Talk:Amphetamine/Archive 4
| This is an archive of past discussions about Amphetamine. Do not edit the contents of this page. If you wish to start a new discussion or revive an old one, please do so on the current talk page. |
| Archive 1 | Archive 2 | Archive 3 | Archive 4 | Archive 5 | Archive 6 | → | Archive 9 |
Added new pharmacokinetics content w/ metabolism content
Boghog (talk · contribs), if you're familiar with this synthesis/metabolism material, the content I just added could probably use copy-editing from a more chemistry-savvy editor than I am. I actually wasn't sure if some of the pathway-related enzymatic reactions were redundant. A lot of that content was bits and pieces from the pubchem compound page. Regards, Seppi333 (talk) 05:39, 12 October 2013 (UTC)
- Boghog, I added another synthesis route - I'd really appreciate it if you could edit it for style/accuracy again. I also added the quote from the source in a censored comment beneath the synthesis section for reference. Regards, Seppi333 (talk) 00:30, 20 October 2013 (UTC)
- I have added a bit more detail to the third synthetic route. (I am restraining myself not to add too much detail ;-) ) I also note that the reaction scheme (File:Amphetamine - Leuckart reaction.png) contains a minor error (the source contains the same error). The second structure should be formamide but what is drawn is acetamide. This can be fixed by adding a "H" symbol to the end of the stick. You are doing a fantastic job by the way in moving this article towards FA status :-) Boghog (talk) 12:19, 20 October 2013 (UTC)
- Thanks! I'll update/fix the image file as soon as I get a chance - likely sometime tomorrow night. Seppi333 (talk) 00:02, 21 October 2013 (UTC)
- I have added a bit more detail to the third synthetic route. (I am restraining myself not to add too much detail ;-) ) I also note that the reaction scheme (File:Amphetamine - Leuckart reaction.png) contains a minor error (the source contains the same error). The second structure should be formamide but what is drawn is acetamide. This can be fixed by adding a "H" symbol to the end of the stick. You are doing a fantastic job by the way in moving this article towards FA status :-) Boghog (talk) 12:19, 20 October 2013 (UTC)
(Outdent)
Sorry for the late follow up - been really busy outside of Wikipedia. I fixed the image, so let me know if it's good or there's still any flaws or potential improvements (no matter how small). Feel free to add whatever you want though - the more (on-topic/relevant) info, the more comprehensive, and hence the better the article. ![]() Also, I need to do the following two things for GA/FA improvements, but as I have no background in chem, it'd be a big help if you could review the content after I add it.
Also, I need to do the following two things for GA/FA improvements, but as I have no background in chem, it'd be a big help if you could review the content after I add it.
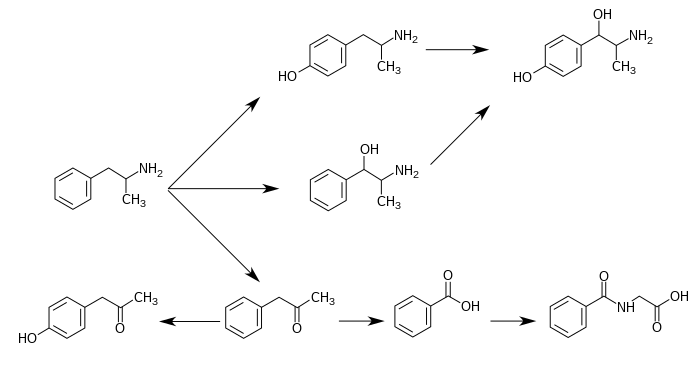
- for FA I'd expect to see a figure showing the chemical structures of metabolic intermediates in the detox pathways
- "so chromatographic methods specific for amphetamine are employed to prevent false positive results." more details please; same for "Chiral-separation techniques may be employed to help distinguish the source of the drug.
Regards, Seppi333 (talk) 16:32, 22 October 2013 (UTC)
- I am also quite busy outside of Wikipedia at the moment. I should have some time this weekend to take a more careful look at the chemistry including the chromatography. I am also working on a graphic that outlines the metabolic pathways. Cheers. Boghog (talk) 17:32, 22 October 2013 (UTC)
- I don't know if you have access to a university or institutional research database, so I'm just going to link these files directly for you to download, since you could probably use them more than I could. The first file is PMID 12191709, the second one is PMID 14871155, and the third is a metabolic pathway including 4-hydroxyphenylacetone + other new stuff from the first paper (neither paper is free).
- I've more or less given up on trying to figure out a complete pathway, because so far as I can tell, "alpha-hydroxy-amphetamine" doesn't exist in any database. Pubchem also links phenylisopropanol to 2-phenyl-2-propanol, but several papers on amph that mention it use it synonymously 1-phenyl-2-propanol. Not really sure why that is, but given my inability to find the metabolites I'm looking for and knack for finding more metabolites that I'm not, I'm going to stop before I'm anymore behind, hehe. Seppi333 (talk) 02:26, 24 October 2013 (UTC)
How's this look in the meantime? It's the best I could do with my limited knowledge of chemistry and chem editors (I actually used MS paint to make some of these). ;P
Seppi333 (talk) 21:34, 24 October 2013 (UTC)
I hate to ask even more of you since I feel like you've already done a lot for me, but if you're willing and have a chance (this isn't even remotely urgent, so no rush), these three article I made could use a quick, cursory stupidity-filter/fact-check: P-hydroxynorephedrine, formetamide, and User:Seppi333/P-hydroxyphenylacetone. Regards, Seppi333 (talk) 17:05, 28 October 2013 (UTC)
Vaporization route removal
Hi everyone - I'm not 100% positive this is the same thing, so revert my edit if vaporization is a more general concept or "route" than smoking.
I came across this page from the EMC stating that, unlike meth, amphetamine (sulfate form) is insufficiently volatile to be smoked. http://www.emcdda.europa.eu/publications/drug-profiles/amphetamine
Regards, Seppi333 (talk) 02:43, 15 October 2013 (UTC)
Amphetamine and Monoamine Oxidase
From the research I've done, and from prior knowledge, it would appear to me that Amphetamine's metabolism is almost entirely mediated by MAO-B. If that's the case, why shouldn't it be noted in the metabolism section on the right, that MAO-B plays a big part in Amphetamine metabolism? I know CYP2D9 does have some effect on amphetamine, however, the studies I've read claim that it's effects on Amphetamine metabolism is <10%.
So, before I add this into the article, am I missing something? It seems to me that this should already be here and the fact it isn't leads me to believe I may be misinterpreting something.
Regards SwampFox556 (talk) 20:06, 15 October 2013 (UTC)
- Its effects on MAO are pretty minor in comparison to methamphetamine, so that was added as 1 sentence in the pharmacodynamics section.
- For cytochrome P450 enzymes - I did a lot of searching for existing literature reviews in humans, but all I found was cyp2d6 and FMO enzymes. There's a lot of literature on nonhuman animals, but that's not necessarily representative of human metabolism. If you know of a review that mentions other enzymes in humans, it would be great if you could add it. Seppi333 (talk) 03:28, 16 October 2013 (UTC)
Detection in body fluids
This section could use a general range of how long amphetamine is detectable by a typical test. That's a significant piece of information, and I'm sure many people come here looking for it. Exercisephys (talk) 21:52, 25 October 2013 (UTC)
- I can try to look into that, but given my lack of familiarity with different methods of mass-spec and immunoassay, I'm not sure I understand the concepts enough to be able to figure out what an average test is. Nonetheless, I don't think it would necessarily matter, since amphetamine elimintion varies with respect to time after intake (moderate influence), urine pH (by far the strongest influence), and tolerance (moderate influence). Consequently, the detectibility in urine after intake, given a minimum detectability threshold for a test, would be a stochastic process, or highly variable, even for the same person over time. I will look anyway though. Regards, Seppi333 (talk) 06:27, 26 October 2013 (UTC)
Semicolons
This article contains a lot of examples of long sentences being combined with semicolons. I would make the article more readable to leave them as separate sentences.
- I don't understand the issue with this. Semicolons are used analogously to a full stop when two sentences are closely related. Seppi333 (talk) 20:22, 26 October 2013 (UTC)
- It's not a big deal, it's just a readability thing. Having two really long sentences, each with three or more clauses, enjambed reduces readability even if it isn't grammatically incorrect; readability is an important facet of an effective Wikipedia page, especially when you consider that readers have varying aptitudes, and that many of them have limited attention spans (especially those viewing an article about amphetamine ;D). Because of this, most style manuals suggest using them sparingly. In some cases, though, they're a good idea. Exercisephys (talk) 02:38, 29 October 2013 (UTC)
- That's a very good point. I'll go through and edit the sentence structure today to make it a simpler read. Seppi333 (talk) 18:21, 29 October 2013 (UTC)
Effects on adolescents
A study conducted soon before the cited Volkow study, which used similar methods, came to the opposite conclusion. The Volkow paper cites it. I don't have time to dig it up now, but I think in the spirit of neutrality it deserves a mention. I posted this here as a self-reminder, and as an offer to any WP:Gnomes that have a little free time. Thanks. Exercisephys (talk) 02:33, 29 October 2013 (UTC)
- I'll see if I can find a review that includes both papers. Thanks for bringing that up. Regards, Seppi333 (talk) 18:20, 29 October 2013 (UTC)
Adderall vs. amphetamine mixed salts
A few months ago, I got Adderall moved to amphetamine mixed salts (medication). This was done because it is Wikipedia policy to name articles after the generic pharmaceutical name of drugs rather than the brand name. The fact that Adderall was one of the few lasting exceptions to this rule points out just how entrenched the brand name is. However, identical generic formulations exist, so the name "amphetamine mixed salts" should be used. However, it's probably a good idea for us to clarify that it's equivalent to Adderall often, as most people are only familiar with the latter term. Exercisephys (talk) 00:44, 3 November 2013 (UTC)
- That's more or less why I've been using the piped wikilinks to adderall in the article. I really don't think readers of this article who are unfamiliar with that page name would know "amphetamine mixed salts" is about "adderall" when they read the term. It's basically the only drug I know of that has no INN or USAN. Every pharmacy seems to have it's own name for it. Seppi333 (talk) 01:01, 3 November 2013 (UTC)
- I agree, there isn't an easy solution. I just think that using the generic name (with the additional mention of Adderall) is necessary for factual accuracy and because we'd otherwise be supporting Teva and Barr's informational monopoly.
Also, as a minor side-note, "Adderall" is capitalized. Exercisephys (talk) 16:55, 3 November 2013 (UTC)
- I'm not really sure what you mean by informational monopoly in relation to a drug name. Amphetamine and Adderall are basically just analogous to tissue and Kleenex.I feel the urge to point out that both MEDMOS and PHARMMOS indicate that this page should be renamed "amfetamine" but that's just not going to happen... Seppi333 (talk) 11:23, 5 November 2013 (UTC)
I also realized it was possible to check the number of users searching for Adderall vs using a wikilink directly to the page or searching the page itself. As of writing this, over the past 90 days, 70000 people searched for Adderall in the search bar or arrived there from outside wikipedia, since redirects to Adderall would just be moved to amph mixed salts by bots. Over that same 90 day period, 184 people arrived at "Amphetamine mixed salts" by searching that term directly or coming from outside wikipedia. The remainder of the 118000 people that viewed amphetamine mixed salts (medication) probably arrived there externally or by wikilink given that 184 (vs 70000 for Adderall) people searched the non-parenthetically disambiguated version. There's really only one conclusion to draw from those stats and the first item in WP:CRITERIA. :P Seppi333 (talk) 12:23, 5 November 2013 (UTC)
- In all of the decade that I've known I had ADHD, and that Adderall was one of the possible drugs to treat it, I have only heard of it as "amphetamine mixed salts" in a few written academic discussions, usually as a parenthetical, eg. "Adderall (brand of amphetamine mixed salts"). People (patients, parents, doctors, researchers) do talk about "generic Adderall", in that a prescription plan or pharmacy is providing something other than "real Adderall". Does Adderall even have a fixed composition, percentages of specific salts? Entirely OR, of course. htom (talk) 01:40, 6 November 2013 (UTC)
- It's listed in the Rx info as 25% amph aspartate, 25% amph sulfate, 25% d-amph sulfate, 25% d-amph saccharate. Seppi333 (talk) 05:28, 6 November 2013 (UTC)
- The definition of "amphetamine mixed salts" is circular. By regulatory definition, it has a composition that is identical to that contained in Adderall. It is one of the few drugs that is so defined. The reason why the name Adderall is so entrenched is not solely due to marketing, but in addition, this name is shorter, simpler, and more precise. Adderall has effectively become a generic name. This is a case where rules have over ruled common sense and common usage. Boghog (talk) 07:32, 6 November 2013 (UTC)
Cite web templates
Instead of replacing the "publisher" parameter with "work" parameter in citation templates as was done in this edit and removing the information that was in the work parameter, why don't we add publisher and work parameters to all cite web templates? According to the {{cite web}} documentation, the "work" parameter contains the "title of the website; may be wikilinked; will display in italics" which is clearly different than the publisher. Boghog (talk) 05:53, 4 November 2013 (UTC)
- That's probably a better way to do it in most circumstances. I just thought to combine the two because in about a quarter of the pages, either one was very hard to figure out or parameters (usually work&publisher or work&URL) were the same. Examples are the refs with an ip domain, where work and URL are redundant, the refs with a page written in another language, where publisher is harder to find. There was also a lot of mixed use of or missing work/publisher parameters in the refs.They also should both be defined if used since every source is (micro-)published and hosted on a website. I'm also not entirely sure which is the work and which is the publisher for NCBI and pubchem compound when citing the latter.
- In any event, we can do it that way if you prefer, but I'll probably need help figuring out the more ambiguous refs for consistency. :P Seppi333 (talk) 10:13, 4 November 2013 (UTC)
- URL ~ work, URL ~ publisher, and work = publisher
- Truncating the url to http://narcotic.fda.moph.go.th/ gives you the main page redirect... and I stopped there.
- IP domain
References
- ^ Hill J. "Paul Erdos, Mathematical Genius, Human (In That Order)" (PDF). Untruth.org. Retrieved 2 November 2013.
- ^ "Thailand Law" (PDF). Thailand Food and Drug Administration. Retrieved 23 May 2013.
- ^ "Clinical Drug Testing in Primary Care" (PDF). Substance Abuse and Mental Health Services Administration. Retrieved 31 October 2013.
Regards, Seppi333 (talk) 23:38, 4 November 2013 (UTC)
Adding a section about why amphetamine treats ADHD and Narcolepsy?
I think the article would be of greater benefit to the internet if it was explained why Amphetamine (but all Dopaminergic stimulants apply) are the ideal treatment for ADHD? I'd also love to see a section about why Amphetamine is used to treat Narcolepsy.
The idea for the section I have in mind would explain what we know about the causing mechanism behind ADHD and why Amphetamines are the prototypical treatment for it. I'd also love to have the ladder explained for Narcolepsy as well.
I am seriously considering putting in the amount of time it would take to research everything in depth while only explaining it in a few paragraphs. I am willing to put in the time to do that, but I'm afraid someone might object and remove the new information. So I ask...
Would that be acceptable? It would be a subsection of the "uses" header at the top of the article. Let me know what you guys think.
Best regards, SwampFox556 (talk) 00:30, 7 November 2013 (UTC)
- "Ideal treatment"? ! Well, a stimulant is one of the best treatments now known, for around 70-80% of those diagnosed (the other 30-20% don't seem to respond to any known stimulants in useful ways.) /citations needed/ Some respond well to Adderall, some well to Ritalin, some to both, and some to neither. (And there are those for whom stimulants are contraindicated who don't even get to try them.) The mechanism of ADHD (or mechanisms or ...) are still very debated. I'm sure someone will come along and claim that it's OR, too. I would love to read it. htom (talk) 00:58, 7 November 2013 (UTC)
- There's very strong evidence (as in, I haven't found a single primary source to say otherwise) in secondary sources that reduced phenethylamine metabolite in human urine is significantly correlated (statistically & clinically) with ADHD (that + heightened amphetamine response in ADHD individuals suggests that hypo-activation of TAAR1 is a causal factor in ADHD - there's several etiological factors that alone or with others can cause it; however, not all of these have been IDed). Refs are 2 TAAR1 reviews not currently in the article.
- Narcolepsy is strongly correlated with reduced orexin (not sure if A,B, or both) content in cerebrospinal fluid (the wakefulness neurpeptides). Ref for that is Westfall.
- There's multiple mechanisms for amphetamine as an obesity treatment - primarily through ghrelin (indirectly affected by amph) and cocaine and amphetamine regulated transcript (directly affected by amph), both of which directly modulate hunger/feeding behavior. (Note: I can't ref this because I haven't found any explicitly stating this in the context of treating obesity)
- Treatment for urinary incontinence is due to effects on the detrusor muscle. Westfall ref
- Potential uses in recovery from stroke or acute brain injury. More research needed for efficacy, mechanisms not understood (according to cochrane, that is - they probably are partly or completely modeled in some review). Cochrane refs.
- I'll probably add that when I get a chance sometime tomorrow night. Don't have much time before that. Seppi333 (talk) 02:53, 7 November 2013 (UTC)
The name of the study escapes me, but I read a very interesting study (that was actually a compilation of around 30 studies) that was able to make a very solid hypothesis that ADHD is caused by an over-expressed DAT1 gene. You seem pretty knowledgeable Seppi, so I'm sure you have already heard this before, however just in case you haven't...
The thesis was written up by Dr. Russell Barkley and published last year. He took many studies and formed a hypothesis from them. We have speculated for years that genes play a major part in the development of illness. However, it's incredibly difficult to understand mental illness due to the fact that we can't open up a human brain without killing that person. Anyways, my point is, we've always known that genes likely play a major role in the predisposition to developing illness, but its never been proven that one specific gene was the cause for an illness.
Dr. Russell Barkley's thesis stated this and he said that the study was start in order to attempt to determine "the genes" that cause ADHD. So he based the initial idea off of already published studies and using that information conducted other studies. His findings were quite interesting. He conducted more than one study and I'm not sure what each specific study was about to be honest, however, he summed it all up in his conclusion pretty well.
He said that they found that several things can lead to ADHD from birth, but all of these changes had to happen in the womb. However, he did mention that there was strong evidence to suggest that if a child sustains a concussion in the very early stages of after-birth development, it appeared that this could also lead to classic symptoms of ADHD.
Anyways, he said all of these things affect development in a different way but the end result is always the same.
The gene that controls the development of the Dopamine Uptake Transporters is called DAT1. It is located on chromosome 5p15. For one reason or another, this gene is mutated this causes the gene to become over-expressive thus resulting in a huge increase in Dopamine Uptake Transporters. The dopaminergic neurons release Dopamine like they should be, but the dopamine has no time to form a complex with a receptor before it gets uptaken. This results in incredibly small extracellular and postsynaptic Dopamine levels.
He found that this gene can already exist in some people and it doesn't have to be mutated. However, he found that introduction of a toxin can result in the mutation of this gene. Specifically, Nicotine and Ethanol.
Children, whose mothers drank or smoked during their pregnancy with the child, were something like 72% more likely to be born with ADHD. There is already a known correlation between ADHD and comorbidity, but he said that there was evidence to suggest that these children (children of mothers who had used a toxin at some point in their pregnancy) were even more likely to have a comorbid, psychiatric disorder diagnosed at some point in their life.
In the study, only Ethanol and Nicotine (well, all the extract of Tobacco) were used. However, both of these substances cause immense release of Dopamine through one mechanism or another. This was not said in the study, but the way he wrote it made it sound like he was alluding to this. The increased Dopamine levels causes the fetus to compensate in order to reach homeostasis. This compensation is the result of more DA transporters - either these transporters were created by the fetus as a means to get rid of extra Dopamine, or it's possible that the body could have mutated the gene so more DAT cells would be produced.
Again, he said none of that directly, but that's the idea I got from the thesis. I guess it doesn't matter how the extra uptake transporters were created, all they know is it happens. Also, I should add, they were actually able to prove this happens with extensive brain imaging. He also said that since the discovery of the over-expressed gene that causes more DA transporters to exist, many correlations between high amounts of these transporters and other illnesses have been seen.
He said that while he was conducting the rest of his thesis, another study came out (using his information) that the presence of this gene is a great indicator for later in life drug addiction. They also concluded that the substance that was most likely for the person to be addicted to at some point in their life was Nicotine. But other drugs were tested in this study and found that it also applies to Ethanol, Cocaine, and Methamphetamines. However, the study also said likelihood for addiction to dissociatives also appeared to be increased. The one tested specifically was Phencyclidine (PCP).
Anyways, to finish up Dr. Barkley's thesis - He found that the presence of this gene was a great indicator for how well you would respond to stimulant treatment. I don't remember how many people were tested (it was something like 11 or 14) but they were all tested for an over-expressed DAT1 gene - all tested positive. When they were asked to take Methylphenidate (I believe it was the minimum dose indicated for adult ADHD) they all responded very well to Methylphenidate. Attention was greatly improved, motivation was markedly improved, psychomotor agitation was markedly decreased, emotional stability was increased, impulsiveness was decreased, upon other things (those were just the one I remembered off the top of my head) and they all reported that there overall quality of life had been improved by Methylphenidate.
There are many videos of Dr. Russell Barkley explaining his finding on YouTube. One of the videos cited the thesis directly, but I can't seem to find it. Let me go back through my internet history and I'll post back.
Regards, SwampFox556 (talk) 05:56, 7 November 2013 (UTC)
- I've read research on DAT polymorphisms in a handful of papers before. I'm hesitant to cover the etiology of ADHD in the article so much as why amphetamine benefits people with ADHD. Adding the former would probably require a summary of the various ADHD articles, which at the moment aren't really up-to-date and, in my opinion, some of them had POV issues the last time I read them. In any event, TAAR1 and D2sh negatively and positively regulate dopamine transporter activity respectively (Aside: D2sh is analogous to alpha-2 adrenoceptor and 5-HT1A autoreceptors). I could probably just use that review you mentioned, or a similar one, to indicate increased DAT activity as a potential cause along with the current statement (in pharmacology) that trace amines/amphetamine activate the former receptor, but not the latter, which makes it useful as a treatment. Seppi333 (talk) 21:48, 7 November 2013 (UTC)
This is what I made reference to earlier. The paragraph is something I added a few months back and subsequently removed after becoming familiar with MEDRS:
Adhd & TAAR1
|
|---|
|
With exception to the last 2 sentences which would need to be cut, every primary source in this paragraph could be replaced with one of the following 3 reviews:[1][2][3] In individuals with ADHD, there is significant evidence that phenethylamine (PEA) – an endogenous amphetamine homologue with analogous dopaminergic pharmacodynamics[4][5] – metabolism is reduced compared to healthy individuals.[6][7][8] It is well documented that urinary excretion of PEA increases following administration of amphetamine and methylphenidate, and that urinary excretion of these drugs is highly correlated with urinary excretion of PEA;[9][10][11] moreover, studies on rodents show that brain PEA biosynthesis and metabolism greatly increases following amphetamine administration at therapeutic doses.[12][13] There is also evidence that pharmacological depletion of PEA blocks the stimulant effects of amphetamine, suggesting that endogenous PEA plays an important role in mediating the effects of amphetamines.[14][15] In spite of similar effects on catecholamines, unlike amphetamine, methamphetamine does not affect brain PEA levels, nor does PEA appear to mediate the effects of methamphetamine.[16]
References
|
- Thanks for the update cob and I like it! :) congrats on the hard work! However...
I apologies, that's not how I meant to present my point. I should have stated this above. What I meant to imply (and should have stated outright) was the fact that; whether or not it's "too many DA uptake pumps" or "too little endogenous Phenethylamine" the end result is always the same. Dopamine levels in the frontal lobe of the brain are lower than normal. This leads to all the motivational deficits, attention issues, emotional instability, etc seen in patients who have ADHD. I know there's a little more to it then just low dopamine, but that's pretty much the gist of it.
To get a little off topic, I remember reading some studies that suggested that there was a deficit in the levels of all the monoamine neurotransmitters in people with ADHD, but I'm not trying to get that far into it. Yes, I agree. Having all the above is a little overkill for just the Amphetamine article. But couldn't there be a very skimmed down version of both possible causes? Something like...
"Were not certain at this point in time what causes ADHD However, it's very widely accepted that the neurotransmitter Dopamine is found in much smaller quantities all over the Brain of someone with ADHD.(see "ADHD cause" article).
believe that genetics may play a major role in determining who will be susceptible to the illness. The gene located on chromosome 5p15, the gene itself is known as DAT1, has been identified as being responsible for the creation of the Dopamine Uptake Transporter. This transporter is responsible for removing dopamine from the synapticcleft and is an important part of dopamine regulation in the Brain. It was discovered *insert year here* that this gene appears to be overly expressed in people with ADHD. This means that many more DA transporters will be created. This would allow too much upregulation of dopamine and would result in much lower postsynaptic dopamine levels."
I didn't know how to summaries the lowered levels PEA paragraph. So in order to save time I didn't put it in in just a reply. But I'm thinking that after that paragraph is stated, that we could then briefly explain that amphetamines raise dopamine levels quite a bit?
would that be acceptable? — Preceding unsigned comment added by SwampFox556 (talk • contribs) 22:08, 8 November 2013 (UTC)
Sorry for the late reply. I think adding something like that would be fine. I'll draft something tonight and post it here to see what you think. Seppi333 (talk) 21:01, 9 November 2013 (UTC)
Actually, do you have a PMID for a MEDRS-quality review on DAT/ADHD (ideally, one published between Jan 2008 and today) handy that I can use to cite the first part? I've been a bit busy with ref editing for GA/FA to do a search for suitable papers to cite. The lack of ref on hand is really the only thing that's been holding me up from doing this. Seppi333 (talk) 20:12, 11 November 2013 (UTC)
Immense information of stimulant treatment with ADHD patients added - Controversial
It took me a couple of hours, but I finally wrote up a section on the results of stimulant treatment in people with ADHD. Even though the information provided is entirely backup, by multiple clinical studies - this section will be controversial due to the fact that there are so many misconceptions out there about stimulants drugs in the treatment of ADHD that are potentiated by the scientologists and media.
I will revert any attempted edits to the section unless claims are backed up with legitimate medical proof. I imagine this section will receive an immense amount of vandalism but I will try to monitor the section as much as I can to revert this attempt to censor information.
If anyone has any problems with the section, and can provide medical proof to backup any claims, feel free to the edit the section at will. If anyone has any problems with the section as it is now, let me know and I'll edit the section in an attempt to comply with Wikipedia's rules as best as I can.
Best regards, SwampFox56 (Zeke Ortiz)
SwampFox556 (talk) 23:30, 12 November 2013 (UTC)
- Just adding this note here in the event anyone is interested in following the thread - conversation is here User Talk:Seppi333#ADHD and stimulant section - Amphetamine
(permalink for archive: https://en.wikipedia.org/w/index.php?title=User_talk:Seppi333&oldid=581577033) Seppi333 (talk) 04:14, 14 November 2013 (UTC)
- Added comment: Exercisephys (talk · contribs) the current revision, as it stands now, omits the primate studies due to a new source explicitly stating long-term safety in humans. Figured I should notify you before the change goes live in the article. I'm working on formatting/content-merging on on this page atm. Seppi333 (talk) 04:25, 14 November 2013 (UTC)
- SwampFox556 (cc: Seppi333) The primate studies should undoubtedly stay. Please attempt to integrate previous editors' contributions instead of steamrolling everything. We just recently had to discuss that with this article. Exercisephys (talk) 17:16, 14 November 2013 (UTC)
- I do however agree that WP generally has a bias against stimulant-treatment of ADHD. I've attempted to fix that on this page to the extent my schedule allows. Exercisephys (talk) 17:18, 14 November 2013 (UTC)
- Eh, I'll reincorporate it in my revision then. Hopefully I can get this to flow well... Seppi333 (talk) 20:58, 14 November 2013 (UTC)
- Moved it to Talk:Amphetamine/sandbox so anyone can work on it - not rly fair to keep it in my sandbox. Seppi333 (talk) 21:26, 14 November 2013 (UTC)
- Exercisephys (talk · contribs) & SwampFox556 (talk · contribs) I finished reformatting, resourcing older sources, and condensing the content to merge. The finished section is at Talk:Amphetamine/sandbox#Content to replace current Uses section. If both of you could take a look and tell me if you feel satisfied with it or if it needs changes, I'd appreciate it. Seppi333 (talk) 22:10, 15 November 2013 (UTC)
I really like all of the edits. It sounds much more professional, and is better written than what I initially wrote. Thanks a lot for the work Seppi! It looks good :) There is one minor change I've decided to ahead and make though. "In particular, children with ADHD who use stimulant medications are generally more sociable." I feel like that implies that the child then becomes overly expressed socially, which isn't necessarily what the source said.
So I decided to change it to "In particular, children with ADHD who use stimulant medications, generally have better relationships with peers and family members." I also changed the sentence located after that one to "Children, also, generally perform better in school, are less distractible and impulsive, and have longer attention spans." In order to fit the above edits.
Anyways, again, everything looks great otherwise! :)
Regards,
SwampFox556 (talk) 23:10, 15 November 2013 (UTC)
- Sounds good. I'll paste it into the article then. Best, Seppi333 (talk) 00:00, 16 November 2013 (UTC)
Amphetamine increased libido?
This is rather minor but it's mentioned a couple times in the article that Amphetamine "increases libido." I'm wondering if this should rather be stated as "change in libido" as it doesn't always cause an increase? I haven't researched the topic in depth yet, however, typical prescribing information lists "change in libido" and not that amphetamine will definitely increase libido.
http://www.rxlist.com/adderall-drug/side-effects-interactions.htm
http://pi.shirecontent.com/PI/PDFs/AdderallXR_USA_ENG.PDF
A libido decrease was noted by Shire in their prescribing information of 60 milligrams of Adderall or higher.
User reports I've read also indicate that amphetamine can both "increase sexual desire" or "decrease sexual desire." I know you can't base anything off of user reports - replicated clinical studies are the only way to be sure of anything. However, it seems to me that "increase in libido" is inappropriate.
If anyone has an opposition to me changing this, I won't make any fuss about it - it's not really that big of a deal anyways. However, I feel this minor edit would make the information in the article a bit more accurate.
SwampFox556 (talk) 22:02, 16 November 2013 (UTC)
 Thank you for tweaking that. Seppi333 (talk) 02:20, 27 November 2013 (UTC)
Thank you for tweaking that. Seppi333 (talk) 02:20, 27 November 2013 (UTC)
other relevant activities section error
Apparently this page is protected so I can't edit it. Anyway, in the other relevant activities section it states that histamine is 'another monoamine' - only it isn't. It's a diamine, and as expected, it metabolized by diamine oxidase.216.105.211.130 (talk) 06:03, 26 November 2013 (UTC)
 Fixed - thanks for pointing that out! Seppi333 (talk) 13:46, 26 November 2013 (UTC)
Fixed - thanks for pointing that out! Seppi333 (talk) 13:46, 26 November 2013 (UTC)
Designated area for slapfighting about the lede
This is the current version of the article. I don't like the lede, it seems rather sloppily written and the "in spite of the significant health risks" is clearly tacked on. Not that it doesn't belong there, but the way it's included looks like the DARE van did a drive-by, so I'm going to edit it. The lede is usually the most contentious part of an article, especially one concerning a widely-abused drug, so I've gone ahead and created this section as a forum for the discussion and compromise that will probably be necessitated eventually. ZigSaw 07:28, 26 November 2013 (UTC)
- If you have a better way to write that, feel free to reword it! I doubt anyone would dispute style improvements. There are several parts of the article that, in my opinion, could use some minor wording revision. In any event, that clause was actually part of the original lead rewrite - I just couldn't think of a better encyclopedic way to say "this isn't particularly safe." Seppi333 (talk) 13:41, 26 November 2013 (UTC)
- Yeah, I put it a bit afterwards in a place where I think it fit better. It just seemed kind of shoehorned-in where it was at before ZigSaw 00:01, 27 November 2013 (UTC)
- Sounds fair enough. In general, I don't think style edits in this article spark much controversy unless they contain poor quality writing. For substantive changes, since every complete clause on the page has at least 1 citation, an edit that changes the intended meaning of a sentence would probably require adding and possibly removing references - that's often been controversial in this article. Seppi333 (talk) 02:32, 27 November 2013 (UTC)
Neurotoxicity...again
Exercisephys, I know you're well aware of WP:MEDRS criteria - stop ignoring it. Asserting neurotoxicity is a medical claim. Since this is now a GA article and I went through a great deal of trouble to remove all the non-MEDRS sources to medical claims and then re-cite the text with MEDRS versions, I'm not going to accept anything but a MEDRS source for a neurotoxicity claim. I.E., use a review of literature or professional text published within the last 5 years. Moreover, the relevant material also needs to be on humans - not animals. All of that is explicitly stated in MEDRS for medical claims on actively studied topics.
I put THREE sources to back the statement that you removed - two of which were MEDRS (1 review, 1 pharmacology textbook) and a primary source on HUMANS (not rats) to supplement the MEDRS review (also on HUMANS) and expand upon the material from that secondary source. I based all of that on what I found on a lit. search, pubchem, and drugbank.
I didn't counter your claims the last time. Since this is now annoying me, I'm going to support my position with MEDRS sources, specifically, NCBI's tertiary source on amphetamine (Pubchem Compound) - a "data encyclopedia" if-you-will.
Before I go into this, just in the event this isn't evident to you from the last time we went over this, the term substituted amphetamine (74 results) is a wikipedia construct. Almost all medical literature refers to the "class of amphetamines" as amphetamineS (again, notice the "s") (33467 results vs 9261 results for methamphetamine, an amph that's been researched more extensively than amph itself).
The massive Pubchem Human Toxicity Section on Amphetamine - notice the highly emphasized passage on direct toxicity in the human brain (i.e. neurotoxicity)
|
|---|
|
Human Toxicity Excerpts [Emphasis added as bold, underlining, capitalizing an "S", and/or increased text size] The toxic dose of amphetamine varies widely. ... Severe reactions have occurred with 30 mg, yet doses of 400 to 500 mg are not uniformly fatal. Larger doses can be tolerated after chronic use of the drug. The acute toxic effects of amphetamine are usually extensions of its therapeutic actions and, as a rule, result from overdosage. The central effects commonly include restlessness, dizziness, tremor, hyperactive reflexes, talkativeness, tenseness, irritability, weakness, insomnia, fever, and sometimes euphoria. Confusion, assaultiveness, changes in libido, anxiety, delirium, paranoid hallucinations, panic states, and suicidal or homicidal tendencies occur, esp in mentally ill pt. However, these psychotic effects can be elicited in any individual if sufficient quantities of amphetamine are ingested for a prolonged period. Fatigue and depression usually follow central stimulation. Cardiovascular effects are common and include headache, chilliness, pallor or flushing, palpitation, cardiac arrhythmias, anginal pain, hypertension or hypotension, and circulatory collapse. Excessive sweating occurs. Symptoms referable to the GI system include dry mouth, metallic taste, anorexia, nausea, vomiting, diarrhea, and abdominal cramps. Fatal poisoning usually terminates in convulsions and coma, and cerebral hemorrhages are the main pathological findings. AMPHETAMINE GIVEN ORALLY RAISES BOTH SYSTOLIC & DIASTOLIC BLOOD PRESSURES. HEART RATE IS OFTEN REFLEXLY SLOWED; WITH LARGE DOSES, CARDIAC ARRHYTHMIAS MAY OCCUR. CARDIAC OUTPUT IS NOT ENHANCED BY THERAPEUTIC DOSES, & CEREBRAL BLOOD FLOW DOES NOT CHANGE MUCH. THE L-ISOMER IS SLIGHTLY MORE POTENT THAN THE D-ISOMER IN ITS CARDIOVASCULAR ACTIONS. IN GENERAL, SMOOTH MUSCLES RESPOND TO AMPHETAMINE AS THEY DO TO OTHER SYMPATHOMIMETIC AMINES. ... PAIN & DIFFICULTY IN MICTURITION OCCASIONALLY OCCUR. THE GI EFFECTS OF AMPHETAMINE ARE UNPREDICTABLE. IF ENTERIC ACTIVITY IS PRONOUNCED, AMPHETAMINE MAY CAUSE RELAXATION & DELAY THE MOVEMENT OF INTESTINAL CONTENTS; IF THE GUT IS ALREADY RELAXED, THE OPPOSITE EFFECT MAY OCCUR. THE RESPONSE OF THE HUMAN UTERUS VARIES, BUT USUALLY THERE IS AN INCREASE IN TONE. Because tolerance develops to the hyperthermic and cardiovascular effects of amphetamine, acute intoxication is more likely to occur in the neophyte. The syndrome includes dizziness, tremor, irritability, confusion, hallucinations, chest pain, palpitation, hypertension, sweating, and cardiac arrhythmias. There may be hyperpyrexia and convulsions. Death is usually preceded by hyperpyrexia, convulsions, and shock. Perivascular infiltration of amphetamineS can produce local necrosis, cellulitis, granulomas, & abscess formation. Intra-arterial injection causes intense vasospasm with distal cyanosis, ecchymosis, petechiae, edema, paresthesias, pain, weakness, necrosis, & decreased capillary filling. Immediate intense vasospasm is obvious after intra-arterial injections. Chronic intoxication with amphetamine causes symptoms similar to those of acute overdosage, but abnormal mental conditions are more common. Weight loss may be marked. A psychotic reaction with vivid hallucinations and paranoid delusions, often mistaken for schizophrenia, is the most common serious effect. Recovery usually is rapid after withdrawal of the drug, but occasionally the condition becomes chronic. In these persons, amphetamine may act as a precipitating factor hastening the onset of an incipient schizophrenia. Chronic use of high doses of amphetamineS has been reported to produce microvascular damage, neuronal chromatolysis (primarily in brain areas rich in adrenergic neurons), and profound and long lasting (or permanent) depletion of dopamine in the caudate nucleus. The psychic effects depend on the dose & the mental state & personality of the individual. The main results of an oral dose of 10-30 mg include wakefulness, alertness, & a decreased sense of fatigue; elevation of mood with increased initiative, self-confidence, & ability to concentrate; often, elation & euphoria; and increase in motor & speech activities. Performance of simple mental tasks is improved, but, although more work may be accomplished, the number of errors may increase. Physical performance - in athletes, for example - is improved, & the drug is often abused for this purpose. These effects are not invariable, & may be reversed by overdosage or repeated usage. Prolonged use or large doses are nearly always followed by depression & fatigue. Many individuals given amphetamine experience headache, palpitation, dizziness, vasomotor disturbances, agitation, confusion, dysphoria, apprehension, delirium, or fatigue. The fully developed toxic syndrome from amphetamine is characterized by vivid visual, auditory, and sometimes tactile hallucinations; picking and excoriation of the skin and delusions of parasitosis are not uncommon. There is also paranoid ideation, loosening of assoc, and changes in affect occurring in assoc with clear sensorium. In chronic users, there may be a striking paucity of sympathomimetic effects, and the blood pressure is not unduly elevated. It is often extremely difficult to differentiate this syndrome from a schizophrenic reaction. The syndrome may be seen as early as 36 to 48 hr after the ingestion of a single large dose of amphetamine; in apparently sensitive individuals, psychosis may be produced by 55 to 75 mg of dextroamphetamine. With high enough doses, psychosis can probably be induced in anyone. Unless the individual continues to use the drug, the psychosis usually clears within a week, the hallucinations being the first symptoms to disappear. Amphetamine ... in large doses systemically can dilate the pupils and cause slight blurring of near vision. Applied to the eye, amphetamine dilates the pupil and retracts the upper lid, but these actions are prevented by previous depletion of catecholamines such as is brought about by local guanethidine. Renal failure assoc with amphetamine use is usually the result of rhabdomyolysis, but it has also been found in patients without evidence of muscle damage or other apparent predisposing factors. Data on the effect of prenatal amphetamines, both prescribed and abused, are conflicting; however no consistent pattern of abnormalities has emerged. A large prospective evaluation of amphetamines prescribed during pregnancy found no incr in severe congenital malformations, but did report three cases of oral clefts. Another prospective study evaluating infants of amphetamine addicted women failed to demonstrate an incr in birth defects, but did note an incr in premature births, respiratory distress and jitteriness. The use of other drugs and alcohol may have confounded these findings. /Amphetamines/ In an acute poisoning in a child ... external stimuli precipitated increased hyperactivity. Abrupt discontinuation of amphetamines produces neither seizures nor life threatening symptoms, even in those patients who habitually consume large quantities. The abstinence syndrome assoc with chronic use of amphetamine ... is characterized by apathy, depression, lethargy, anxiety, & sleep disturbances. Myalgias, abdominal pain, voracious appetite, & a profound depression with suicidal tendencies may complicate the immediate postwithdrawal period & peak in 2-3 days. Symptoms persisting 6-7 days indicate an underlying disease process. During the early phases of iv use, 3 to 4 doses of 20 to 40 mg of amphetamine are usually considered sufficient /by abusers to produce euphoric effects/. In addition to the marked euphoria, the user experiences a sense of markedly enhanced physical strength & mental capacity, & feels little need for either sleep or food. Difficult to substantiate by objective means is the claim made by many users that orgasm in both male & female is delayed, permitting extended periods of sexual activity finally culminating in orgasms reported to be more intense & pleasurable. The sensation of "flash" or "rush" that immediately follows iv admin, while qualitatively distinct from the opioid "rush", is nevertheless described as being intensely pleasurable & somewhat akin to sexual orgasm. Many of those who use amphetamine ... are best described as "recreational" or occasional users, but some become dependent. A small percentage of the latter (eg, those taking the drugs for control of obesity) seem able to restrict drug intake & function productively (stabilized addicts). Others show progressive social & occupational deterioration, punctuated by periods of hospitalization for toxic psychosis. In terms of the compulsion to continue use, the degree to which a drug pervades the life of the user, & the tendency to relapse following withdrawal, some compulsive users of amphetamine ... are addicts. The risk of developing patterns of compulsive use is not limited to those who use drugs intravenously ... It is not clear whether the dependence syndromes caused by amphetamine ... are as persistent as that produced by opioids. In the US the waves of amphetamine use did not leave large numbers of chronic users in their wake. However, many iv users eventually became heroin users. ANOREXIA IS A COMMON FINDING /IN CHRONIC TOXICITY FROM ABUSE/. OCCASIONALLY IT MAY BE SO PRONOUNCED THAT THE AMPHETAMINE ABUSER EXPERIENCES CONSIDERABLE DIFFICULTY IN SWALLOWING. CHRONIC ABUSERS ARE REPORTED TO FORCE THEMSELVES TO EAT SMALL AMT OF HIGHLY NUTRITIOUS FOOD & TAKE VITAMIN SUPPLEMENTS TO COMPENSATE FOR DECR IN APPETITE. ... CONSTANT GRINDING OF TEETH IS ALSO A COMMON FINDING ... THE HISTORY, CHEMISTRY, PHARMACOLOGY, MEDICAL USE, ILLICIT USE & ADDICTION & TOLERANCE POTENTIAL OF AMPHETAMINES ARE PRESENTED. ALTHOUGH THERE ARE FEW PUBLISHED ACCOUNTS OF DEATH KNOWN TO RESULT DIRECTLY FROM AMPHETAMINES, DEATHS MAY RESULT INDIRECTLY FROM EFFECTS SUCH AS VIOLENT BEHAVIOR & HEPATITIS.[HART JB, WALLACE J; CLIN TOXICOL 8 (2): 179-90 (1975)] PubMed Abstract Few deaths have ... been attributed to amphetamine overdose. Amphetamines have a relatively low ratio of effective dose to fatal dose. Fatalities resulting from amphetamine use are usually the result of one of the following processes: 1) combinations with other drugs; 2) complications of iv injections, such as septicemia, bacterial endocarditis, or homicide, during withdrawal depression. Although comparable clinical data are lacking, hyperpyrexia has been noted as a frequent & prominent sign in acute human intoxication. During a grueling bicycle race a cyclist collapsed with symptoms closely resembling heat exhaustion, &, despite vigorous treatment, he died /after/ cardiovascular collapse; it was learned subsequently that he had consumed 105 mg of amphetamine during the race. Bleeding within the cranial vault is a rare but well-reported complication of amphetamine use. About 20 cases, which are about evenly divided between iv & oral exposures, have been reported in the American literature. Ages range from 16-60, & most patients are habitual & often multidrug abusers. However, intracranial hemorrhages have been reported after the ingestion of as few as 2-4 tablets of amphetamine or structurally related anorectic drugs ... The etiology of intracerebral & subarachnoid hemorrhages associated with amphetamine use appears multifactorial. Inflammation & necrosis of small cerebral arteries (ie, vasculitis) secondary to particulate foreign bodies or bacterial endocarditis can develop after iv drug use. Subsequently, the hypertension seen in amphetamine use may lead to vessel rupture & hemorrhage. However, vasculitis has occurred in the setting of oral acute dextroamphetamine overdose, amphetamine withdrawal, & therapeutic use as an anorectic drug. The presence of vasculitis after exposure by different routes suggests an immunopathological abnormality. Direct toxic damage to vessels seems unlikely because of the dilution that occurs before the drug reaches the cerebral circulation. Repetitive behavior may occur /from the use of amphetamines/ (e.g. repeatedly cleans dishes or continually grooms hair). Amphetamines also will extenuate hostile, aggressive, and antisocial behavior. Progression to paranoia, panic states, violence, and even suicide may occur. /Amphetamines/ Amphetamines used in large doses over a long period of time may lead to substantial weight loss, liver disease, hypertensive disorders, kidney damage, stroke, heart attack, nonhealing ulcers, and sores in the skin. /Amphetamines/ The abuse of amphetamines by combining the oral and inhalation routes of administration usually leads to a more intense effect and/or more toxic effect than if either was taken alone. /Amphetamines/ Doses as little as 2 mg, but more likely between 15 and 30 mg, may induce toxic effects. However, even doses of 400-500 mg are not uniformly fatal. Illicit maternal use /of amphetamines is/ associated with intrauterine growth retardation, premature birth, and increased fetal and newborn morbidity. /Amphetamines, from table/ Intrauterine ... amphetamine exposure may cause neonates to exhibit abnormal sleep patterns, tremors, poor feeding, hypotonia, fever, and vomiting. |
NCBI cited the amph article ref named "Westfall" for it's toxicity statements on the class of amphetamines. I cited Westfall too and not only covered what it said on amphetamine (oxidative damage from radical species), I also expanded upon it with the other two sources. Most of the WP:PAYWALLED refs cited in the article are hosted here, including other relevant sections of the Westfall ref that I didn't cite in the article.
With all that said, I'll just summarize and briefly state the issues:
- NCBI's pubchem page on amphetamine and my graduate molecular neuropharmacology textbook (the ref named "Malenka_2009"), both MEDRS sources, directly support the statement that amphetamine is NOT "directly neurotoxic" in humans and hence, by definition, it is NOT a neurotoxin to humans. (Note also that cerebral hemorrhage is a lethal medical emergency that occurs only at stupidly high doses, as stated/cited in the article OD section) That's two highly authoritative sources now that have asserted this.
- In your edits, you changed "The only proposed mechanism for neurotoxicity from high-dose amphetamine use in humans is indirect damage to dopamine terminals via autoxidation of dopamine, as opposed to direct toxicity from amphetamine" to "a variety of potential mechanisms for indirect neurotoxicity have been proposed." As this passage was and currently still is about humans, I'm going to ask you to explicitly state/list them with a WP:MEDRS citation (preferably, explain the mechanism with the same level of detail as on human dopamine autoxidation for consistency).
If you add a WP:MEDRS secondary source demonstrating the existence of (singular) amphetamine neurotoxicity in humans, I would be happy to see and have it included in the article. If you add a source that falls short of what the policy requires, I will revert it, per the policy. If you change and of the language in that section such that it doesn't agree with the cited sources (hence causing at least WP:V and potentially WP:NPOV issues), I will revert it. WP policy practically dictates that I do this if I want to see this article reach FA.
Lastly, I also find it almost obnoxious, and it's completely illogical, to suggest that *I* am causing WP:NPOV problems with this article when you're citing animal studies to make claims about humans any skewing text-source integrity (the refs on humans stated only a single mechanism and you stated there were multiple). I'm not assuming bad faith on your part - now stop making assumptions and accusations about mine. Seppi333 (talk) 18:12, 1 December 2013 (UTC)
- I don't have much time to get in another war over this at the moment, but you're clearly in the wrong and I'm going to briefly outline my points:
- To clarify, the POV you inject is that amphetamine isn't actually neurotoxic in humans (alternatively stating or strongly implying that this is proven true).
- The statement I removed was "The only proposed mechanism for neurotoxicity from high-dose amphetamine use in humans is indirect damage to dopamine terminals via autoxidation of dopamine". This is simply factually untrue. A variety of possible mechanisms have been suggested. I don't need a MEDRS source to verify that because that statement doesn't state a fact about a medical topic, it states the existence of proposed opinions. A legitimate published alternate opinion is proof of the existence of an alternate opinion.
- We already went through a very extended discussion about this. I had to pull two outside mediators in to correct you. We came up with a mutually accepted passage, heavily cited with quoted MEDRS sources. You then removed it and added a POV version with all the sources/quotes mentioning neurotoxicity removed. I was never notified of this.
This is ridiculous and unjustifiable. I'm going to have to bring more mediators in when I have the time. Exercisephys (talk) 22:56, 1 December 2013 (UTC)
There are bad faith user warning templates for a reason. I normally avoid using them because, exactly like going off topic, personal attacks, or asserting bad faith intent of other users, it detracts from a conversation. So, once again, and I won't ask next time, please, stop saying I'm intentionally POV editing and focus on the actual issue: we need sources to directly support the text.
For 1: I've literally just asked you for a MEDRS source indicating other indirect mechanisms besides radical toxicity in humans or a source for any direct toxicity by amph in humans. You've just replied to this by restating this; it's a bit circular, but ignoring that, unfortunately, I don't think you are a MEDRS source. For 2: As I told you like a week ago via the user notification template in a thread currently on this page (SwampFox's thread, current the third section on this page as of this edit), I moved that material to the ADHD section. The paper is on neuroplasticity, not neurotoxicity. It's a more general concept. If anything, it belongs in the OD section, but since the study a study on human neuroplasticity is in that section, it MUST be there in order to not refute that source elsewhere in the article. I only kept it because you've been complaining I delete your material. If you didn't cite animal studies I probably wouldn't be trying to remove it.
[Related aside to this list item: I've said it over and over again, animal studies do not say anything about humans - extending the inference is spurious because the non-human sample in those studies is a nonprobability sample for human neurotoxicity. I can literally produce an analytic proof to demonstrate that any statistical model for a drug effect using nonprobability sampling (like animal studies with inference on humans) is spurious. In other words, I am literally stating that every animal study that has ever been conducted to detect the presence of any drug-related phenomenon in any (non-human) species yields invalid/spurious statistical inference in humans (the bolded terms are universal quantification in an analytic context). The fact that I can make that statement given that much scope is why representative sampling, like random sampling, is such a fundamental concept in statistics. Literally every stat textbook you might check for reference will tell you use "random" and "representative" samples. It's included in intro stats texts without rigorous justification simply because most people taking an intro stats course won't understand analytic proofs (i.e. the kind of argument in the collapse tabs of holder's inequality). In the event you don't have a solid background in math, just take it on faith - it's stated everywhere for a reason. This is the exact reason WP:MEDRS has a policy that says "don't use animal studies." The MEDRS policy is the justification for why I remove animal studies. This "aside" is an explanation of why that policy even exists.]
Added by Seppi333 at 19:43, 7 December 2013 (UTC) - I made the policy shortcut WP:MEDANIMAL for your reference.
For 3: I revised the passage that I stated without citation. Sasata reviewed the content and asserted that all medical claims had adequate MEDRS citations yesterday in the concluding remarks to the GA review. He did an extremely thorough review to help this article with FA and I provided every single WP:PAYWALLED source in the GA-review (it's still linked in the GA archive with all the files still hosted in the link). I don't think he'd make that statement lightly.
I'm not asking you do to anything that any editor from WP:MED wouldn't ask of you.
If you state or even imply "some evidence of amphetamine neurotoxicity exists in humans" you need a source on amphetamine which states amphetamine is a neurotoxin. Stop using some paper on an entire class of substances, some of which have been proven to be neurotoxins in humans (meth). A paper on amphetamine human neurotoxicity would unequivocally support a statement about that - this ref is the ONLY THING you need (as well as what must be) cited to make that particular medical claim. That's the same standard for citing any medical claim. You need a ref making a definite statement which directly supports an included medical statement in the article. Every single source in the article CURRENTLY has a direct text-source relation like that, which is stated as what's required of a citation in WP:V. How do I know this? I checked all 100+ sources in the article when I did the WP:V check for GA. You only need to do this for a single source. It's not that hard. If the material you claim to be true exists, a paper on human amph neurotoxicity will be easy to produce (and it literally says this is true of the prevailing/majority viewpoint in WP:DUE. If it's not easy to find, you should be able to list a major proponent of the theory (ideally, someone who has done a case study demonstrating this). If you can't find a ref on amphetamine neurotoxicity, it shouldn't be on wikipedia, per WP:UNDUE. So once again, I'm not taking a position on content. I'm enforcing a policy that you know very well, as I've told you to use it CONSTANTLY in the last thread on this.
I want to emphasize these points so this thread isn't directed off on some random tangent again:
- Please, for the love of god, don't argue with me and just cite the source which backs the statement you want to make. That's all I'm asking of you.
- I frankly don't know or even care about what you or anyone else believes is correct about amphetamine neurotoxicity.
- I also do not even care about whether or not it's actually neurotoxic in some manner/dose in humans.
- I DO care about whether or not the citation supporting that statement satisfies the relevant policies, which are there for a reason. Seppi333 (talk) 06:54, 2 December 2013 (UTC)
I figured I'd cite WP:MEDASSESS here and underline what the original claim of neurotoxicity is in this list:
Roughly in descending order of quality, lower-quality evidence in medical research comes from individual RCTs; other controlled studies; quasi-experimental studies; non-experimental, observational studies, such as cohort studies and case control studies, followed by cross-sectional studies (surveys), and other correlation studies such as ecological studies; and non-evidence-based expert opinion or clinical experience
Regards, Seppi333 (talk) 19:50, 7 December 2013 (UTC)
The discussion concluded at [1].
Pharmacology section
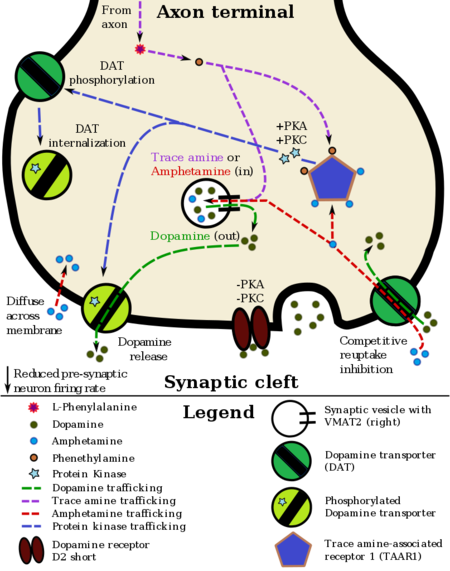
Does this help at all with explaining the technical stuff in this section? (Copied from User:Seppi333/sandbox2#pharmacodynamics)
Seppi333 (talk) 23:03, 11 December 2013 (UTC)
- Yes, I think this image would be a welcome addition! Sasata (talk) 00:26, 12 December 2013 (UTC)
Metabolic pathways of amphetamine in humans[sources 1]
|
I put this in the article as well - same as before, but with winkilink annotations (citation errors not included ![]() ). I think that's all I can do with the images for now. Seppi333 (Insert 2¢) 08:15, 13 December 2013 (UTC)
). I think that's all I can do with the images for now. Seppi333 (Insert 2¢) 08:15, 13 December 2013 (UTC)
References
- ^ a b "Adderall XR Prescribing Information" (PDF). United States Food and Drug Administration. Shire US Inc. December 2013. pp. 12–13. Retrieved 30 December 2013.
- ^ a b Glennon RA (2013). "Phenylisopropylamine stimulants: amphetamine-related agents". In Lemke TL, Williams DA, Roche VF, Zito W (eds.). Foye's principles of medicinal chemistry (7th ed.). Philadelphia, US: Wolters Kluwer Health/Lippincott Williams & Wilkins. pp. 646–648. ISBN 9781609133450.
The simplest unsubstituted phenylisopropylamine, 1-phenyl-2-aminopropane, or amphetamine, serves as a common structural template for hallucinogens and psychostimulants. Amphetamine produces central stimulant, anorectic, and sympathomimetic actions, and it is the prototype member of this class (39). ... The phase 1 metabolism of amphetamine analogs is catalyzed by two systems: cytochrome P450 and flavin monooxygenase. ... Amphetamine can also undergo aromatic hydroxylation to p-hydroxyamphetamine. ... Subsequent oxidation at the benzylic position by DA β-hydroxylase affords p-hydroxynorephedrine. Alternatively, direct oxidation of amphetamine by DA β-hydroxylase can afford norephedrine.
- ^ Taylor KB (January 1974). "Dopamine-beta-hydroxylase. Stereochemical course of the reaction" (PDF). Journal of Biological Chemistry. 249 (2): 454–458. doi:10.1016/S0021-9258(19)43051-2. PMID 4809526. Retrieved 6 November 2014.
Dopamine-β-hydroxylase catalyzed the removal of the pro-R hydrogen atom and the production of 1-norephedrine, (2S,1R)-2-amino-1-hydroxyl-1-phenylpropane, from d-amphetamine.
- ^ Krueger SK, Williams DE (June 2005). "Mammalian flavin-containing monooxygenases: structure/function, genetic polymorphisms and role in drug metabolism". Pharmacology & Therapeutics. 106 (3): 357–387. doi:10.1016/j.pharmthera.2005.01.001. PMC 1828602. PMID 15922018.
Table 5: N-containing drugs and xenobiotics oxygenated by FMO - ^ Cashman JR, Xiong YN, Xu L, Janowsky A (March 1999). "N-oxygenation of amphetamine and methamphetamine by the human flavin-containing monooxygenase (form 3): role in bioactivation and detoxication". Journal of Pharmacology and Experimental Therapeutics. 288 (3): 1251–1260. PMID 10027866.
- ^ a b Santagati NA, Ferrara G, Marrazzo A, Ronsisvalle G (September 2002). "Simultaneous determination of amphetamine and one of its metabolites by HPLC with electrochemical detection". Journal of Pharmaceutical and Biomedical Analysis. 30 (2): 247–255. doi:10.1016/S0731-7085(02)00330-8. PMID 12191709.
- ^ a b c Sjoerdsma A, von Studnitz W (April 1963). "Dopamine-beta-oxidase activity in man, using hydroxyamphetamine as substrate". British Journal of Pharmacology and Chemotherapy. 20 (2): 278–284. doi:10.1111/j.1476-5381.1963.tb01467.x. PMC 1703637. PMID 13977820.
Hydroxyamphetamine was administered orally to five human subjects ... Since conversion of hydroxyamphetamine to hydroxynorephedrine occurs in vitro by the action of dopamine-β-oxidase, a simple method is suggested for measuring the activity of this enzyme and the effect of its inhibitors in man. ... The lack of effect of administration of neomycin to one patient indicates that the hydroxylation occurs in body tissues. ... a major portion of the β-hydroxylation of hydroxyamphetamine occurs in non-adrenal tissue. Unfortunately, at the present time one cannot be completely certain that the hydroxylation of hydroxyamphetamine in vivo is accomplished by the same enzyme which converts dopamine to noradrenaline.
- ^ Badenhorst CP, van der Sluis R, Erasmus E, van Dijk AA (September 2013). "Glycine conjugation: importance in metabolism, the role of glycine N-acyltransferase, and factors that influence interindividual variation". Expert Opinion on Drug Metabolism & Toxicology. 9 (9): 1139–1153. doi:10.1517/17425255.2013.796929. PMID 23650932. S2CID 23738007.
Figure 1. Glycine conjugation of benzoic acid. The glycine conjugation pathway consists of two steps. First benzoate is ligated to CoASH to form the high-energy benzoyl-CoA thioester. This reaction is catalyzed by the HXM-A and HXM-B medium-chain acid:CoA ligases and requires energy in the form of ATP. ... The benzoyl-CoA is then conjugated to glycine by GLYAT to form hippuric acid, releasing CoASH. In addition to the factors listed in the boxes, the levels of ATP, CoASH, and glycine may influence the overall rate of the glycine conjugation pathway.
- ^ Horwitz D, Alexander RW, Lovenberg W, Keiser HR (May 1973). "Human serum dopamine-β-hydroxylase. Relationship to hypertension and sympathetic activity". Circulation Research. 32 (5): 594–599. doi:10.1161/01.RES.32.5.594. PMID 4713201. S2CID 28641000.
The biologic significance of the different levels of serum DβH activity was studied in two ways. First, in vivo ability to β-hydroxylate the synthetic substrate hydroxyamphetamine was compared in two subjects with low serum DβH activity and two subjects with average activity. ... In one study, hydroxyamphetamine (Paredrine), a synthetic substrate for DβH, was administered to subjects with either low or average levels of serum DβH activity. The percent of the drug hydroxylated to hydroxynorephedrine was comparable in all subjects (6.5-9.62) (Table 3).
- ^ Freeman JJ, Sulser F (December 1974). "Formation of p-hydroxynorephedrine in brain following intraventricular administration of p-hydroxyamphetamine". Neuropharmacology. 13 (12): 1187–1190. doi:10.1016/0028-3908(74)90069-0. PMID 4457764.
In species where aromatic hydroxylation of amphetamine is the major metabolic pathway, p-hydroxyamphetamine (POH) and p-hydroxynorephedrine (PHN) may contribute to the pharmacological profile of the parent drug. ... The location of the p-hydroxylation and β-hydroxylation reactions is important in species where aromatic hydroxylation of amphetamine is the predominant pathway of metabolism. Following systemic administration of amphetamine to rats, POH has been found in urine and in plasma.
The observed lack of a significant accumulation of PHN in brain following the intraventricular administration of (+)-amphetamine and the formation of appreciable amounts of PHN from (+)-POH in brain tissue in vivo supports the view that the aromatic hydroxylation of amphetamine following its systemic administration occurs predominantly in the periphery, and that POH is then transported through the blood-brain barrier, taken up by noradrenergic neurones in brain where (+)-POH is converted in the storage vesicles by dopamine β-hydroxylase to PHN. - ^ Matsuda LA, Hanson GR, Gibb JW (December 1989). "Neurochemical effects of amphetamine metabolites on central dopaminergic and serotonergic systems". Journal of Pharmacology and Experimental Therapeutics. 251 (3): 901–908. PMID 2600821.
The metabolism of p-OHA to p-OHNor is well documented and dopamine-β hydroxylase present in noradrenergic neurons could easily convert p-OHA to p-OHNor after intraventricular administration.
Long-term therapeutic use in humans - neuroplasticity
@Exercisephys: Following this conversation, these refs[1][2] were added to ADHD to support the benefits of psychostimulants on the human brain. I'm notifying you for the sake of openness, because I'm now adding the refs to this article and their conclusions directly contradict what the animal studies that you added imply for humans. I also don't to give you the impression that I'm trying to subvert you again. This is the current paragraph in medical:
In studies of amphetamine exposure in nonhuman primates, some report no discernible adverse effects on behavior or dopamine system development, while others noted reductions to dopamine-associated structures and metabolites.[3][4] In stark contrast for humans, recent literature reviews, including a meta-analysis and a systematic review, indicate that the long-term use of amphetamine at therapeutic doses for ADHD actually appears to produce beneficial changes in brain function and structure, such as an improvement in function of the right caudate nucleus.[1][2]
Best regards, Seppi333 (Insert 2¢) 06:44, 4 January 2014 (UTC)
References
- ^ a b Hart, H (February 2013). "Meta-analysis of functional magnetic resonance imaging studies of inhibition and attention in attention-deficit/hyperactivity disorder: exploring task-specific, stimulant medication, and age effects". JAMA psychiatry. 70 (2): 185–98. PMID 23247506.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b Spencer, TJ (September 2013). "Effect of psychostimulants on brain structure and function in ADHD: a qualitative literature review of magnetic resonance imaging-based neuroimaging studies". The Journal of clinical psychiatry. 74 (9): 902–17. PMID 24107764.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Berman S, O'Neill J, Fears S, Bartzokis G, London ED (2008). "Abuse of amphetamines and structural abnormalities in the brain". Ann. N. Y. Acad. Sci. 1141: 195–220. doi:10.1196/annals.1441.031. PMC 2769923. PMID 18991959.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Volkow ND (2012). "Long-term safety of stimulant use for ADHD: findings from nonhuman primates". Neuropsychopharmacology. 37 (12): 2551–2552. doi:10.1038/npp.2012.127. PMC 3473329. PMID 23070200.
{{cite journal}}: Unknown parameter|month=ignored (help)
Drugbox structure image
I was thinking about changing the drugbox image.
Does anyone have an objection to or support this change? Seppi333 (talk) 22:24, 30 November 2013 (UTC)
I think that it could be presented in the chemistry section, but that the main drugbox should only contain the original. Exercisephys (talk) 23:35, 1 December 2013 (UTC)
Supplemental FA-review feedback
@The Sceptical Chymist: I wanted to keep all these sections together for the archives - I hope this is ok with you; feel free to revert this edit if not. Best regards, Seppi333 (Insert 2¢) 01:27, 11 January 2014 (UTC).
When was amphetamine discovered/synthesized?
A contradiction in references. The article states "Amphetamine was first synthesized in 1887 in Germany by Romanian chemist Lazăr Edeleanu who named it phenylisopropylamine". On the other hand, a different reference, also used in the article (Heal DJ, Smith SL, Gosden J, Nutt DJ (June 2013). "Amphetamine, past and present – a pharmacological and clinical perspective") states: "racemic α-methylphenethylamine (amphetamine) was discovered by Barger and Dale in 1910, it was not until 1927 that this molecule was first synthesised by the chemist, G. A. Alles" The Sceptical Chymist (talk) 03:44, 10 January 2014 (UTC)
- I'll see if I can fish up a source specifying the difference between both. I encountered this issue a while back but just chose to ignore it because I had included the original paper from Lazar as a citation, but chose to delete it due to its age, being over a century old (it's the first citation in History and culture of amphetamines#History (amphetamine)). Seppi333 (Insert 2¢) 00:21, 11 January 2014 (UTC)
- This ref covers the distinction - it was an independent resynthesis:[1]
Long quote
|
|---|
|
Synthetic AMPH was invented in 1887 by Lazar Edeleanu (1862–1941, a.k.a. Edeleano), a Rumanian chemist who described its synthesis in his doctoral dissertation under A.W. Hofmann at the University of Berlin (Edeleano, 1887). Edeleanu later became famous for also inventing the method to distill petroleum using sulphur dioxide, providing the tell-tale odor of gasoline distilleries. AMPH was bequeathed its generic name from a contraction of α-methyl-phenethyl-amine. Some notion of the colorful history of this drug can be seen from the 1989 Merck Index listing, which lists 17 trade names, not even including such familiar trade names as Adderall, Benzedrine, and Dexedrine, or for that matter the myriad nicknames used by drug abusers. Of course, chemists have since developed an astonishing range of synthetic AMPH derivatives. Following work discussed below by Barger and Dale that introduced the concept of sympathomimetic amines (Section 3.1), researchers have examined a wide range of catecholamine-like derivatives for the ability to raise blood pressure and to relieve nasal and bronchial congestion from colds and hay fever. AMPH was independently resynthesized by Gordon Alles in 1927 in an effort toward developing synthetic sympathomimetics, and he and his coworkers are credited with the first report of its stimulant effects |
- Did you want me to note this in the article itself? Seppi333 (Insert 2¢) 01:57, 11 January 2014 (UTC)
- I think both stories should be given since it is not clear which one of them is correct. Barger/Dale 1910 or Edeleanu in 1887 The Sceptical Chymist (talk) 17:19, 15 January 2014 (UTC)
 Added to History section. Seppi333 (Insert 2¢) 19:46, 15 January 2014 (UTC)
Added to History section. Seppi333 (Insert 2¢) 19:46, 15 January 2014 (UTC)
References
- ^ Sulzer D, Sonders MS, Poulsen NW, Galli A (2005). "Mechanisms of neurotransmitter release by amphetamines: a review". Prog. Neurobiol. 75 (6): 406–33. doi:10.1016/j.pneurobio.2005.04.003. PMID 15955613.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)
Notes on literature
Reference 17 - "Methamphetamine facts". DrugPolicy.org. - is probably not the best source, even for the history reference. It is a website of an advocacy organization. Accordingly, a better reference supporting the historical use of amphetamine for nasal congestion and obesity is needed. The Sceptical Chymist (talk) 04:24, 10 January 2014 (UTC)
- I've replaced that source with the "Amph Uses" and "Benzedrine" sources,[1][2] since together they encompass all the uses cited in the DrugPolicy.org ref.[3]
Reference 29 - Berman S, O'Neill J, Fears S, Bartzokis G, London ED (2008). "Abuse of amphetamines and structural abnormalities in the brain", at least according to the abstract is not relevant to amphetamine. It is about the abuse of amphetaminES, but amphetamine appears not to be among the drugs considered in the reviewed literature. From the abstract: "Ten studies compared controls to individuals who were exposed to methamphetamine. Three studies assessed individuals exposed to 3–4-methylenedioxymethamphetamine (MDMA)." The Sceptical Chymist (talk) 04:38, 10 January 2014 (UTC)
- I completely agree with you - I'd have deleted this source in a heartbeat; however, I've had several run-ins with another editor (first thread, second thread, and a mediation attempt that was resolved independently) on the topic of amphetamine neurotoxicity and adverse neuroplastic alterations in methamphetamine users and amphetamine in animals vs the effects of amphetamine in humans. Because I don't want to create more unnecessary conflict with him, I chose to include his source but very clearly and assertively indicate that these effects are not present in humans using amphetamine at therapeutic doses. I did the same thing to differentiate amphetamine from methamphetamine on the methamphetamine page in the neurotoxicity and pharmacodynamics sections.Seppi333 (Insert 2¢) 01:02, 11 January 2014 (UTC)
References
- ^ Heal DJ, Smith SL, Gosden J, Nutt DJ (2013). "Amphetamine, past and present – a pharmacological and clinical perspective". J. Psychopharmacol. 27 (6): 479–496. doi:10.1177/0269881113482532. PMC 3666194. PMID 23539642.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Rasmussen N (2006). "Making the first anti-depressant: amphetamine in American medicine, 1929–1950". J . Hist. Med. Allied Sci. 61 (3): 288–323. doi:10.1093/jhmas/jrj039. PMID 16492800.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ "Methamphetamine facts". DrugPolicy.org. Retrieved 19 October 2013.
Effects of stimulants for ADHD on brain functions
- In stark contrast for humans, literature reviews from 2013, including a meta-analysis and a systematic review, indicate that the long-term use of amphetamine at therapeutic doses for ADHD actually appears to produce beneficial changes in brain function and structure, such as an improvement in function of the right caudate nucleus.[[Amphetamine#cite_note-Neuroplasticity_1-38|]]
This wording seems to be too strong, considering the cautious way the results are summarized in the corresponding references:
- preliminary evidence suggests that long-term stimulant medication use may be associated with more normal activation in right caudate during the attention domain (Hart, 2013)
- Despite the inherent limitations and heterogeneity of the extant MRI literature, our review suggests that therapeutic oral doses of stimulants decrease alterations in brain structure and function in subjects with ADHD relative to unmedicated subjects and controls. (Spencer, 2013)
I suggest the following re-wording of this paragraph:
- The most recent systematic reviews of magnetic resonance imaging studies suggest that the treatment of ADHD with stimulants, including amphetamine, may decrease the abnormalities in brain structure and functions in subjects with ADHD, for example, in activation of right caudate nucleus during attention tasks.
The Sceptical Chymist (talk) 13:49, 10 January 2014 (UTC)
- Based upon JMH649's critiques of similar wording that I used to describe this,[1] and due to the issues mentioned in the above section, I'm going with a mix of your wording and the current version:
In stark contrast for humans, literature reviews from 2013, including a meta-analysis and a systematic review, of magnetic resonance imaging studies indicate that long-term treatment of ADHD with amphetamine may decrease the abnormalities in brain structure and function in subjects with ADHD, such as an improvement in function of the right caudate nucleus.
- Original wording for comparison:
In stark contrast for humans, literature reviews from 2013, including a meta-analysis and a systematic review, indicate that the long-term use of amphetamine at therapeutic doses for ADHD actually appears to produce beneficial changes in brain function and structure, such as an improvement in function of the right caudate nucleus.
- Thanks for all the feedback - I really appreciate all the effort you're putting into this!
 Seppi333 (Insert 2¢) 01:21, 11 January 2014 (UTC)
Seppi333 (Insert 2¢) 01:21, 11 January 2014 (UTC)
References
- ^ My wording was: "Despite the potential biases, limitations, and data heterogeneity endemic to studies on the long-term effects of ADHD stimulants, the results appear to suggest that these drugs normalize brain structure abnormalities in ADHD and improve classroom behavior and academic performance in children.[1][2][3]"
Multiple problems with pharmacokinetics chapter
"However, oral availability varies with gastrointestinal pH.[72] Amphetamine is a weak base with a pKa of 9–10;[3] consequently, when the pH is basic, more of the drug is in its lipid soluble free base form, and more is absorbed through the lipid-rich cell membranes of the gut epithelium.[3][72] Conversely, an acidic pH means the drug is predominantly in its water soluble cationic form, and less is absorbed.[3][72]"
- Reference 72 does not directly point out that oral availability varies with gastrointestinal pH. To the contrary, it states: "Food does not affect the extent of absorption of d-amphetamine and l-amphetamine, but prolongs Tmax by 2.5 hours (from 5.2 hrs at fasted state to 7.7 hrs after a high-fat meal) for d-amphetamine and 2.7 hours (from 5.6 hrs at fasted state to 8.3 hrs after a high fat meal) for l-amphetamine after administration of ADDERALL XR 30 mg." Note that food makes the stomach more acidic.
The confusion stems from the fact that taking amphetamines with multiple grams (>10 g per day) of sodium bicarbonate (alkalyzer) or ammonium chloride (acidifier) does affect bioavailability of amphetamine. However, this is relevant only to research situations, and in practice no person would consume spoons of soda or ammonium chloride.
Next, there seem to be no evidence that large amounts of alkalizer of acidifier would change the absorption of amphetamine. It appears that they predominantly work through changing elimination (as described in he article below).
One of the strongest antacids (proton pump inhibitor) omeprazol also does not change bioavailability of amphetamine: "For MAS XR monotherapy, total amphetamine mean (SD) exposure was 36.6 (9.19) ng/mL and 640.8 (95.66) ng . h/mL; when coadministered with omeprazole it was 38.1 (7.35) ng/mL and 643.9 (143.16) ng . h/mL, for Cmax and AUCinf, respectively. The median Tmax was 5 hours and 2.75 hours without and with omeprazole, respectively; 57.1% to 61.9% of subjects receiving MAS XR and 25% receiving LDX showed an earlier (>or= 1 hour) Tmax with omeprazole" (PMID 19820270)
And lastly, amphetamine has pKa of 9.9 according to the reference you cited; it is a strong organic base.
The Sceptical Chymist (talk) 15:25, 16 January 2014 (UTC)
- Ehh...PPIs, like gastric H2 antagonists, are just gastric acid neutralizers - they're not really antacids like typical OTC agents (i.e.,calcium carbonate or magnesium hydroxide) - ie they wont make the stomach more alkaline than its pH sans gastric acid. I'd assume you'd only see a noticeable effect if you generate a lot of digestive acids, since that's all they neutralize. In any event, the quoted passage actually comes from the interactions section of the Rx info:
7 DRUG INTERACTIONS
7.1 Agents that Increase Blood Levels of Amphetamines
... Alkalinizing Agents
Gastrointestinal alkalinizing agents (e.g., sodium bicarbonate) increase absorption of amphetamines. Co-administration of ADDERALL XR and
gastrointestinal alkalinizing agents, such as antacids, should be avoided. Urinary alkalinizing agents (acetazolamide, some thiazides) increase the
concentration of the non-ionized species of the amphetamine molecule, thereby decreasing urinary excretion. Both groups of agents increase
blood levels and therefore potentiate the actions of amphetamines.
7.2 Agents that Lower Blood Levels of Amphetamines
Acidifying Agents
Gastrointestinal acidifying agents (e.g., guanethidine, reserpine, glutamic acid HCl, ascorbic acid) lower absorption of amphetamines. Urinary
acidifying agents (e.g., ammonium chloride, sodium acid phosphate, methenamine salts) increase the concentration of the ionized species of the
amphetamine molecule, thereby increasing urinary excretion. Both groups of agents lower blood levels and efficacy of amphetamines.
— Bottom of page 8 to the top of page 9 in the Rx info
- I don't have much more time to write this reply since I need to get stuff done irl, but the pharmacokinetics part of Anypodetos' section covers a lot of discussion about bioavailability and acid/alkaline agents. Seppi333 (Insert 2¢) 15:38, 16 January 2014 (UTC)
- Feel free to ask me about the supporting content for references/verifiability if you can't locate something in a ref. I've checked the text-source integrity of every citation at least once (multiple times for heavily cited sources). Seppi333 (Insert 2¢) 16:59, 16 January 2014 (UTC)
"Peer review" comments
Lead:
- "approved for the treatment of" -- approved by whom? The FDA? If yes, what about rest of world? If no, who approved?
 Fixed changed to original wording. approval isnt mentioned, since the compound isn't technically what the FDA approves anyway - it's the brand mixtures & brands.
Fixed changed to original wording. approval isnt mentioned, since the compound isn't technically what the FDA approves anyway - it's the brand mixtures & brands. - "in many countries, unauthorized possession and distribution of amphetamine is often tightly controlled due to the significant health risks associated with uncontrolled or heavy use.[15][16][17] Consequently, amphetamine is illegally synthesized, trafficked, and sold" -- do we have any proof that the illegal synthesis, trafficking and selling of amphetamine is a consequence of laws? Sounds obvious but really this is a post hoc ergo propter hoc fallacy.
 Meant to indicate that the illegality is a consequence, not the acts - implying the acts are would definitely be a post hoc fallacy. I tweaked the wording since someone changed it though - not all synth is illegal.
Meant to indicate that the illegality is a consequence, not the acts - implying the acts are would definitely be a post hoc fallacy. I tweaked the wording since someone changed it though - not all synth is illegal. - "enantiomers"-- although this is wikilinked, it should be expected that readers will find explanation for jargon in the page htey are reading. We should not shy away from jargon, we should use the language the sources use, but we need to adequately explain any jargon to a general audience. The gold standard imo is a wikilink combined with a parenthetical lay explanation. As this is the lead and there is already a note at the end of the sentence, maybe the explanation could be incorporated into the note.
 Fixed
Fixed - " It was first made available as a pharmaceutical drug under the Benzedrine brand of inhalers for a variety of medical conditions." this is unnecessarily verbose. Consider "It was first available as Benzedrine inhalers for a variety of conditions"
 Fixed - I actually lengthened it a tiny bit, but made the wording more direct. "The first pharmaceutical amphetamine the was Benzedrine, a brand of inhalers used to treat a variety of conditions."
Fixed - I actually lengthened it a tiny bit, but made the wording more direct. "The first pharmaceutical amphetamine the was Benzedrine, a brand of inhalers used to treat a variety of conditions." - "neurotransmitters "-- I understand you are already linking catecholamines etc in this sentence, but I think we have an article for this term too.
 I actually wanted to do that originally, but couldn't think of how to reword it, since WP:SEAOFBLUE says to avoid back-to-back wikilinking multiple terms.
I actually wanted to do that originally, but couldn't think of how to reword it, since WP:SEAOFBLUE says to avoid back-to-back wikilinking multiple terms. - "psychological and cognitive effects"-- is there a difference between these terms?
 Fixed as emotional and cognitive
Fixed as emotional and cognitive - "Very high doses can induce a state of psychosis characterized by delusions and paranoia, and, although rare, this may also occur as a side effect during long-term use at therapeutic doses.[17][24] Moreover, recreational doses are generally much larger than prescribed therapeutic doses, and recreational use therefore carries a far greater risk of serious side effects.[25]"-- unnecessarily verbose. Consider "Very high doses can induce psychosis (e.g. delusions and paranoia). Rarely this can occur with long term use at therapeutic doses, however recreational doses tend to be larger and carry more risk of serious side effects"
 Fixed shortened the first half. The emphasis in the second reflects the ref's, so I kept the magnitude terms
Fixed shortened the first half. The emphasis in the second reflects the ref's, so I kept the magnitude terms - "compound " -- not all readers have understanding of basic chemistry
 Fixed removed it, converted "amine compounds" to "trace amines, specifically" - more general, but still true.
Fixed removed it, converted "amine compounds" to "trace amines, specifically" - more general, but still true. - "notably" and "notable"-- used twice in the last paragraph of lead.
 Fixed 2nd -> prominent
Fixed 2nd -> prominent
I will look at rest of sections as I go along. From reading lead, consider reducing verbosity. I have this problem too. When I read back over things I have written I find I can reduce the word count by about 40% through rewording, without losing any actual content. This will reduce the overall length of the article and make it more approachable for readers. The lead especially should be clear and concise (see WP:LEAD). I also noted that the images used in this article are not standardized to thumbnails. I think this is in the MOS, let me check. Lesion (talk) 07:01, 1 December 2013 (UTC)
Lead Length
Does anyone agree that the lead could be a little shorter? We're currently at the maximum of four paragraphs mentioned in WP:Lead, but they're a little long (especially the first) and at times too thorough. Exercisephys (talk) 22:58, 7 February 2014 (UTC)
- I honestly think it's slightly vague in its present state (i.e., it could use more as opposed to less). The latter 2 paragraphs are pretty short as it is. Seppi333 (Insert 2¢ | Maintained) 23:15, 7 February 2014 (UTC)
Production statistics
I was looking for statistics like how much Amphetamine is produced/manufactured globally, legally, and an estimate of illegal production. I was unable to find this information in the article. Shouldn't this be included somewhere in the article ? --Siddhant (talk) 15:10, 19 February 2014 (UTC)
- The comparison of illicit production to meth is (supposed to be) contained in a large section of the sub-article - History and culture of amphetamines#Illicit drug culture. I'm still in the process of copyediting that article, as it's not organized to my satisfaction. Seppi333 (Insert 2¢ | Maintained) 00:22, 20 February 2014 (UTC)
- Edit:I'm not aware of any sources on legal production globally - would be hard to track; there's Rx statistics though. I may add this sometime soon if I find a good source for all amph pharmaceuticals in various countries. Seppi333 (Insert 2¢ | Maintained) 00:27, 20 February 2014 (UTC)
Structure
I think that the information presented in this article is sound; I would look more at the structure of the article. I feel that if the article was structured in more of a chronological order, it may be easier to interpret for those that don't know much about the content. Nicholas2015 (talk) 12:57, 27 February 2014 (UTC)
- @Nicholas2015: The user Seppi333 (talk · contribs) wants to stick directly to the WP:MEDRS guidelines. I haven't questioned it yet (there's some tension here at the moment), but I do agree that there are parts of it that don't suit this subject perfectly. If you have specific suggestions for changes we can consider them. Exercisephys (talk) 15:35, 27 February 2014 (UTC)
Toxicity
@Seppi333: I'm not trying to open old wounds here, but can you justify the continual distinction of "indirect neurotoxicity" from "direct neurotoxicity"? Also, I noticed that you used the term "indirect toxicity", which I find even further softened. I think that this phrasing is a bit of a POV-injection. Neurotoxicity is toxicity to neurons, no? I see the value in differentiating the two mechanisms, but I think that continually using the "indirect" qualifier suggests that it's less serious, or not "true" neurotoxicity. Exercisephys (talk) 19:18, 24 February 2014 (UTC)
- Exercisephys, def: https://sites.google.com/site/seppilurvespancakes/home/wikicontent/forep
- Both are toxicity to neurons. Direct neurotoxicity is blatantly obvious and really not hard to detect. It's what neurotoxicity is typically regarded as. Indirect NT is where another substance/medium causes the damage as either an indirect consequence of the compound in question, or as an interaction.
- Water is indirectly neurotoxic at high doses as a result of blood salt dilution - it causes brain damage (that's quite obviously neurotoxicity). Water is *not* a direct neurotoxin though.
- Amph is indirectly neurotoxic as a result of dopamine autoxidation - dopamine is oxidized, then damages dopamine neurons. If amph was oxidized and interacted with the cell, then IT would be causing the neurotoxicity, and hence it would be direct, since that would produce dose-dependent damage (positive correlation in the context of that ref).
- Probably the simplest way to consider the difference is this: what is the substance damaging the cell? The compound itself (direct) or is another substance involved (indirect)? Seppi333 (Insert 2¢ | Maintained) 21:47, 24 February 2014 (UTC)
- Just to show you that they're terms in common use, google what's inside the parentheses: ("Direct neurotoxicity" AND "indirect neurotoxicity"). Seppi333 (Insert 2¢ | Maintained) 22:19, 24 February 2014 (UTC)
- @Seppi333: I understand the definitions, I was just questioning the need to continually specify which is being referred to. I agree that there is no conclusive evidence that the chemical (RS)-1-phenylpropan-2-amine acts directly on human neurons to damage or kill them, and that should be mentioned in the article. However, in the context of a pharmaceutical like this, that isn't what "neurotoxic" means. Rather, it means that consumption of the compound can, by any mechanism, damage or kill neurons. To quote the neurotoxicity article, "[neurotoxicity] is generally used to describe a condition or substance that has been shown to result in observable physical damage."
- My real overarching concern is that the whole paragraph has, in my eyes, a subtle POV. It seems to spend most of its time disregarding amphetamine neurotoxicity as faux neurotoxicity, and then ends by mentioning in vitro neuroprotectant properties. That is itself a little dubious, as I remember being very vigorously shot down for mentioning in vitro evidence in our previous discussion. Moreover, it doesn't even seem like the source for that is MEDRS compliant. I sense a double standard being held against anything that I add to a page involving psychostimulants, and I feel like our current phrasing of amphetamine neurotoxicity is bending the truth. Exercisephys (talk) 23:39, 24 February 2014 (UTC)
- We don't have a single source that actually states amphetamine demonstrates any directly toxic actions. So what are you talking about "disregarding amphetamine neurotoxicity as faux neurotoxicity"? Is that what you think indirect neurotoxicity is - some trivial, fake toxicity? Seppi333 (Insert 2¢ | Maintained) 00:29, 25 February 2014 (UTC)
The section as it is basically says: low doses have a net positive cytoprotective/cytogenerative effect. High doses have a net cytotoxic effect. That seems exactly in line with what I would expect. If the compound were neurotoxic, it'd basically say low doses have a net cytotoxic effect. The page as is seems perfectly in line with clinical observations as well. Seppi333 (Insert 2¢ | Maintained) 00:37, 25 February 2014 (UTC)
After going over my edit, all I did that could actually concern you is remove the word "systematic". I'm kind of dumbfounded that you're expressing any concern over this. Besides the fact that we don't have any evidence to cite, it's just padding. Seppi333 (Insert 2¢ | Maintained) 00:45, 25 February 2014 (UTC)
- @Seppi333: This isn't due to recent changes, just a review of the wording. I don't know of any evidence for this statement: "low doses have a net positive cytoprotective/cytogenerative effect." The only evidence provided in the article is in vitro. Again, I'm really not trying to start a firing match. However, I think you're avoiding my central points:
- I don't see any need to continually specify amphetamine's neurotoxicity as "indirect" in this article, and in others.
- The paragraph's thesis seems to involve downplaying possible toxicity.
- Is the in vitro neuroprotective information and its corresponding citation MEDRS compliant? If not, doesn't that suggest a double standard to you?
- Exercisephys (talk) 01:35, 25 February 2014 (UTC)
- It's necessary to specify that it's indirect because people have the misconception that this compound is neurotoxic. If that misconception weren't rampant, I'd agree with you that it's unnecessary to specify.
- The paragraph is downplaying direct neurotoxicity for two reasons: 1) we have no evidence of any, 2) the reason above this one.
- The in vitro evidence pertains to CART, which doesn't even have an identified receptor. The evidence on that is preclinical. Similarly, the entire addiction/genetics section I just added is also preclinical and based upon animal studies. These sections need to be updated to the associated clinical evidence when it comes available, but as of right now, they're the most current evidence on these topics. As there's already clinical evidence on the issue related to the neurotoxicity, we use clinical evidence as opposed to preclinical evidence, since it's more current. That's just what MEDRS says - use the most current evidence available that's related to humans. Just to be clear, the entire pharmacodynamics section is more or less a mix of preclinical and clinical evidence weaved together, but its the most up-to-date and human-relevant evidence on the compound, that's what matters. Seppi333 (Insert 2¢ | Maintained) 01:47, 25 February 2014 (UTC)
- @Seppi333: "people have the misconception that this compound is neurotoxic" ...it is (most probably) neurotoxic; it's indirectly neurotoxic. That's the point I've been making this whole time. In the context of pharmacology, indirectly neurotoxic = neurotoxic. People don't care whether it's the chemical itself doing the damage, they care whether the damage is done. That's what I've been saying this whole time. That's why I subsequently think it's unnecessary to use the qualifier "indirect" after you've already specified that the neurotoxicity happens through indirect mechanisms. Exercisephys (talk) 03:58, 25 February 2014 (UTC)
@Exercisephys: Look, ignoring the statistical definition, here's what those two concepts boil down to:
- Direct - The compound damages a cell in the process of interacting with it. (positive dose-dependent toxicity ---> lots of damage with lots of compound concentration) [A direct neurotoxin is a neurotoxin. ]
- Indirect - The compound damages a cell in overdose via a mechanism which is not endemic to the compound itself. [An indirect neurotoxin is just a compound with a toxicity threshhold.]
Water, all neurotransmitters, all minerals, all vitamins, etc are indirect neurotoxins. That 2 part definition prevents virtually every substance from being called a "neurotoxin" because the unqualified definition is literally just '"toxic" to a neuron.' Is this registering?
If you call amphetamine a neurotoxin, you can't explain to me why water isn't a neurotoxin given the way you're defining neurotoxicity. Seppi333 (Insert 2¢ | Maintained) 04:08, 25 February 2014 (UTC)
- @Seppi333: The dose :P
- You need an absurd amount of water to kill brain cells. But, by my definition, it would be okay to call hyponatremia or hyperhydration neurotoxic. Current evidence suggests that a pretty standard recreational amphetamine dose can be neurotoxic, so it's fair to say that supratherapeutic amphetamine doses are probably neurotoxic. Exercisephys (talk) 04:38, 25 February 2014 (UTC)
@Exercisephys: Defining a neurotoxin by relative toxic dose is completely arbitrary.
- Ah yes, that current evidence - the one conducted and authored by Wikipedia elementary school? (You say that like I'm some uninformed reader of this article - wtf are you talking about?) And no, water is the neurotoxin, hyponatremia is a condition. Just as dopamine would be a neurotoxin and autoxidative stress being the condition given your definition paradigm. Seppi333 (Insert 2¢ | Maintained) 04:51, 25 February 2014 (UTC)
- I don't know why you're all of the sudden going off the wall about this section once again, but this is what it boils down to: we're not changing jack shit in this section unless we get new sources like pharm databases or journals/books published from 2009 onward, on humans, and specifically, humans using L-amphetamine/D-amphetamine; i.e., the same way it's always been with this section (and the rest of the article where medical claims are made...).Seppi333 (Insert 2¢ | Maintained) 04:57, 25 February 2014 (UTC)
Toxicity - cont
Hey, guys. I think there's a bug in the section-adder, as this title wasn't initially added. It's probably due to the fact that I tried to put Wikilinks in it. I'll report that.
Anyway, I guess the subject of this wasn't clear, as the facepalm of the ever respectful, dispassionate, and open-minded Seppi333 (talk · contribs) noted.
Original post:
The toxicity section should also discuss these aspects. There's a good source here: http://link.springer.com/article/10.1007/s00204-012-0815-5/fulltext.html
If anyone needs access, let me know. Exercisephys (talk) 15:59, 25 February 2014 (UTC)
![]() Facepalm Seppi333 (Insert 2¢ | Maintained) 17:18, 25 February 2014 (UTC)
Facepalm Seppi333 (Insert 2¢ | Maintained) 17:18, 25 February 2014 (UTC)
Wait, I just realized that you removed the title, Seppi333 (talk · contribs). Whydju do that? I'm just trying to improve this article, dude. Exercisephys (talk) 16:25, 26 February 2014 (UTC)
- Look, I have no clue why you're going off and trying to put crap about animals and methamphetamine into this article again, but the standard you need to match for this section is this: Methamphetamine#Neurotoxicity. Notice how the quote is quite clearly talking about human meth abusers and not some lab rat with a conditioned place preference.
- On a different note, I pruned out a lot of the crap that you said you didn't like (e.g., "direct" vs "indirect" toxicity and the statement on CART) - what issue do you have with this now? Seppi333 (Insert 2¢ | Maintained) 23:35, 28 February 2014 (UTC)
- Just for the record, the sources do not support a direct statement about amphetamine and dopamine autoxidation. That's WP:SYNTH that I knowingly added in an attempt to placate you on the grounds of WP:IGNOREALLRULES. Is that seriously not enough for you? I'm not going to allow ANYTHING to be added to this article that even remotely implies it's a neurotoxin without actual evidence of that. Seppi333 (Insert 2¢ | Maintained) 23:41, 28 February 2014 (UTC)
- Also, Exercisephys, before you throw that source back at me, LOOK AT THE PAPERS ITS CITING WHEN IT SUGGESTS "XYZ IS NEUROTOXIC." I can't tell whether you're intentionally and knowingly trying to put POV in this article, or you just don't know any better, but I'm really running out of patience. Seppi333 (Insert 2¢ | Maintained) 23:44, 28 February 2014 (UTC)
I suggest before re-adding anything potentially controversial back into this article, we try to achieve consensus here on the talk page. I think both of you are making some good points. Toxicity is toxicity whether it is by a direct or indirect mechanism. On the other hand, toxicity is not clinically relevant if it occurs only at doses significantly higher than patents are likely to be exposed to. The key point of course is whether there are MEDRS compliant sources that would directly support a conclusion one way or the other. I am not at all familiar with the amphetamine toxicity literature. I will read through the available secondary literature and try to offer some suggestions. Boghog (talk) 01:22, 1 March 2014 (UTC)
- @Boghog: Okay, we first need to establish that the two-clause section Seppi333 keeps adding is ridiculous and reactionary. Animal results are mentioned in all medical treatments of amphetamine toxicity because human toxicity can't be studied well (due to medical ethics and methamphetamine's prevalence). Furthermore, the section I keep restoring is the result of the previous discussion's consensus, with a single additional sentence that simply specifies what kind of toxicity occurs in animals (which was already mentioned). He also went through and systematically removed a bunch of other stuff that I added. Basically, he's just losing his temper and trying to get me mad.
- I'm not trying to inject POV or "trash the substance". I just think that leaning so heavily on the distinction between direct and indirect neurotoxicity distracts the reader from the fact that amphetamine can in fact damage neurons in recreational doses. In the medical context, people don't care how it happens, just whether it happens. Mentioning the distinction is important (if it does exist, which I'll discuss later), doting on it is bias.
- It's generally just tiresome to have Seppi333 straw-man my arguments and insult me. He generally continually reverts any change I make and then starts a war of time-attrition that he usually wins. We need someone else working on this article at least semi-regularly. Seppi333 does a good job, but he takes far too much ownership, isn't open to correction, and takes challenges personally. This conflict is tiresome, but I think this it's important that people get accurate information about substances' dangers.
- This is a valuable read. Seppi333 does have a subtle bias because he's "been using it for about 14 years or so, and [his] brain still isn't fried yet. :P". That's okay, I've used amphetamine medically too. But I think it affects his wording and the way he interprets sources.
- I don't entirely buy the idea that amphetamine is proven not to be directly neurotoxic. That one textbook says so, but I haven't actually seen a study stating that. If I recall correctly, Seppi333 couldn't find a source from the textbook itself. I therefore think we should do more research before adding that to the article, but that's the fact closest to Seppi333's heart and he's been very successful at stymieing any changes to it.
- Here's what I suggest:
- First and foremost, for the love of god, let's stop the reversion nonsense and work from the previous consensus (what I've been restoring).
- Lets agree on a general treatment of animal and in vitro data that applies to things casting things in both a positive and negative light (e.g. primate neurotoxicity and CART neuroprotection). This also applies to stymieing over minor MEDRS guidelines.
- Let's review what data is available where, and focus on the general tone of the available literature rather than quote-pulling.
Seppi's response
|
|---|
Bullshit
No, you just annoyed me to the point that I stopped caring about offending you by editing text you've added. You made it abundantly clear (with two sections from different occassions on my talk page) that you don't like it when I edit content you add to articles. Why did I delete a clause stating that amph and meth toxicity are indistinguishable? Because that comparison is nothing but trivia/textual padding to the 99.9% of readers that know nothing about meth addiction.
Besides the fact that I already acknowledged this months ago to WP:MED when I was a new editor, I don't see how this could possibly constitute a COI for ANY editor unless I/he/she were an addict. Perhaps you've completely missed the adverse effects and overdose sections, which are far more detailed than they were before I started working on this article.
No, I just never looked. |
Seppi333 (Insert 2¢ | Maintained) 02:55, 1 March 2014 (UTC)
Also, Exercisephys, before you throw that source back at me, LOOK AT THE PAPERS ITS CITING WHEN IT SUGGESTS "XYZ IS NEUROTOXIC." I can't tell whether you're intentionally and knowingly trying to put POV in this article, or you just don't know any better, but I'm really running out of patience. -Seppi333
- @Boghog: Not to get too polemical, but this is the stuff that is just goofy. I site a well-regarded MEDRS review, and he questions the sources cited by it. Meanwhile, his information source for amphetamine not being directly neurotoxic is an uncited anecdotal mention in a section about meth in a general subject textbook, and a link to a toxicity site that (the best I can tell) doesn't mention direct neurotoxicity at all. Exercisephys (talk) 02:59, 1 March 2014 (UTC)
- The point of that statement was for you to observe which of the "amphetamines" substances the author is referring to. It had nothing to do with casting doubt on the validity of a paper.
- "Molecular Neuropharmacology: A Foundation for Clinical Neuroscience" doesn't have a section on meth. Also, molecular neuropharmacology is a pretty general subject, right?
- "That website", i.e., Hazardous Substances Data Bank, is a comprehensive toxicology database. Like you said, funny how it doesn't have a neurotoxicity statement, right?Seppi333 (Insert 2¢ | Maintained) 03:14, 1 March 2014 (UTC)
- @Boghog: Not to get too polemical, but this is the stuff that is just goofy. I site a well-regarded MEDRS review, and he questions the sources cited by it. Meanwhile, his information source for amphetamine not being directly neurotoxic is an uncited anecdotal mention in a section about meth in a general subject textbook, and a link to a toxicity site that (the best I can tell) doesn't mention direct neurotoxicity at all. Exercisephys (talk) 02:59, 1 March 2014 (UTC)
- (And things like the fact that he said it's "bullshit" that studying human toxicity is hard, when most reviews acknowledge this, it's common sense, and he himself acknowledged it in the first consensus discussion.) Exercisephys (talk) 03:02, 1 March 2014 (UTC)
- Neuroimaging is very difficult.[1] Seppi333 (Insert 2¢ | Maintained)
- (And things like the fact that he said it's "bullshit" that studying human toxicity is hard, when most reviews acknowledge this, it's common sense, and he himself acknowledged it in the first consensus discussion.) Exercisephys (talk) 03:02, 1 March 2014 (UTC)
References
- ^ Krasnova IN, Cadet JL (May 2009). "Methamphetamine toxicity and messengers of death". Brain Res. Rev. 60 (2): 379–407. doi:10.1016/j.brainresrev.2009.03.002. PMC 2731235. PMID 19328213.
Neuroimaging studies have revealed that METH can indeed cause neurodegenerative changes in the brains of human addicts (Aron and Paulus, 2007; Chang et al., 2007). These abnormalities include persistent decreases in the levels of dopamine transporters (DAT) in the orbitofrontal cortex, dorsolateral prefrontal cortex, and the caudate-putamen (McCann et al., 1998, 2008; Sekine et al., 2003; Volkow et al., 2001a, 2001c). The density of serotonin transporters (5-HTT) is also decreased in the midbrain, caudate, putamen, hypothalamus, thalamus, the orbitofrontal, temporal, and cingulate cortices of METH-dependent individuals (Sekine et al., 2006) ...
Neuropsychological studies have detected deficits in attention, working memory, and decision-making in chronic METH addicts ...
There is compelling evidence that the negative neuropsychiatric consequences of METH abuse are due, at least in part, to drug-induced neuropathological changes in the brains of these METH-exposed individuals ...
Structural magnetic resonance imaging (MRI) studies in METH addicts have revealed substantial morphological changes in their brains. These include loss of gray matter in the cingulate, limbic and paralimbic cortices, significant shrinkage of hippocampi, and hypertrophy of white matter (Thompson et al., 2004). In addition, the brains of METH abusers show evidence of hyperintensities in white matter (Bae et al., 2006; Ernst et al., 2000), decreases in the neuronal marker, N-acetylaspartate (Ernst et al., 2000; Sung et al., 2007), reductions in a marker of metabolic integrity, creatine (Sekine et al., 2002) and increases in a marker of glial activation, myoinositol (Chang et al., 2002; Ernst et al., 2000; Sung et al., 2007; Yen et al., 1994). Elevated choline levels, which are indicative of increased cellular membrane synthesis and turnover are also evident in the frontal gray matter of METH abusers (Ernst et al., 2000; Salo et al., 2007; Taylor et al., 2007).
- @Seppi333: I don't see a single mention of AMPH in that ref. Exercisephys (talk) 03:59, 1 March 2014 (UTC)
- It's the meth ref on neurotoxicity. The point was that it was demonstrated via neuroimaging. Seppi333 (Insert 2¢ | Maintained) 04:05, 1 March 2014 (UTC)
- @Seppi333: I don't see a single mention of AMPH in that ref. Exercisephys (talk) 03:59, 1 March 2014 (UTC)
- @Seppi333: That's not what I'm asking for. What I'm asking for is a single source (other than that offhanded anecdotal sentence) stating that amphetamine is proven not to be a direct neurotoxin in humans. I haven't seen one, and I've looked. I also haven't been provided one from you, though I've asked.
- Where was this research done? Who did it? How was it determined? You seem extremely sure of this fact and yet I don't know any of these details. Exercisephys (talk) 06:08, 1 March 2014 (UTC)
@Exercisephys: I've been sure of it because I know that those three researchers all have an interest in various psychostimulant-related topics. I.e., I know for a fact that all three actively do research with amphetamine. Look for their publications (not the textbook) in this article if you don't believe me. Nestler in particular is purely focused on the genetic aspects of psychostimulant addiction. In any event, after I last posted, I started searching through toxicology databases for more information. I'm sure you'll be as pleased as I am after reading this:
http://projectreporter.nih.gov/project_info_description.cfm?aid=8429516&icde=0
It's oddly good timing and rather amusing that this study ended yesterday (This research started in 2009 and was initially slated to end April 2014, but was rescheduled to end Feb 28th 2014): http://projectreporter.nih.gov/project_info_details.cfm?aid=8429516&icde=0
And lastly, this is a related paper he published on this topic in 2005: http://jpet.aspetjournals.org/content/315/1/91.full
I'm going to email the researcher tomorrow and ask about the results ahead of any publications. His results will settle our content dispute. Seppi333 (Insert 2¢ | Maintained) 06:44, 1 March 2014 (UTC)
@Exercisephys: I'll email Drs. Nestler, Hyman, and Malenka about that statement while I'm at it. Seppi333 (Insert 2¢ | Maintained) 06:52, 1 March 2014 (UTC)
- I will point out though that this is the very same researcher who published the controversial, retracted MDMA neurotoxicity paper. Seppi333 (Insert 2¢ | Maintained) 06:58, 1 March 2014 (UTC)
- Again, I'm not trying to be a jerk, but there is a double standard here. You spent a long time treating me like a senseless moron that was wasting your time by injecting POV into this article. However, now that we're reviewing the evidence for amphetamine lacking neurotoxicity, we have:
- an anecdotal mention in a general textbook.
- an unfinished clinical trial by a researcher of questionable integrity, who hypothesized that the trial will show neurotoxicity.
- possible future personal correspondence with researchers.
- Again, I'm not trying to be a jerk, but there is a double standard here. You spent a long time treating me like a senseless moron that was wasting your time by injecting POV into this article. However, now that we're reviewing the evidence for amphetamine lacking neurotoxicity, we have:
- I just don't see what makes this conclusion bullet-proof, much less worthy of being in an article of MEDRS standards. Am I missing something? Exercisephys (talk) 19:24, 1 March 2014 (UTC)
Thanks @Exercisephys: and @Seppi333: for brining me up to speed. It seem to me that part of this dispute revolves around what exactly WP:MEDRS allows and disallows. I think everyone is in agreement that to the greatest extent possible, human studies should be cited in preference to animal or in vitro studies. However I think toxicology is a special case. For ethical reasons, humans toxicology data is generally not available (I think this and this discussion where it was proposed to modify MEDRS to specifically address toxicology is especially relevant). While animal toxicity experiments are imperfect models of human toxicity, they are often the best and only data we have. Hence I think including animal toxicology studies that are discussed in secondary sources should be allowed. Boghog (talk) 19:45, 1 March 2014 (UTC)
- @Boghog: Thanks for the input. More specifically, what do you think about the statement that amphetamine is known not to be a direct neurotoxin? Do you think the evidence is sufficient? If not, will you help us word a passage that expresses the ambivalence of current research? Exercisephys (talk) 19:52, 1 March 2014 (UTC)
- @Exercisephys: Proving a negative is very difficult. There is lack of evidence that amphetamine is a direct neurotoxin, but this of course is different than saying amphetamine is known not to be a direct neurotoxin. Hence I would suggest replacing "amphetamine is not directly neurotoxic in humans" with something like "there is no evidence that amphetamine is directly neurotoxic in humans".
- I also wanted to point out that while the terms direct and indirect (or primary and secondary) toxicity are widely used, there is no universally accepted definition of what meant by these terms. The definitions are context dependent. In the context of amphetamine toxicity, I think the definitions provided above are reasonable but they need to be made explicit in the article because it is not a prior obvious what is implied by these terms. There is also an implicit assumption in the above discussion that indirect toxicity is less of a concern, because presumably it requires higher exposures of drug to manifest itself. This may be true, but it is not true by definition. Boghog (talk) 11:32, 2 March 2014 (UTC)
After spending a stupid amount of time searching for and reading papers, I've basically discovered that there's evidence of indirect amphetamine neurotixicity in humans which is analogous, although milder, than methamphetamine neurotoxicity. What's interesting it that it only seems to manifest with cognitive dysfunction in addicts. Makes me wonder about just how deep the connection between neurotoxicity, (adverse) neuroplasticity and addiction are;† this is OR, but to give you an example of how interrelated these are, there's some clear connections in reviews, but I need to read more of the papers I spent hours sifting through and downloading before I add anything else to the article. I should emphasize that this is indirect neurotoxicity simply because therapeutic use of ADHD stimulants (incl. amph) produces the opposite histological and biomarker changes as methamphetamine neurotoxicity. (read the quote in the reflist) It DOES produce *some* of those changes in abuse conditions though, based upon what I've read so far. E.g., it can compromise the BBB through adverse effects on gene expression from heightened oxidative stress (meth apparently has a more direct impact on BBB integrity). Also can reduce gray matter volume in overdose (the reverse is evident at therapeutic doses - see the refs named "neuroplasticity" in the source). Amph sensitization also doesn't occur at therapeutic doses, which is additional evidence that it doesn't adversely affect the DA/NE neurotransmitter systems. I'm too lazy to cite specific papers, but if you're curious about a particular claim, just ask me for the ref. Seppi333 (Insert 2¢ | Maintained) 10:50, 2 March 2014 (UTC)
- †
 Note: This is my OR/Synth; it agrees with the sources I've read though: To give you an idea of how interrelated these seem, ΔFosB is dose-dependently upregulated by amph throughout the brain during chronic use (see the addiction section for reference. Also note the top interacting gene in this link.), including the hippocampus, which results in dose-dependent neurogenesis (I think it's both absurd and amusing that amphetamine is indirectly neurotoxic, neuroprotective, AND neurogenerative at abused doses in rats). This neuroprotection/neurogenesis doesn't seem to be related to CART either, if only because its known to be ΔFOSB mediated. It probably applies to humans as well given the similarity between human/mouse amphetamine-mediated FOSB upregulation and its resulting effects: ref PMID 23178911 ).
Note: This is my OR/Synth; it agrees with the sources I've read though: To give you an idea of how interrelated these seem, ΔFosB is dose-dependently upregulated by amph throughout the brain during chronic use (see the addiction section for reference. Also note the top interacting gene in this link.), including the hippocampus, which results in dose-dependent neurogenesis (I think it's both absurd and amusing that amphetamine is indirectly neurotoxic, neuroprotective, AND neurogenerative at abused doses in rats). This neuroprotection/neurogenesis doesn't seem to be related to CART either, if only because its known to be ΔFOSB mediated. It probably applies to humans as well given the similarity between human/mouse amphetamine-mediated FOSB upregulation and its resulting effects: ref PMID 23178911 ). - Exercise upregulates ΔFosB in the hippocampus as well, and that's one of the mechanisms by which it produces beneficial changes (see the bottom of my userpage or the relevant exercise article) in brain structure PMID 18493951 PMID 24282574 PMID 10448191
- Although the neurogenesis study suggests FOSB activation isn't correlated with the neurogenesis, based upon the strong evidence from other papers/reviews (some are cited above), I think the reserachers might've just sampled the wrong cells for ΔFosB-mediated hippocampal neurogenesis (plausible, since the mechanism of ΔFosB in hippocampal neurogenesis is unknown).Seppi333 (Insert 2¢ | Maintained) 10:50, 2 March 2014 (UTC)
- I noticed you guys going back and forth on this and thought I would drop by and see if I could add a different perspective that might help you resolve this. I haven't read everything above in detail, but I wonder if trying to break this into a binary "is/is not" neurotoxic issue is a little artificial and that's why you can't reach an agreement. Is amphetamine neurotoxic? Absolutely. Take a plate of cultured neurons and cover them with 10% aqueous amphetamine hydrochloride. They'll all die. This is obviously a reducto ad absurdum argument, but my point is that everything is neurotoxic depending on the dose. You need to formulate a more precise question.
- I think meaningful questions would be 1) Are cognitive or other neuropsychiatric deficits observed in long term studies of ADHD patients treated with therapeutic doses of amphetamine, and 2) Are such deficits seen in long term abusers exposed chronically to high doses? The animal, in vitro, and imaging studies really seem to me to be sort of a "how many angels can dance on the head of a pin" issue. They aren't really clinical outcomes, and it is outcomes that people care about. If there is no clear answer in the literature regarding cognitive effects of long term use in humans, I would suggest simply noting that fact and moving on.
- Anyway, I don't know if this comment will be helpful or just irritating. Hopefully the former. Formerly 98 (talk) 12:20, 2 March 2014 (UTC)
- I don't think anyone is going to argue that amphetamine is not indirectly neurotoxic (we all agree it has indirect toxicity mechanisms). The histological changes produced by therapeutic use of amphetamine are overall neurogenerative though; this is in contrast to meth which does the opposite at moderate-high doses in humans. In any event, we just don't have any evidence to claim it's a direct neurotoxin; I've found lots of sources for indirect neurotoxicity during my day-long dive into subst. amph. toxicity research yesterday.Seppi333 (Insert 2¢ | Maintained) 18:39, 2 March 2014 (UTC)
Neurotoxicity - cont. (2)
- The best evidence of any human DA neurotoxicity I have found so far
http://www.ncbi.nlm.nih.gov/pubmed/23415394
This is very weak (and only marginally significant - p=.05) neurotoxicity given that:
- some participants had some polydrug use
- dose range: ".5g-3g" per occassion. [the minimum of .5g is about 10x the maximum therapeutic dose] A full gram was the average dose used
- the average amount of time that d-amph was used recreationally by the study participants was over a decade:" 13.9 (±8.7))
- The most annoying thing about this study, to me, is that it didn't compare the effect of normal doses of d-amph with MPH in healthy users, which they probably didn't do because it would show the same effect as MPH; they made the (dose-unspecified) claim, "We also predicted that dAMPH users would show an altered performance on tests of attention, memory and executive function." In other words, it just reads like they're trying to avoid evidence to the contrary to "prove" their hypothesis.
- Edit/add, I noticed this study was published earlier than the above paper by the same authors - http://www.ncbi.nlm.nih.gov/pubmed/23296186 - No clue why this wasn't mentioned to any extent Seppi333 (Insert 2¢ | Maintained) 08:00, 5 March 2014 (UTC)
- Should probably add that this isn't evidence of a direct form of toxicity. Seppi333 (Insert 2¢ | Maintained) 07:53, 5 March 2014 (UTC)
This study - PMID 17049170 - is very clearly asserting that the neurotoxic effects of amphetamine are dose-dependent above some threshold (as I've suggested since I wrote about it here), based upon their data. There's also a review, PMID 24440369, which cites it (the article/citation name itself supports the claim). Seppi333 (Insert 2¢ | Maintained) 08:53, 5 March 2014 (UTC)
- It's kind of sad that I never read the full abstract of this review - I ignored it because it's 7 years old. PMID 17606768 "Imaging studies of ADHD-diagnosed individuals show an increase in striatal dopamine transporter availability that may be reduced by methylphenidate treatment." Seppi333 (Insert 2¢ | Maintained) 18:32, 5 March 2014 (UTC)
@Exercisephys: Err...this was my bad. I thought I shared this with you like a week or two ago EP. PMID 21886562. Added that to meth a while back. That's 1 reason it has a greater neurotoxic potential. Found another review showing detectable acute neurotoxicity in humans using large binge doses. PMID 19897075
MPH is a sigma agonist as well. Amph has no detectable binding affinity for sigmas based upon Binding DB's data. Seppi333 (Insert 2¢ | Maintained) 00:11, 24 March 2014 (UTC)
Neuroplasticity
- @Seppi333: Why were the Volkow primate studies removed? Exercisephys (talk) 19:48, 3 March 2014 (UTC)
There's a plethora of clinical evidence on neuroplasticity and therapeutic ADHD psychostimulant use. I found another meta analysis to tack onto that section. Going to put it in when I expand toxicity. Busy irl lately. Seppi333 (Insert 2¢ | Maintained) 20:04, 3 March 2014 (UTC)
Same here, to a frightening degree. I'll have some time in a few days. Exercisephys (talk) 17:27, 5 March 2014 (UTC)Busy irl lately. -Seppi333
5-HT toxidrome
@Dosenfant:, instead of edit-warring over the inclusion of this phenomenon, I'm starting this thread.
I'd be happy to give you a detailed explanation, with citation, of the toxicodynamics of amphetamine-induced serotonin toxidrome. [Edit/add: for a simple comparison, amphetamine acts analogously to an SSRI, except: it reduces postsynaptic 5-HT firing rate/action potentials (produces a less potent effect in comparison to SSRIs), but effluxes 5-HT into the synaptic cleft via PKC signaling (produces a more potent effect in comparison to SSRIs).] In any event, the relevant text from the body (not the abstract) of the paper from my recent revert is below (emphasis added):
2 Stimulants
2.1 Amphetamines
Amphetamine is the common name for the racemic mixture of b-phenylisopropylamine or a-methylphenylethylamine [11]. Substitutions of the phenylethylamine result in the creation of different amphetamine analogs, which are also described using the term ‘amphetamines’. Currently available prescription amphetamines include amphetamine, lisdexamphetamine, phentermine, phendimetrazine, and dextroamphetamine. Because lisdexamphetamine is rapidly converted to dextroamphetamine in the blood, it is reviewed in this section.
...2.1.2 Mechanism of Toxicity
The mechanism of toxicity of amphetamines is primarily related to excessive extracellular dopamine, norepinephrine, and serotonin [22, 23]. The most prominent clinical picture is alpha- and beta-adrenoreceptor-mediated sympathomimetic syndrome, with psychiatric symptoms and hyperthermia secondary to the dopamine and serotonin excess [23–26].
— Overdose of drugs for attention-deficit hyperactivity disorder: clinical presentation, mechanisms of toxicity, and management, PMID23757186
Seppi333 (Insert 2¢ | Maintained) 17:04, 18 March 2014 (UTC)
- True statement, like birds include species who can fly. But you can't conclude that all birds are able to fly. Amphetamines are a superset that contains amphetamine, MDMA, and much more. A "primarily related to" statement about this superset isn't neccesary true for amphetamine (without the s). Like a Kiwi can't fly although flying is primarily related to birds. I sligthly changed bold letters in your cite, to emphasize the difference between amphetamine and amphetamines (different articles!). --Richard (talk) 17:56, 18 March 2014 (UTC)
- I cited the sentence "Currently available prescription amphetamines include amphetamine, lisdexamphetamine, phentermine, phendimetrazine, and dextroamphetamine." Because those are the drugs this review is talking about specifically.
- I cited the article title itself and bolded it - Overdose of drugs for attention-deficit hyperactivity disorder: clinical presentation, mechanisms of toxicity, and management, PMID 23757186 - because, among the aforementioned drugs, amphetamine, d-amph, and lisdexamfetamine are the only drugs among that group which are prescribed for ADHD.
- Consequently, you can't argue that this isn't referring SPECFICALLY to amphetamine and its enantiomers. Seppi333 (Insert 2¢ | Maintained) 18:07, 18 March 2014 (UTC)
- Yes, the review aims at prescription amphetamines. But even in a review about birds from africa, the statement some birds can fly doesn't exclude kiwis. Therefore must be written all birds in africa can fly.
- And do you know, is (only) lisdexamphetamine a bad serotonin toxic guy, because it acts on 5-HTP before it's metabolized, which matters only in overdoses? Respect WP:NOR. --Richard (talk) 18:19, 18 March 2014 (UTC)
- ...Lisdexamfetamine isn't even pharmacologically/biologically active. It has no pharmacodynamic action at all. Read this article for the corresponding statement/reference.Seppi333 (Insert 2¢ | Maintained) 18:22, 18 March 2014 (UTC)
- I guess that's right, but we are both guessing it concerning serotonin effects in overdose use.
- check the cited sources, anything else conflicts with WP:NOR.
- 22. Hoffman BB, Lefkowitz RJ. Catecholamines, sympathomimetic
- drugs, and adrenergic receptor antagonists. In: Hardman JG,
- Limbird LE, Molinoff PB, et al., editors. Goodman and Gil-
- man’s the pharmacological basis of therapeutics. 9th ed. New
- York: McGraw-Hill; 1996. p. 199–227.
- 23. Chiang WK. Chapter 75. Amphetamines. In: Hoffman RS,
- Nelson LS, Goldfrank LR, Howland MA, Lewin NA, Flomen-
- baum NE, editors. Goldfrank’s toxicologic emergencies. 9th ed.
- New York: McGraw-Hill; 2011. http://www.accessemergency
- medicine.com/content.aspx?aID=6520715. Accessed 14 January
- 2013.
- --Richard (talk) 18:25, 18 March 2014 (UTC)
- ...Lisdexamfetamine isn't even pharmacologically/biologically active. It has no pharmacodynamic action at all. Read this article for the corresponding statement/reference.Seppi333 (Insert 2¢ | Maintained) 18:22, 18 March 2014 (UTC)
Sigh...ok, look; I wrote that entire section, so I obviously read all these references, as I cited every review/medical source in that section (in addition to the vast majority of the rest of the article...); I therefore know exactly what citation references each symptom. The above source asserts 5-HT overdose in a section titled "mechanisms of toxicity." I don't need anything more specific/direct to support that assertion because it's the definition of 5-ht toxicity syndrome, which is a toxic concentration of synaptic 5-ht. Seppi333 (Insert 2¢ | Maintained) 18:58, 18 March 2014 (UTC)
- Are confusing writing the section with doing WP:PRIMARY research? It's honorable that you write a lot, but it doesn't matter how many edits you have, if your thesis is just a belief without appropriate proof, as it is in the hypotheses of an amphetamine's serotonin syndrom (not just contribution of serotonin effects).
- --Richard (talk) 21:38, 18 March 2014 (UTC)
- I'm confused as to why you don't think "The most prominent clinical picture is alpha- and beta-adrenoreceptor-mediated sympathomimetic syndrome, with psychiatric symptoms and hyperthermia secondary to the dopamine and serotonin excess" supports serotonin toxidrome. That statement is even a perfect match with the lead of serotonin syndrome. A much more concise way to write that sentence is it presents as adrenergic storm (i.e., norepi/epinephrine toxidrome), serotonin toxidrome, and "dopamine toxidrome" (there's no analogous syndrome/concept defined for this). It would be OR if I said that this "due/likely due to TAAR1's inhibitory effects of DA/5-HT neuronal firing, but not on NE neuronal firing." Seppi333 (Insert 2¢ | Maintained) 22:25, 18 March 2014 (UTC)
- No, it's not a pefect match, a serotonin syndrom is not just an excess of serotonin. Otw. e.g. MDMA users would always have a serotonin syndrom, because the use of MDMA causes an excess of serotonin. But unless combined with other drugs like MAOI it isn't notorious for serotonin syndrom. If you change your contribution to "an excess of serotonin" (add "and related symptoms" if you want) instead of serotonin syndrom/toxidrome, then I'm pleased. --Richard (talk) 22:48, 18 March 2014 (UTC)
- If you want to get a feeling for the difference, read Death of Libby Zion (R.I.P.), and compare it with the prominent symptoms a usual MDMA excess raver. --Richard (talk) 22:59, 18 March 2014 (UTC)
- I'm confused as to why you don't think "The most prominent clinical picture is alpha- and beta-adrenoreceptor-mediated sympathomimetic syndrome, with psychiatric symptoms and hyperthermia secondary to the dopamine and serotonin excess" supports serotonin toxidrome. That statement is even a perfect match with the lead of serotonin syndrome. A much more concise way to write that sentence is it presents as adrenergic storm (i.e., norepi/epinephrine toxidrome), serotonin toxidrome, and "dopamine toxidrome" (there's no analogous syndrome/concept defined for this). It would be OR if I said that this "due/likely due to TAAR1's inhibitory effects of DA/5-HT neuronal firing, but not on NE neuronal firing." Seppi333 (Insert 2¢ | Maintained) 22:25, 18 March 2014 (UTC)
![]() Note:To keep this conversation in one place, reply at: WT:MED#WP:SYNTH on amphetamine articles
Note:To keep this conversation in one place, reply at: WT:MED#WP:SYNTH on amphetamine articles
Shudde
@Shudde: Continue your review here. Seppi333 (Insert 2¢ | Maintained) 06:55, 24 April 2014 (UTC)
- PS: It shouldn't take you two full months to review this article. Seppi333 (Insert 2¢ | Maintained) 06:57, 24 April 2014 (UTC)
- There are plenty of comments at the recent FAC that probably need to be fully addressed. My comments there should be taken as guidance and examples of what further work is required, rather than a point by point list of problems. I'm not going to repeat all those here as it's not necessary. I'll repeat a couple of my concerns though, and will wait until these have been adequately addressed before giving the article another read through.
- There is Wikipedia:Citation overkill in this article, I'm not sure why we need a citation every single sentence rather than following this guideline. I don't know of another article that insists on at least one inline citation every sentence. As the essay says as per WP:PAIC, citations should be placed at the end of the passage that they support. If one source alone supports consecutive sentences in the same paragraph, one citation of it at the end of the final sentence is sufficient. It is not necessary to include a citation for each individual consecutive sentence, as this is overkill.
- I'm seeking consensus on WT:MED at the moment. You're welcome to participate. The citation style will only follow what what is supported there. Seppi333 (Insert 2¢ | Maintained) 12:31, 27 May 2014 (UTC)
- Comment: I think reviewer needs to recognise here that WP:Citation overkill is merely an essay, not a "guideline". 86.181.67.132 (talk) 15:36, 28 May 2014 (UTC)
- I'm seeking consensus on WT:MED at the moment. You're welcome to participate. The citation style will only follow what what is supported there. Seppi333 (Insert 2¢ | Maintained) 12:31, 27 May 2014 (UTC)
- Try and fix overlinking (WP:OVERLINK). As Tony1 says in User:Tony1/Build your linking skills -- It is only over the past few years that we have begun to realise the potential for refining wikilinking—how sophisticated decision-making is required to achieve a high standard of linking: what to link, what not to link, how and when to research more focused links, and how to integrate links smoothly into the text. In this respect, linking deserves attention just as does the prose in our articles. I'd recommend at least reading Tony1's guide on this before deciding what to link or not link. We've also got a large number of duplicate links.
- I've addressed this to a max of 2 WL's/term using AWB. Seppi333 (Insert 2¢ | Maintained) 12:31, 27 May 2014 (UTC)
- There is a lot of jargon and technical language that needs to be reduced in order to increase accessibility. At the moment the article reads like it is written for an MD rather than a general audience. There are plenty of high quality references for those that want technical details -- also notes can help with this, giving more information than the general reader would require. Wikipedia:Manual of Style/Medicine-related articles expresses my concerns well. I'll point to the section Technical terminology, and also to the section Signs of writing or editing for (other) healthcare professionals. In particular You use jargon when there are suitable plain English words (for example, consider using "kidney" rather than "renal"). and You use a writing style appropriate only for graduate-level courses, because that's what you see in peer-reviewed journal articles and professional reference works.. For this reason, once you've reduced the jargon and tried to make the language less technical, it may be worth getting several non-experts to read through the text and give feedback on accessibility.
- I believe I've addressed this in pharmacodynamics. I've gotten feedback from WT:MED on side effects and OD symptoms. My unorthodox link to the less technical version on Adderall was also supported in a discussion on WT:MED. I await your thoughts. Seppi333 (Insert 2¢ | Maintained) 12:31, 27 May 2014 (UTC)
- Once everything else is done, the lead probably needs a careful read through. At the moment there are four notes, and a large number of references. This really should not be necessary if the lead is written well, and if it doesn't cover any material not covered in the main text of the article. I would leave addressing this until you're happy with everything else though.
- I'm seeking consensus on WT:MED at the moment. You're welcome to participate. I do not agree with you on this, but this is up to the community and not me or the FAC review. Seppi333 (Insert 2¢ | Maintained) 12:31, 27 May 2014 (UTC)
- The article is very US-centric. I mentioned this several times during the FAC, giving a few examples. However it's a general problem that is prevalent throughout the article.
- I'm seeking consensus on WT:MED at the moment. You're welcome to participate. I don't believe that it is US centric, but I'm not entirely sure that I know what your concern is either. I've asked WT:MED to take a look and make a determination on this. Hence, the removal of any language regarding the US will be up to the consensus developed there. Seppi333 (Insert 2¢ | Maintained) 12:31, 27 May 2014 (UTC)
- Some concerns at the previous FAC, and the talk page archives have not been addressed and kept popping up. For example a number of Aa77zz's concerns are still present, and maybe some in the talk-page archives as well (lead verbosity for example). I suppose my point is that if people keep raising very similar concerns, there is probably something in it, even if you disagree, and may be worth the effort to make extra sure that it's been addressed adequately.
- AA77zz's concerns about the lead are now entirely moot. I'm seeking a consensus, rendering his personal preference unimportant, unless he wishes to participate in the discussion. Seppi333 (Insert 2¢ | Maintained) 12:31, 27 May 2014 (UTC)
- I'll leave you to use this feedback. If you try and address these comments, and think the article is ready for FA, I'd then open a peer review and ask for further feedback. Having a peer review is better than using the talk page because it keeps everything together and can easily be referred to in the future (like past FACs, GA reviews etc) rather than an annoying search back through talk page archives. I'm not sure exactly how to take your last comment, but an incomplete review at FAC should not run to > 100 kB. That's probably a sign that the article was far from ready before being nominated. There is still a lot to do before the article is ready, and it's not just a case of giving it a little bit of a polish. Because of this, I'm going to give you at least a few weeks before coming back, but if you're convinced it's ready before then do let me know. I hope all this helps, and also hope you remember that there is no deadline here, better to take the time getting it right rather than rushing back to FAC, which could just lead to frustration (for everyone). -- Shudde talk 07:30, 25 April 2014 (UTC)
- Alright, I'll work on that. Thank you for explaining that - I didn't understand the "big picture" that you had in mind during the FAC review - this helps me a lot more than a sentence-by-sentence review. Seppi333 (Insert 2¢ | Maintained) 13:51, 26 April 2014 (UTC)
- @Shudde:How should I approach accessibility in sections that are inherently technical, like pharmacology, synthesis, and detection in bodily fluids? Seppi333 (Insert 2¢ | Maintained) 14:08, 26 April 2014 (UTC)
- One suggestion I have for the pharmacodynamics section is to start out with a less technical overview focusing initially on what amphetamine does rather how it does it. For example, the current third paragraph could begin the section. I think this paragraph would provide a more accessible introduction to the section. Boghog (talk) 17:05, 26 April 2014 (UTC)
- Good idea - I'll tinker with that section sometime today or tomorrow.
Thanks for your help with reducing overlinking! Seppi333 (Insert 2¢ | Maintained) 19:58, 26 April 2014 (UTC)
- Good idea - I'll tinker with that section sometime today or tomorrow.
- I'm not sure there is an easy way to reduce jargon and increase accessibility. I wish there was some kind of step-by-step guide out there, but I've not seen one. The only advice I can give is have a look at User:Tony1/Writing exercise box and see if there is anything in there that may be of use. I'm not sure what else I can suggest, other than maybe trying to recruit some non-experts to help with the copy-edit, but that may be difficult. -- Shudde talk 00:24, 27 April 2014 (UTC)
- One suggestion I have for the pharmacodynamics section is to start out with a less technical overview focusing initially on what amphetamine does rather how it does it. For example, the current third paragraph could begin the section. I think this paragraph would provide a more accessible introduction to the section. Boghog (talk) 17:05, 26 April 2014 (UTC)
- There are plenty of comments at the recent FAC that probably need to be fully addressed. My comments there should be taken as guidance and examples of what further work is required, rather than a point by point list of problems. I'm not going to repeat all those here as it's not necessary. I'll repeat a couple of my concerns though, and will wait until these have been adequately addressed before giving the article another read through.
@All: I've been procrastinating - I'll make the edits to pharmacology before Friday and repost here once I'm done simplifying what I can.
- Medical uses - Summary of Millichap's review
@Shudde: I'm still sort of unsure about what your concerns were with the long-term evidence review, so I was wondering if you would be willing to read the cited section excerpt and give me your thoughts on how you'd phrase it:
Quoted from pages 122-123 of the Millichap text (Link inside tab).
|
|---|
|
The author stated that the underlined study was both multicenter and placebo controlled, which makes it higher quality evidence than the other open placebo-controlled studies.
I uploaded this newer review which indicated more or less the same continuation of benefits from 2 studies involving ~2 years of amphetamine use (Scroll down to table 2 or search for the term "amfetamine" to get there - the paper uses the amphetamine INN); these were open, placebo-controlled trials though. Millichap also pointed out the unusually exceptional benefits beyond just a continued therapeutic effect that were observed in that multicenter trial as well.
- A note about the studies: I don't know if this is obvious or not, but it's not really possible to "blind" the patients in a study involving amphetamine, so none of the referenced studies are double-blinded. Amphetamine has a rapid onset with an extremely noticeable psychoactive effect even in long-term daily users of the drug. Receiving the drug vs placebo is probably about as obvious as taking very high-dose niacin vs a placebo in niacin megadose-naive individuals (i.e., the presence/absence of the massive full-body niacin-flush would be telling).
Any thoughts/advice/suggestions on communicating this material? Seppi333 (Insert 2¢ | Maintained) 08:43, 30 April 2014 (UTC)
- Pharmacodynamics
I followed Boghog's advice and put the simpler and more general pharmacodynamic information first. It currently summarizes the effect it has on catecholamines and the neural pathways in acts upon in the first paragraph. I don't think I can simplify the subsequent material more than using the graphic I made to illustrate the process though. It simply requires a technical background to understand.
In any event, I'm satisfied with this section now. If you could take a look at it and give me your thoughts, I'd appreciate it. Seppi333 (Insert 2¢ | Maintained) 03:19, 4 May 2014 (UTC)
- Wikilinks
Per AWB, there's now at most 2 wikilinks for any given term in the article. Seppi333 (Insert 2¢ | Maintained) 03:39, 4 May 2014 (UTC)
Discussion
@Shudde: Can you give me some feedback on the recent changes please? Seppi333 (Insert 2¢ | Maintained) 03:45, 4 May 2014 (UTC)
- I'll have a brief look, but I've got a few other projects on the go at the moment, so can't promise too much time during the next two weeks. Sorry I forgot to answer the Millichap comment, but my problem was never with the use of them as a source, rather (as per my FAC comments) how the material was presented. There is a more detailed critique at the FAC. -- Shudde talk 04:05, 4 May 2014 (UTC)
- Is there any specific area where you want feedback? Like I said I can't devote much time, so if you have a particular area you want me to look at then that would be good. -- Shudde talk 04:09, 4 May 2014 (UTC)
- Just two things: help with phrasing the Millichap cited prose and your thoughts on the general layout of pharmacodynamics in terms of accessibility. Seppi333 (Insert 2¢ | Maintained) 04:18, 4 May 2014 (UTC)
- Regarding the layout of that section, I'm not sure it makes life much easier regarding accessibility. Even the first sentence, indeed the first paragraph, reads much more like a technical review than an encyclopaedia article. Regarding the Millichap paragraph, it's very dry, which is one of the problems. It again reads as technical, is it important the children were Swedish? Do we need to know it was a 4.5 increase in IQ (rather than just an increase, or small increase, or moderate increase? Are these details important to non-technical readers? Technical readers should have access to the review and the primary literature, so if they want these details they are available; we shouldn't be including a lot of info on the methodology unless we absolutely have to. This is part of the problem with the article, it gives excessive technical detail, which hinders readability, does not increase accessibility, and seems unlikely to appeal to many non-lay readers. Try and cut that where you can, and if you really, really want to keep some of it, then retain it as a note rather than in the main body of text. That way someone that wants the technical details without accessing the sources (I would hope these would not be professionals or researchers) can do so, but it doesn't weigh down the text, or make the prose suffer. -- Shudde talk 04:46, 4 May 2014 (UTC)
- I'll see what I can do what I can about the detail. I didn't make any changes to the Millichap sentence - I linked it above because I wanted your take on how to phrase it. I'm not entirely sure what your concern is so I don't think I can fix the problem myself. I was hoping you could take a look at it and give me your version. Seppi333 (Insert 2¢ | Maintained) 04:56, 4 May 2014 (UTC)
- Regarding the layout of that section, I'm not sure it makes life much easier regarding accessibility. Even the first sentence, indeed the first paragraph, reads much more like a technical review than an encyclopaedia article. Regarding the Millichap paragraph, it's very dry, which is one of the problems. It again reads as technical, is it important the children were Swedish? Do we need to know it was a 4.5 increase in IQ (rather than just an increase, or small increase, or moderate increase? Are these details important to non-technical readers? Technical readers should have access to the review and the primary literature, so if they want these details they are available; we shouldn't be including a lot of info on the methodology unless we absolutely have to. This is part of the problem with the article, it gives excessive technical detail, which hinders readability, does not increase accessibility, and seems unlikely to appeal to many non-lay readers. Try and cut that where you can, and if you really, really want to keep some of it, then retain it as a note rather than in the main body of text. That way someone that wants the technical details without accessing the sources (I would hope these would not be professionals or researchers) can do so, but it doesn't weigh down the text, or make the prose suffer. -- Shudde talk 04:46, 4 May 2014 (UTC)
- Just two things: help with phrasing the Millichap cited prose and your thoughts on the general layout of pharmacodynamics in terms of accessibility. Seppi333 (Insert 2¢ | Maintained) 04:18, 4 May 2014 (UTC)
- There are a number of problems in addition to those listed above, but really I wonder why it couldn't be simplified -- The safety and effectiveness of long-term amphetamine use in treating ADHD is well established. A nine month randomized controlled trial of amphetamine treatment for ADHD in children found that the children experienced improvements in attention, disruptive behaviors, and hyperactivity, and also found a small [or whatever, moderate?] increase in IQ. Of course, another problem with this paragraph (regardless of the prose) is that you've only used one review, and one nine month trial when elaborating on long-term safety and efficacy. It does come across as a bit flimsy, but if you're going to give examples supporting a statement (even though you don't need to have further evidence if they statement is well supported by RS) then this does seem like a strange one. Of course, for the lay reader you've helped a little because you've said what long-term means in this case (nine months). As well, all the terms used "attention, disruptive behaviors, and hyperactivity, and a small increase in IQ" would not be unfamiliar to an English speaking adult, so you don't have to stress about jargon. This is just a suggestion, but hopefully illustrates the kind of thing I've been thinking. -- Shudde talk 09:22, 5 May 2014 (UTC)
- Before
Reviews of clinical stimulant research have established the safety and effectiveness of long-term amphetamine use for ADHD.[1][2] An evidence review noted the findings of a randomized controlled trial of amphetamine treatment for ADHD in Swedish children following 9 months of amphetamine use.[3] During treatment, the children experienced improvements in attention, disruptive behaviors, and hyperactivity, and an average change of +4.5 in IQ.[3] It noted that the population in the study had a high rate of comorbid disorders associated with ADHD and suggested that other long-term amphetamine trials in people with less associated disorders could find greater functional improvements.[3]
- After
Reviews of clinical stimulant research have established the safety and effectiveness of long-term amphetamine use for ADHD.[1][4] Controlled trials spanning two years have demonstrated continuous treatment effectiveness and safety.[4][3] One review highlighted a 9 month randomized controlled trial in children that found an average increase of 4.5 in the IQ and continued improvements in attention, disruptive behaviors, and hyperactivity.[3]
References
- ^ a b A ref named "Millichap_3" (cited elsewhere)
- ^ Chavez B, Sopko MA, Ehret MJ, Paulino RE, Goldberg KR, Angstadt K, Bogart GT (June 2009). "An update on central nervous system stimulant formulations in children and adolescents with attention-deficit/hyperactivity disorder". Ann. Pharmacother. 43 (6): 1084–1095. doi:10.1345/aph.1L523. PMID 19470858.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b c d e Millichap JG (2010). Millichap JG (ed.). Attention Deficit Hyperactivity Disorder Handbook: A Physician's Guide to ADHD (2nd ed.). New York: Springer. pp. 122–123. ISBN 9781441913968. Cite error: The named reference "Millichap" was defined multiple times with different content (see the help page).
- ^ a b Huang YS, Tsai MH (2011). "Long-term outcomes with medications for attention-deficit hyperactivity disorder: current status of knowledge". CNS Drugs. 25 (7): 539–554. doi:10.2165/11589380-000000000-00000. PMID 21699268.
{{cite journal}}: Unknown parameter|month=ignored (help)
The main changes were the removal and addition of a review, summary of both reviews, and merging two sentences. Minor copyedits too. How's it look now? Seppi333 (Insert 2¢ | Maintained) 10:44, 5 May 2014 (UTC)
- The last sentence seems like a violation of WP:CRYSTAL (it may be better, but we don't know, so why mention it?) and you've still left details such as "+4.5 in IQ" (I mentioned this earlier). How have the reviews established anything? The research established it and I the experts have reached a consensus (I assume -- if not, lets make that clear). It's definitely better, but we still have things like "inconsequential adverse effects" when we could just say "safe". The addition of a two year trial does help though -- especially as this further helps define what is meant by long-term. But like I said, big improvement over what was there originally. -- Shudde talk 11:13, 5 May 2014 (UTC)
Eh, 4.5 points is roughly 5% of the average person's IQ. Seems sizeable to me, but I'll cut it if it's that much of an issue for you. I've made changes per your suggestion - the new section is reflected in the blockquote above. A minor detail, though the reviews cover 4 trials with durations of 9, 15, 24, and 24 months. Seppi333 (Insert 2¢ | Maintained) 12:49, 5 May 2014 (UTC)
- @Shudde: Hey Shudde, how do you feel about what I've done with Amphetamine#Pharmacodynamics and Adderall#Mechanism of action to address accessibility? (See the hatnotes)Seppi333 (Insert 2¢ | Maintained) 03:22, 25 May 2014 (UTC)
- I have seen the discussion at WT:MED -- and after reading your comments there, I've decided not to give further feedback -- it's just not worth my time. I've stated my objections to giving this article the star, and I'll leave it to you and others to try and address those. The article still lacks accessibility and has a number of other weaknesses (see the many hundreds (thousands?) or words I've written on this article). At the moment it's just not written for the general reader. It fails criteria 1a "its prose is engaging, even brilliant, and of a professional standard" -- there is no way the prose is engaging, and it's definitely not brilliant. And of course there is the WP:MOSMED problems I've stated before, (see the section Signs of writing or editing for (other) healthcare professionals). I've got limited time to edit at the moment, and I get the feeling you see producing an FA as jumping through a number of hoops, addressing a few comments, brow-beating over others, then eventually getting a nice star. I see it as producing an article of a certain quality (whether called "FA" or not). Because of this difference of view, and my limited time, I'd rather focus on WP:PR and other editing than comment further here. I hope you can find someone to help with the accessibility problem. -- Shudde talk 09:47, 28 May 2014 (UTC)
- Fair enough. I consider a lot of the replacement text you provided me with to be poorly written, but I simply added that to placate you. I agree with you on some issues, but "brilliant" text is subjective, and I doubt you can show me a single article I'd agree with you about that on. Glad you're finished reviewing. Seppi333 (Insert 2¢ | Maintained) 14:51, 28 May 2014 (UTC)
Adding a table of affinities
I believe that a good addition to this article would be adding a table that that includes Amphetamine's EC50, IC50, and dissociation constant (Ki) values. I think this table should include binding to the monoamine transporters (including VMAT), and receptor affinities (since amphetamine does have very minor, but notable) at some of the adrenergic receptors and dopamine receptors. Personally, I think that would pretty much complete this article.
What does everyone else think?
SwampFox556 (talk) 02:29, 27 April 2014 (UTC)
- Double check the species in the database you're looking at. If it's not homo sapiens sapiens/homo sapiens, it's not relevant data for us. Wouldn't satisfy WP:MEDRS (WP:MEDANIMAL) anyway. I'm not aware of any postsynaptic receptor targets for amph in humans (I know of 5-ht and adrenergic receptor affinities in certain rodent species; IDK what species has DA affinities though). That said, if you've got a database or literature ref for human receptors, please let me know!
 Seppi333 (Insert 2¢ | Maintained) 08:49, 27 April 2014 (UTC)
Seppi333 (Insert 2¢ | Maintained) 08:49, 27 April 2014 (UTC)
- Absolutely. I'll look right now in fact. If you also want to look (and if I remember correctly) it's DA affinity was something like 200ish Ki for D1 and 770ish Ki for D5. It's adrenergic affinity was something that surprised me (and that's why I remember), it had a Ki of 76 for Alpha-1 receptors, no affinity for alpha-2, and slight... I think it was...Beta-2? Anyways, the Ki was listed as 1000+.
Anyways, I'll check through my plethora of bookmarked studies and go from there ;). Good hunting!
SwampFox556 (talk) 01:09, 29 April 2014 (UTC)
Small nomenclature error in synthetic route 5
@Boghog: The imine intermediate in method 5 is incorrectly named (2-nitroprop-1-en-1-yl)benzene. I'm guessing that was accidentally carried over from method 4?
Since it's a primary imine, I'm pretty sure you'd just call it 1-phenylpropan-2-imine. BlackstarX (talk) 07:35, 1 May 2014 (UTC)
 Fixed. Thanks for catching the error. It now should be correct. Cheers. Boghog (talk) 13:46, 1 May 2014 (UTC)
Fixed. Thanks for catching the error. It now should be correct. Cheers. Boghog (talk) 13:46, 1 May 2014 (UTC)
Cite error: There are <ref group=note> tags on this page, but the references will not show without a {{reflist|group=note}} template (see the help page).