Talk:Hepatorenal syndrome
 | Hepatorenal syndrome is a featured article; it (or a previous version of it) has been identified as one of the best articles produced by the Wikipedia community. Even so, if you can update or improve it, please do so. | |||||||||||||||
| This article appeared on Wikipedia's Main Page as Today's featured article on November 29, 2009. | ||||||||||||||||
| ||||||||||||||||
| Current status: Featured article | ||||||||||||||||
| This article is rated FA-class on Wikipedia's content assessment scale. It is of interest to the following WikiProjects: | |||||||||||||||||
| |||||||||||||||||
Pathophysiology accuracy?
[edit]The article cited in reference 9 states that subjects in group B, those with acites and functional renal failure, have decreased renal and femoral cardiac output fractions, in contrast to what is written in the pathophys section of this article. What is the basis for this discrepency? —Preceding unsigned comment added by 130.91.98.31 (talk) 03:57, 22 June 2008 (UTC)
prognosis
[edit]I reverted 'slightly' to the 'slightly better prognosis' with HRS2, as the prognosis is still ghastly, whether or not they on average last for another few months. I think it's important to bear in mind that patients and relatives will read these articles when they or their loved ones are sick-and we should avoid giving falsely positive impressions of the outcome of this disorder, of which I cannot think of one good outcome in all the cases I've seen professionally over the last ten years.Felix-felix 07:17, 24 July 2006 (UTC)
- I disagree on the word "slightly" for one reason: It's agreed that prognosis is poor with Type II HRS (<6/12) but, this data is almost all from the pre-liver transplant era. Practically, the difference now is the time to transplant, which is the major determinant to long term prognosis. The prognostic figures on T1 and T2 HRS commonly cited are from the Barcelona series (PMID 8514039) published in 1993, which was also presented in graph schematic form in their Lancet review (PMID 14654322 -- the same graph is copied in most reviews on HRS since). Some of this was done in the era pre-OLTx, and almost all was before the availability of LRDLTx.
- Type I HRS patients are so ill that, especially in organ-deficient areas, a large percentage still don't make it to transplant (even when dialysis supported). Type II HRS patients, on the other hand, do have time to make it. At my centre, in the past five years we've transplanted at least 40 patients on an accelerated basis with type II HRS (diuretic resistant ascites and renal failure). In practical terms in my area, T2 HRS results in admission to hospital, and a higher priority for transplantation, which, now, is becoming feasible. -- Samir धर्म 09:25, 24 July 2006 (UTC)
- You guys are obviously alot more proactive than our liver boys! We normally get suckered into dialysing the 'type 2 HRS' patients on the understanding that they'll be transplanted and get left holding the can when 8 weeks down the line, we're told they're not suitable for transplantation at all! Anyway-ammended edit to try and encompass the 'they'll die if they're not transplanted' angle. See what you think.Felix-felix 10:00, 24 July 2006 (UTC)
- Looks good! An apt synopsis -- Samir धर्म 12:19, 24 July 2006 (UTC)
- You guys are obviously alot more proactive than our liver boys! We normally get suckered into dialysing the 'type 2 HRS' patients on the understanding that they'll be transplanted and get left holding the can when 8 weeks down the line, we're told they're not suitable for transplantation at all! Anyway-ammended edit to try and encompass the 'they'll die if they're not transplanted' angle. See what you think.Felix-felix 10:00, 24 July 2006 (UTC)
Good Article
[edit]This was definately clear, well-referenced, and approachable from someone like me, who doesn't know anything about the subject. Great work! Dlmccaslin 18:24, 11 August 2006 (UTC)
Hepatorenal failure
[edit]I haven't heard hepatorenal syndrome referred to as hepatorenal failure. eMedicine does not give hepatorenal failure as a synonym[1] nor does Stedman's medical dictionary.[2] Hepatorenal failure is not a precise term for the condition -- and the following ref. suggests it is not used, as hepatic and renal failure can occur simulateously for a number of different reasons. Davison AM. Hepatorenal failure. Nephrol Dial Transplant. 1996;11 Suppl 8:24-31. Review. PMID 9044337 Nephron T|C 19:31, 9 September 2006 (UTC)
- Agreed. Hepatorenal syndrome is a distinct definition -- Samir धर्म 01:28, 10 September 2006 (UTC)
Quote
[edit]I removed the quote. {diff} I liked it-- but could not find a reference for it. (Wikipedia:Verifiability) The user that added it has since posted nothing --see Special:Contributions/Rajat666 and did not respond to my request to reference it -- see User talk:Rajat666. Nephron T|C 22:50, 19 December 2006 (UTC)
- "The liver and kidney are the greatest of lovers.When the liver is diseased the kidney weeps" - Dr (Col)S.Krishnan, M.D.(Pune),D.M.(Chandigarh),Apollo Hospitals,Chennai,India"
- Except of course, that when the kidneys are diseased, the liver doesn't return their calls...Felix-felix 10:03, 20 December 2006 (UTC)
- "The liver and kidney are the greatest of lovers.When the liver is diseased the kidney weeps" - Dr (Col)S.Krishnan, M.D.(Pune),D.M.(Chandigarh),Apollo Hospitals,Chennai,India"
Trials
[edit]The trials are lousy[3]. JFW | T@lk 20:13, 6 March 2007 (UTC)
- So's the prognosis, my friend, unfortunately with or without therapy -- Samir 06:44, 26 May 2007 (UTC)
I know, Samir, which is why we need to enrol every patient in a trial, and preferably in a trial that has adequate power, good outcome measures and generalisability (?word exists). JFW | T@lk 22:34, 2 July 2007 (UTC)
The final section on prevention suggests the prophylactic use of iv albumin to reduce the risk of progression to hepatorenal failure. This is not common practice despite the fact that the quoted study has been in the public sphere for at least the last 10 years. This study was limited to patients with bacterial peritonitis and it had a number of serious flaws. The article as it currently stands would suggest that this therapy is useful in all patients who may potentially develop HRS and not just this subset. I would suggest that this section be deleted entirely or modified to point out that only a small percentage of patients may be suitable for this treatment. gearoidmm (talk) 22:28, 5 January 2009 (UTC)
GA status
[edit]- does not fulfill WP:LEAD
- no images
- The section on history is limited. When did the first case occur.
- How common is this condition?
- What are the causes?
--Doc James (talk · contribs · email) 01:32, 21 May 2009 (UTC)
See the community reassessment page for further discussion.
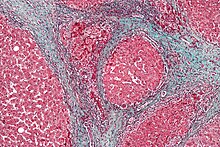
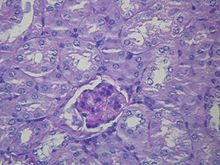
article image
[edit]Hello,
Regarding the two images in the infobox: Are these images even at the same scale? What is the scale of this image? -- It looks like it was taken via an optical microscope, and either the colour balance of one of the images is wrong, or they have used a different preparation method -- why is it a different colour? Are the two cross sections comparable? Are livers even isotropic, do we need to quote a direction of the cross-section. It concerns me that we have just picked some images straight out of Flickr, rather than from a more reputable public source, like PLoS, or the CDC. User A1 (talk) 01:27, 29 November 2009 (UTC)
- Given that two different "stains" have been used, is it right to compare them in this manner? User A1 (talk) 01:31, 29 November 2009 (UTC)
- I'm a bit concerned that for a featured article, this concern has not been addressed. I am not an expert on this particular subject, but it seems to me that the image is not a rational comparison -- two different preparation methods are used and we don't even know if the images are at the same scale, are the same thickness or the same orientation of cut. User A1 (talk) 12:32, 29 November 2009 (UTC)
- Same concern. What is the reason for selecting these two images to join? Are they even from the same species? They're just two random micrographs, at low resolution, without scales, joined to demonstrate... What? What the two different stains indicate? Do they highlight particular molecules or structures or what? Are they the same species? --IP69.226.103.13 (talk) 19:53, 29 November 2009 (UTC)
- The image is meant to be conceptual to depict normal kidney histology in the context of altered hepatic pathology. I think it is highly useful conceptually -- Samir 23:38, 29 November 2009 (UTC)
- Same concern. What is the reason for selecting these two images to join? Are they even from the same species? They're just two random micrographs, at low resolution, without scales, joined to demonstrate... What? What the two different stains indicate? Do they highlight particular molecules or structures or what? Are they the same species? --IP69.226.103.13 (talk) 19:53, 29 November 2009 (UTC)
I removed the image. It doesn't make sense. It's original research. No one can explain it. --69.226.100.7 (talk) 23:15, 29 November 2009 (UTC)
- The top image is an H&E stain of liver showing alcoholic cirrhosis which is a common cause of hepatorenal syndrome. It shows classic changes of alcoholic cirrhosis (steatosis and Mallory's hyaline, and fibrous septae, which admittedly would be better with a trichrome stain) and is a fine image. The second is an image of a normal kidney glomerulus at fairly high magnification. The combined image is useful conceptually to understanding HRS as it depicts that renal histology is normal in this syndrome and that the pathology is found in the liver. I have reverted the removal. -- Samir 23:37, 29 November 2009 (UTC)
- What about all these other questions people have asked about the image? "Fairly high?" What? How do you know? Is the liver low magnification? What species are they? Are they human? I guess you know what species, so what species is it? Why not just say, "Pathological Liver" and "Normal Kidney," then caption them as indicating a normal kidney is a typical finding with hepatorenal syndrome, and the glomerulus is the section of the kidney used for medical diagnoses during biopsy or anything that explains why two images from two different sites, both emphasizing the staining for light microscopy without explanation as to why the staining matters, particularly when you're showing a normal kidney stained with a common liver stain, are juxtaposed? It's still original research on your part and doesn't support an otherwise well-written article. I ask you to remove them. They don't belong, you've emphasized the wrong things, you've inappropriately juxtaposed two unrelated images. --69.226.100.7 (talk) 23:47, 29 November 2009 (UTC)
- Agreed that the caption needs clarification but the image is very useful to the article in my opinion. Let me try re-writing it -- Samir 23:52, 29 November 2009 (UTC)
- I've re-written the caption and when the image is unprotected on Commons, I can add to the description that both images are from humans, although it is unnecessary for the caption as the entire article is about human illness. The idea for the composite image came from
Sleisenger and Fordtran(in error, I just checked; I must have gotten the idea from either another book or a review article) where a similar image is used in their hepatorenal syndrome chapter (side by side as opposed to top to bottom, also two images from different pages). -- Samir 00:03, 30 November 2009 (UTC)
- I've re-written the caption and when the image is unprotected on Commons, I can add to the description that both images are from humans, although it is unnecessary for the caption as the entire article is about human illness. The idea for the composite image came from
- Agreed that the caption needs clarification but the image is very useful to the article in my opinion. Let me try re-writing it -- Samir 23:52, 29 November 2009 (UTC)
- What about all these other questions people have asked about the image? "Fairly high?" What? How do you know? Is the liver low magnification? What species are they? Are they human? I guess you know what species, so what species is it? Why not just say, "Pathological Liver" and "Normal Kidney," then caption them as indicating a normal kidney is a typical finding with hepatorenal syndrome, and the glomerulus is the section of the kidney used for medical diagnoses during biopsy or anything that explains why two images from two different sites, both emphasizing the staining for light microscopy without explanation as to why the staining matters, particularly when you're showing a normal kidney stained with a common liver stain, are juxtaposed? It's still original research on your part and doesn't support an otherwise well-written article. I ask you to remove them. They don't belong, you've emphasized the wrong things, you've inappropriately juxtaposed two unrelated images. --69.226.100.7 (talk) 23:47, 29 November 2009 (UTC)
outdent : My recommendation is that we scour PLoS for a suitable image. The concern is that the images are unverifiable, and that in general synthesis from Flickr microscope images is not a good idea. User A1 (talk) 00:11, 30 November 2009 (UTC)
- PLoS is a good idea or I can ask our pathologists to scrounge up some photomicrographs if it is that much of a concern. User:Nephron is also an exceptional resource and I can ping him. I don't see how this qualifies as Wikipedia:Synthesis though as there is no original research involved here. The reason I chose those pictures is because they happen to be a brilliant free image of alcoholic cirrhosis and a fantastic free image of a glomerulus. Together they illustrate the most common pathology of HRS (i.e. alcoholic cirrhosis/normal kidney) perfectly. -- Samir 00:18, 30 November 2009 (UTC)
- PLoS would be a good idea. Also, the caption needs to de-emphasize the stains. The stains are not particularly relevant for the image caption for this image in this article, and, in fact, it adds confusing information--please just delete them. As they are, wikilinked and all, they are emphasizing the different stains, and, because the kidney is stained with a common liver stain, the first thought is that there is some additional thing about these images. Please just delete the stain information. Yes, synthesis of Flikr images is a bad idea, particularly if you're working with micrographs and you're neither a microscopist nor a pathologist. --69.226.100.7 (talk) 00:39, 30 November 2009 (UTC)
- Adding the stain information to the caption was suggested in WP:FAC but I agree with removing it entirely or de-emphasizing it. Also PAS is not a "common liver stain". -- Samir 01:08, 3 December 2009 (UTC)
- PLoS would be a good idea. Also, the caption needs to de-emphasize the stains. The stains are not particularly relevant for the image caption for this image in this article, and, in fact, it adds confusing information--please just delete them. As they are, wikilinked and all, they are emphasizing the different stains, and, because the kidney is stained with a common liver stain, the first thought is that there is some additional thing about these images. Please just delete the stain information. Yes, synthesis of Flikr images is a bad idea, particularly if you're working with micrographs and you're neither a microscopist nor a pathologist. --69.226.100.7 (talk) 00:39, 30 November 2009 (UTC)
- I also recommend that the image be removed until we sort this out; though I think it would be polite if one of the more active page editors were to do this. User A1 (talk) 02:10, 30 November 2009 (UTC)
- I think removing it is a bad idea. It conveys excellent graphical conceptual information regarding hepatorenal syndrome. It shows the pathology of alcoholic cirrhosis and normal renal histology and shows this very well. This is the crux of the condition. The caption needs to be changed, but it is an excellent addition to the article IMO -- Samir 01:08, 3 December 2009 (UTC)
- Maybe we could use these two images instead? They are not as nice as the Flickr ones IMO but they were added by User:Nephron and User:Arcadian respectively, who are long term contributors to medical content here, and who can comment on details of staining/magnification, etc. My preference is still the image as is
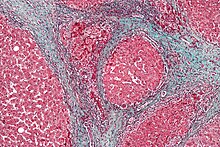
Trichrome stain of cirrhosis PAS stain of kidney
-- Samir 01:25, 3 December 2009 (UTC)
I'm afraid I have to agree that the combined image is way too confusing: to the typical Wikipedia reader it conveys the mistaken impression that the image compares normal and diseased tissue of the same type. I replaced it with the two images suggested above. I'm no expert in the area, so please check my caption and alt text. Eubulides (talk) 19:22, 18 December 2009 (UTC)
When both the caption and the images clearly indicate that the tissue types are different, kindly explain why is this confusing? This however is a reasonable compromise -- Samir 05:56, 21 December 2009 (UTC)
Predictors of response
[edit]doi:10.1002/hep.23283 - higher bilirubin and poorer BP response to albumin + terlipressin predicts treatment failure. JFW | T@lk 14:03, 25 December 2009 (UTC)
All change
[edit]An international committee has met to try to align the definitions of HRS with the new AKI classification for acute kidney injury. The result is this document: doi:10.1136/gut.2010.236133. It will probably need mentioning, especially if this becomes widely used. JFW | T@lk 11:04, 4 April 2011 (UTC)
- I hadn't seen doi:10.1186/cc11188, a new ADQI consensus document on HRS. This needs to be mentioned. Particularly interesting is the paucity of good evidence, and the advice to withhold RRT if someone with HRS is not a transplant candidate. JFW | T@lk 13:23, 29 October 2012 (UTC)
TIPS(S) and encephalopathy
[edit]"Complications of TIPS for treatment of HRS include the worsening of hepatic encephalopathy (as the procedure involves the forced creation of a porto-systemic shunt, effectively bypassing the ability of the liver to clear toxins)"
- I think there's no question that TIPS can worsen encephalopathy, but there is no support in the literature for the mechanism implied parenthetically here, that the liver's failure to 'clear' 'toxins' results in encephalopathy. What toxin is that? By what mechanism does the liver 'clear' it? How does TIPS result in a failure of this mechanism? Researchers, myself among them - sacrificed dozens of portal-shunted rats, ill-tempered bastards all - have been investigating these questions for 50+ years and there is no consensus about the answers; most of us feel that there is in fact no endogenous toxin responsible for HE. The cited references are careful not to claim any such mechanism, by the way. 99.127.139.233 (talk) 18:07, 7 August 2011 (UTC)
- Many clinical papers seem to accept the ammonia hypothesis as fact, and indeed there is good basic scientific data on radiolabeled ammonia concentrating in the brain. Bypassing the liver (and thus the urea cycle enzymes) does certainly seem to be the mechanism of HE following iatrogenic shunting. JFW | T@lk 13:31, 29 October 2012 (UTC)
- Wikipedia featured articles
- Featured articles that have appeared on the main page
- Featured articles that have appeared on the main page once
- FA-Class medicine articles
- Mid-importance medicine articles
- FA-Class gastroenterology articles
- Mid-importance gastroenterology articles
- Gastroenterology task force articles
- FA-Class nephrology articles
- Mid-importance nephrology articles
- Nephrology task force articles
- All WikiProject Medicine pages