named reference
:2was invoked but never defined (see the help page). - ^ Judd, G. I.; Starcher, R. W.; Hotchkin, D. (2021). "Fentanyl-Induced Wooden Chest Syndrome Masquerading as Severe Respiratory Distress Syndrome in COVID-19". TP47. TP047 COVID AND ARDS CASE REPORTS. doi:10.1164/AJRCCM-CONFERENCE.2021.203.1_MEETINGABSTRACTS.A2430.

