User:181kotj/sandbox
| 181kotj/sandbox | |
|---|---|
| Other names | Bilateral perisylvian polymicrogyria |
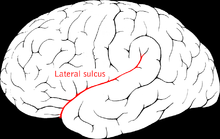 | |
| Lateral sulcus (Sylvian fissure) | |
| Specialty | Neurology |
Perisylvian syndrome is a rare neurological disease characterized by damage to the sylvian fissure (lateral sulcus), an area in the brain involved in language and speech. The main symptoms are difficulty chewing and swallowing, low muscle tone in the face and tongue, speech and language development disorders, and epilepsy. These symptoms are also often accompanied by difficulties with mobility and intellectual disabilities.[1]
Researchers have expressed difficulty in understanding the exact underlying cause of this condition. Many articles postulate several sources for causes, such as stroke and external trauma to the head, causing damage to the fissure and resulting in malfunctioning structures that interact with it. Interestingly, it has become and increasing focus due to the significant anatomical structures that cross it.
Signs and Symptoms
[edit]Because of the relationships the fissure has with multiple vital parts of the brain, damage to any one of them can alter the function of the adjacent cortical regions, disrupting the connection between the cognitive, neural, and muscular network.
It is unclear if these are specific to long term or short term in duration, but symptoms are implied to be permanent without medical intervention.

Speech:
[edit]Trauma to the fissure near the temporal lobe can cause speech issues. Wernickes area is located on the temporal gyrus next to the caudal end of the Sylvian fissure. This area is part of the language system, and majorly functions in the ability to recall speech sounds associated with written letters. Damage to this area can cause Anomia, and Phonemic Paraphasia. [2]
As well, the sylvian surface on the frontal lobe, located deep in the sylvian fissure, contains a bundle of fibers called the arcuate fasciculus (AF) that arches around the fissure, and comes from Brocas area, which is involved in language production and comprehension. Damage to this nerve bundle can cause conditions such as Brocas Aphasia and Expressive Aphasia[2].
Auditory Processing Disorders:
[edit]Damage to the fissure near the temporal lobe may also cause auditory processing disorders[2].
Epilepsy
[edit]Epilepsy is common in studies related to congenital, bilateral, and unilateral Perisylvian syndrome. Kuzniecky et all. Reported 90% of cases with epilepsy. [3]

Facial paralysis
[edit]While the Sylvian fissure does not directly connect to the cranial nerves, previous exploratory dissection reveals that the middle cerebral artery (specifically the M2 segment) runs through the deep insular tissue. Damage to the Sylvian tissue may cause damage or malfunction to the arterial supply of the M2 and create an infarction resulting in hemiparesis (unilateral paralysis).[2] . Mavili E et all. Study found that 89% of patients were present with mental-motor retardation, 84% with speech disorders, and 57% with cerebral palsy [3].
Cause and Prevention
[edit]There are many unrelated pre-occuring conditions and risk factors that lead to the following causes of Perisylvian syndrome. Though the definitive cause is still being explored, it has been well defined that the condition cannot be spread from person to person. One study proposes several of the following causes that may create trauma to the fissure[3]:
- Cerebral hypoperfusion- a condition where there is inadequate blood flow to the brain, and can be caused by smoking, blood pressure disorders, stroke, and sepsis[4]
- Stroke - A condition where blood flow to the brain is disrupted, causing brain cells to die off[5]
- Possible injury during neuronal migration in fetal development
- Brain lesions - An area of damaged brain tissues from injury or disease[6]
In the majority of cases however, the condition appears sporadically[2].
Cysts
[edit]Arachnoid cysts represent <1% of intracranial lesions, with the Sylvian fissure being the most common location, most predominant in males on the left side.
Cysts are often discovered incidentally during imaging, and most common associated symptoms are headaches, seizures, and motor deficit due to the pressure the cyst applies to the temporal lobe[2].
Pathophysiology and Mechanism
[edit]The Sylvian fissure is the most prominent crease on the brain. It sits on the lateral hemisphere of the brain, separating the temporal and frontal lobe. It extends into the parietal lobe, and sits perpendicular to the central sulcus, a prominent groove on top of the brain. It also sits in the insula, a part of the brain involved in various functions such as decision making, social emotions, empathy, pain processing, interception, auditory processing. The site is also closely associated with a major cranial artery known as the middle cerebral artery, a vital and the largest branch of the internal carotid artery that is responsible for blood supply to the brains frontal, temporal, and parietal lobes. It is made up of 4 branches labeled as M1, M2, M3, and M4.
In most cases of Perisylvian syndrome, the condition exists congenitally and is not typically developed throughout one’s lifetime without some sort of significant trauma to the head, causing lesions, pressure, or tissue death, and trickles down to the rest of neural processing in other vital functions of the brain. Once neural processes weaken in these areas, the brain is not able to send signals to its respective parts of the body.
Diagnosis
[edit]A neurologist would be seen if a diagnosis is desired. Considerning the symptoms, a diagnosis may be confirmed with the following:
CT scan
[edit]Early signs of the middle cerebral artery occlusion can be found upon discovery of a hyperdense MCA: it appears with increased attenuation of the M1 segment, or with hyperdensity in the distal MCA & branches inside the Sylvian fissure[2].
Brain MRI
[edit]Appearance of ‘bat wings’ – bilateral open fissure typically seen in type 1 Glutaric aciduria[2]
Angiography
[edit]The Sylvian triangle is an important landmark on lateral cerebral angiograms. It is made up of 3 lines; one if a straight line that follows the insular loops of the M2 segment, a large trunk of the MCA anterior, and the first ascending insular branch of the M2 segment posterior[2].
History of Aneurysms:
[edit]Bifurcation of trifurcation of the M1 segment, located in the Sylvian fissure sphenoidal compartment, may arise intracranial saccular aneurysms from the MCA. (Occurs in 22% of people)[2].
Treatment and Prognosis
[edit]Data in prognosis is very limited for this syndrome. However, neurological conditions affecting multiple parts of the brain have had a wide range of recovery timelines. However, there have been many invasive surgical interventions to improve symptoms.
Aneurysms
[edit]Transluminal embolization techniques, microsurgical techniques, hybrid techniques[2].
Inside-out dissection:
[edit]General principle for surgery. Patient lays in supine position with the head rotated away at 30%. There are 3 spaces to consider with different challenges for each.
In the superficial ocular compartment, the best point to begin is at the anterior sylvian point, below the pars traignularis of the inferior frontal lobe. Then a sharp incision of the outer arachnoid membrane, always on frontal side of superficial Sylvian veins. Then a gentle displacement of superficial veins to temporal lobe, and finally dissection of arachnoid bands that connect brain-brain and vein-vein, exposing the lateral Sylvian membrane[2].
In the deep opercular compartment, begin with dissection of lateral slvian membrane to expose the compartment, then dissection of deep arachnoid bands, mainly brain-brain and artery-brain[2].
Lastly, in the Cisternal compartment, the M2 segment must be identified, deeply seated on lateral insular surface[2].
Cysts
[edit]Treatment & management include conservative & surgical alternatives (endoscopic, microsurgical craniotomy, shunting. Neuroendoscopic fenestration is best initial procedure for middle cranial fossa arachnoid cysts)[2].
Medication:
[edit]While medication cannot treat the condition, it may treat some associated symptoms:
One woman with bilateral Perisylvian Syndrome was treated for her epilepsy with lamotrigine and oxcarbazepine and was in remission for 8 years. When reappeared, treatment included LTG and levetiracetam, and resulted in significant clinical improvement[3].
Recent Research
[edit]In 2017, a study conducted by Freri et all. A new surgical treatment was explored to improve symptoms of epilepsy in the perisylvian region for 16 pediatric patients who were resistant to medication, the median age during time of surgery was 12 years old. Prior to the procedure, patients completed a preoperative assessment including analysis of clinical history, EEG monitoring, High-resolution MRI, and a cognitive/neuropsychological evaluation. The procedure was preformed with the goal of removing the epileptogenic zone. It was found post-operatively (39 months) that seizure outcome improved satisfactory in 69% of patients, with 7 being seizure-free, and two were free from disabling seizures. Cognition improved in 38% of patients as well[7].
References
[edit]- ^ "Perisylvian syndrome". www.socialstyrelsen.se. Retrieved 2015-08-13.
- ^ a b c d e f g h i j k l m n o Alvarez Toledo N, Munakomi S, Prestigiacomo CJ. Neuroanatomy, Sylvian Fissure. [Updated 2023 Aug 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK574552/
- ^ a b c d Mameniškienė, R., et al. "Bilateral Perisylvian Syndrome With Autonomic Seizures and Autonomic Status Epilepticus: A Case Report With Long-Term Follow-up." Neurologijos seminarai 18.3 (2014).
- ^ Ciacciarelli A, Sette G, Giubilei F, Orzi F. Chronic cerebral hypoperfusion: An undefined, relevant entity. J Clin Neurosci. 2020 Mar;73:8-12. doi: 10.1016/j.jocn.2020.01.026. Epub 2020 Jan 14. PMID: 31948882.
- ^ Stephen JX. Murphy, David J. Werring, Stroke: causes and clinical features, Medicine, Volume 48, Issue 9, 2020, Pages 561-566, ISSN 1357-3039, https://doi.org/10.1016/j.mpmed.2020.06.002.(https://www.sciencedirect.com/science/article/pii/S1357303920301389)
- ^ Singh A, Kate MP, Nair MD, Kesavadas C, Kapilamoorthy TR. Bilateral perisylvian infarct: a rare cause and a rare occurrence. Singapore Med J. 2011 Apr;52(4):e62-5. PMID: 21552775.
- ^ Fereri, E., Matricardi, S., Gozzo, F., Cossu, M., Granata, T., & Tassi, L. (2017, June 23). Perisylvian, including insular, childhood epilepsy: Presurgical workup and surgical outcome. online library.wiley.com. https://onlinelibrary.wiley.com/doi/10.1111/epi.13816

