Sickness behavior
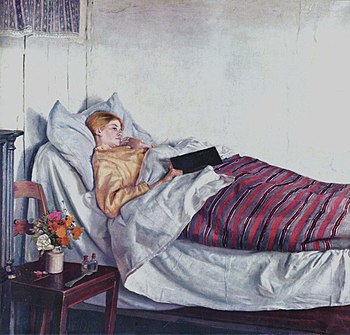
Sickness behavior is a coordinated set of adaptive behavioral changes that develop in ill individuals during the course of an infection.[1] They usually, but not always,[2] accompany fever and aid survival. Such illness responses include lethargy, depression, anxiety, malaise, loss of appetite,[3][4] sleepiness,[5] hyperalgesia,[6] reduction in grooming[1][7] and failure to concentrate.[8] Sickness behavior is a motivational state that reorganizes the organism's priorities to cope with infectious pathogens.[8][9] It has been suggested as relevant to understanding depression,[10] and some aspects of the suffering that occurs in cancer.
History
[edit]Sick animals have long been recognized by farmers as having different behavior. Initially it was thought that this was due to physical weakness that resulted from diverting energy to the body processes needed to fight infection. However, in the 1960s, it was shown that animals produced a blood-carried factor X that acted upon the brain to cause sickness behavior.[11][12] In 1987, Benjamin L. Hart brought together a variety of research findings that argued for them being survival adaptations that if prevented would disadvantage an animal's ability to fight infection. In the 1980s, the blood-borne factor was shown to be proinflammatory cytokines produced by activated leukocytes in the immune system in response to lipopolysaccharides (a cell wall component of Gram-negative bacteria). These cytokines acted by various humoral and nerve routes upon the hypothalamus and other areas of the brain. Further research showed that the brain can also learn to control the various components of sickness behavior independently of immune activation.[citation needed].
In 2015, Shakhar and Shakhar[13] suggested instead that sickness behavior developed primarily because it protected the kin of infected animals from transmissible diseases. According to this theory, termed the Eyam hypothesis, after the English Parish of Eyam, sickness behavior protects the social group of infected individuals by limiting their direct contacts, preventing them from contaminating the environment, and broadcasting their health status. Kin selection would help promote such behaviors through evolution. In a highly prosocial species like humans, however, sickness behavior may act as a signal to motivate others to help and care for the sick individual.[14]
Advantages
[edit]General advantage
[edit]Sickness behavior in its different aspects causes an animal to limit its movement; the metabolic energy not expended in activity is diverted to the fever responses, which involves raising body temperature.[1] This also limits an animal's exposure to predators while it is cognitively and physically impaired.[1]
Specific advantages
[edit]The individual components of sickness behavior have specific individual advantages. Anorexia limits food ingestion and therefore reduces the availability of iron in the gut (and from gut absorption). Iron may aid bacterial reproduction, so its reduction is useful during sickness.[15] Plasma concentrations of iron are lowered for this anti-bacterial reason in fever.[16] Lowered threshold for pain ensures that an animal is attentive that it does not place pressure on injured and inflamed tissues that might disrupt their healing.[1] Reduced grooming is adaptive since it reduces water loss.[1]
Inclusive fitness advantages
[edit]According to the 'Eyam hypothesis',[13] sickness behavior, by promoting immobility and social disinterest, limits the direct contacts of individuals with their relatives. By reducing eating and drinking, it limits diarrhea and defecation, reducing environmental contamination. By reducing self-grooming and changing stance, gait and vocalization, it also signals poor health to kin. All in all, sickness behavior reduces the rate of further infection, a trait that is likely propagated by kin selection.[citation needed]
Social advantage
[edit]Humans helped each other in case of sickness or injury throughout their hunter-gatherer past and afterwards. Convincing others of being badly in need of relief, assistance, and care heightened the chance of survival of the sick individual. High direct costs, such as energy spent on fever and potential harm caused by high body temperatures, and high opportunity costs, as caused by inactivity, social disinterest, and lack of appetite, make sickness behavior a highly costly and therefore credible signal of need.[14]
Immune control
[edit]Lipopolysaccharides trigger the immune system to produce proinflammatory cytokines IL-1, IL-6, and tumor necrosis factor (TNF).[17] These peripherally released cytokines act on the brain via a fast transmission pathway involving primary input through the vagus nerves,[18][19] and a slow transmission pathway involving cytokines originating from the choroid plexus and circumventricular organs and diffusing into the brain parenchyma by volume transmission.[20] Peripheral cytokines are capable of entering the brain directly[21][22] but are large lipophilic polypeptide proteins that generally do not easily passively diffuse across the blood-brain barrier. They may also induce the expression of other cytokines in the brain that cause sickness behavior.[23][24] Acute psychosocial stress enhances the ability of an immune response to trigger both inflammation and behavioral sickness.[25]
Behavioral conditioning
[edit]The components of sickness behavior can be learned by conditional association. For example, if a saccharin solution is given with a chemical that triggers a particular aspect of sickness behavior, on later occasions the saccharin solution will trigger it by itself.[26][27]
Medical conditions
[edit]Depression
[edit]It has been proposed that major depressive disorder is nearly identical with sickness behavior, raising the possibility that it is a maladaptive manifestation of sickness behavior due to abnormalities in circulating cytokines.[28][29][30] Moreover, chronic, but not acute, treatment with antidepressant drugs was found to attenuate sickness behavior symptoms in rodents.[31] The mood effects caused by interleukin-6 following an immune response have been linked to increased activity within the subgenual anterior cingulate cortex,[32] an area involved in the etiology of depression.[33] Inflammation-associated mood change can also produce a reduction in the functional connectivity of this part of the brain to the amygdala, medial prefrontal cortex, nucleus accumbens, and superior temporal sulcus.[32]
Cancer side effect
[edit]In cancer, both the disease and the chemotherapy treatment can cause proinflammatory cytokine release which can cause sickness behavior as a side effect.[34][35]
See also
[edit]References
[edit]- ^ a b c d e f Hart, BL (1988). "Biological basis of the behavior of sick animals". Neuroscience and Biobehavioral Reviews. 12 (2): 123–137. doi:10.1016/S0149-7634(88)80004-6. PMID 3050629. S2CID 17797005.
- ^ Kent, S.; Bluthe, R. M.; Dantzer, R.; Hardwick, A. J.; Kelley, K. W.; Rothwell, N. J.; Vannice, J. L. (1992). "Different receptor mechanisms mediate the pyrogenic and behavioral effects of interleukin 1". Proceedings of the National Academy of Sciences of the United States of America. 89 (19): 9117–9120. Bibcode:1992PNAS...89.9117K. doi:10.1073/pnas.89.19.9117. PMC 50076. PMID 1409612.
- ^ Exton, M. S. (1997). "Infection-Induced Anorexia: Active Host Defence Strategy". Appetite. 29 (3): 369–383. doi:10.1006/appe.1997.0116. PMID 9468766. S2CID 10465902.
- ^ Murray, M. J.; Murray, A. B. (1979). "Anorexia of infection as a mechanism of host defense". The American Journal of Clinical Nutrition. 32 (3): 593–596. doi:10.1093/ajcn/32.3.593. PMID 283688.
- ^ Mullington, J.; Korth, C.; Hermann, D. M.; Orth, A.; Galanos, C.; Holsboer, F.; Pollmächer, T. (2000). "Dose-dependent effects of endotoxin on human sleep". American Journal of Physiology. Regulatory, Integrative and Comparative Physiology. 278 (4): R947–R955. doi:10.1152/ajpregu.2000.278.4.r947. PMID 10749783. S2CID 10272455.
- ^ Maier, SF; Wiertelak, EP; Martin, D; Watkins, LR (1993). "Interleukin-1 mediates the behavioral hyperalgesia produced by lithium chloride and endotoxin". Brain Research. 623 (2): 321–324. doi:10.1016/0006-8993(93)91446-Y. PMID 8221116. S2CID 40529634.
- ^ Dantzer R, Kelley KW (February 2007). "Twenty years of research on cytokine-induced sickness behavior". Brain Behav. Immun. 21 (2): 153–160. doi:10.1016/j.bbi.2006.09.006. PMC 1850954. PMID 17088043.
- ^ a b Kelley, KW; Bluthé, RM; Dantzer, R; Zhou, JH; Shen, WH; Johnson, RW; Broussard, SR (2003). "Cytokine-induced sickness behavior". Brain, Behavior, and Immunity. 17 (Suppl 1): S112–S118. doi:10.1016/S0889-1591(02)00077-6. PMID 12615196. S2CID 25400611.
- ^ Johnson, R. W. (2002). "The concept of sickness behavior: A brief chronological account of four key discoveries". Veterinary Immunology and Immunopathology. 87 (3–4): 443–450. doi:10.1016/S0165-2427(02)00069-7. PMID 12072271.
- ^ Dantzer, Robert (May 2009). "Cytokine, Sickness Behavior, and Depression". Immunology and Allergy Clinics of North America. 29 (2): 247–264. doi:10.1016/j.iac.2009.02.002. PMC 2740752. PMID 19389580. Retrieved 23 February 2015.
- ^ Holmes, J. E.; Miller, N. E. (1963). "Effects of Bacterial Endotoxin on Water Intake, Food Intake, and Body Temperature in the Albino Rat". The Journal of Experimental Medicine. 118 (4): 649–658. doi:10.1084/jem.118.4.649. PMC 2137667. PMID 14067912.
- ^ Miller, N. (1964) "Some psychophysiological studies of motivation and of the behavioral effects of illness". Bull. Br. Psychol. Soc. 17: 1–20
- ^ a b Shakhar K, Shakhar G (Oct 2015). "Why Do We Feel Sick When Infected-Can Altruism Play a Role?". PLOS Biol. 13 (10): e1002276. doi:10.1371/journal.pbio.1002276. PMC 4608734. PMID 26474156.
- ^ a b Steinkopf L (Aug 2015). "The Signaling Theory of Symptoms: An Evolutionary Explanation of the Placebo Effect". Evolutionary Psychology. 13 (3): 100. doi:10.1177/1474704915600559. PMC 10480909. PMID 37924177.
- ^ Kluger, M. J.; Rothenburg, B. A. (1979). "Fever and reduced iron: Their interaction as a host defense response to bacterial infection". Science. 203 (4378): 374–376. Bibcode:1979Sci...203..374K. doi:10.1126/science.760197. PMID 760197.
- ^ Weinberg, E. D. (1984). "Iron withholding: A defense against infection and neoplasia". Physiological Reviews. 64 (1): 65–102. doi:10.1152/physrev.1984.64.1.65. PMID 6420813.
- ^ Konsman, JP; Parnet, P; Dantzer, R (March 2002). "Cytokine-induced sickness behaviour: mechanisms and implications". Trends in Neurosciences. 25 (3): 154–159. doi:10.1016/s0166-2236(00)02088-9. PMID 11852148. S2CID 29779184.
- ^ Goehler, L. E.; Gaykema, R. P.; Nguyen, K. T.; Lee, J. E.; Tilders, F. J.; Maier, S. F.; Watkins, L. R. (1999). "Interleukin-1beta in immune cells of the abdominal vagus nerve: A link between the immune and nervous systems?". The Journal of Neuroscience. 19 (7): 2799–2806. doi:10.1523/JNEUROSCI.19-07-02799.1999. PMC 6786076. PMID 10087091.
- ^ Goehler, L. E.; Relton, J. K.; Dripps, D.; Kiechle, R.; Tartaglia, N.; Maier, S. F.; Watkins, L. R. (1997). "Vagal paraganglia bind biotinylated interleukin-1 receptor antagonist: A possible mechanism for immune-to-brain communication". Brain Research Bulletin. 43 (3): 357–364. doi:10.1016/s0361-9230(97)00020-8. PMID 9227848. S2CID 22591654.
- ^ Konsman, J. P.; Kelley, K.; Dantzer, R. (1999). "Temporal and spatial relationships between lipopolysaccharide-induced expression of Fos, interleukin-1beta and inducible nitric oxide synthase in rat brain". Neuroscience. 89 (2): 535–548. doi:10.1016/s0306-4522(98)00368-6. PMID 10077334. S2CID 25173830.
- ^ Banks, W. A.; Kastin, A. J.; Gutierrez, E. G. (1994). "Penetration of interleukin-6 across the murine blood-brain barrier". Neuroscience Letters. 179 (1–2): 53–56. doi:10.1016/0304-3940(94)90933-4. PMID 7845624. S2CID 22712577.
- ^ Banks, W. A.; Ortiz, L.; Plotkin, S. R.; Kastin, A. J. (1991). "Human interleukin (IL) 1 alpha, murine IL-1 alpha and murine IL-1 beta are transported from blood to brain in the mouse by a shared saturable mechanism". The Journal of Pharmacology and Experimental Therapeutics. 259 (3): 988–996. PMID 1762091.
- ^ Ban, E.; Haour, F.; Lenstra, R. (1992). "Brain interleukin 1 gene expression induced by peripheral lipopolysaccharide administration". Cytokine. 4 (1): 48–54. doi:10.1016/1043-4666(92)90036-Q. PMID 1535519.
- ^ Van Dam, A. M.; Brouns, M.; Louisse, S.; Berkenbosch, F. (1992). "Appearance of interleukin-1 in macrophages and in ramified microglia in the brain of endotoxin-treated rats: A pathway for the induction of non-specific symptoms of sickness?". Brain Research. 588 (2): 291–296. doi:10.1016/0006-8993(92)91588-6. PMID 1393581. S2CID 35583973.
- ^ Brydon, L.; Walker, C.; Wawrzyniak, A.; Whitehead, D.; Okamura, H.; Yajima, J.; Tsuda, A.; Steptoe, A. (2009). "Synergistic effects of psychological and immune stressors on inflammatory cytokine and sickness responses in humans". Brain, Behavior, and Immunity. 23 (2): 217–224. doi:10.1016/j.bbi.2008.09.007. PMC 2637301. PMID 18835437.
- ^ Exton, M. S.; Bull, D. F.; King, M. G. (1995). "Behavioral conditioning of lipopolysaccharide-induced anorexia". Physiology & Behavior. 57 (2): 401–405. doi:10.1016/0031-9384(94)00249-5. PMID 7716224. S2CID 41061406.
- ^ Exton, M. S.; Bull, D. F.; King, M. G.; Husband, A. J. (1995). "Modification of body temperature and sleep state using behavioral conditioning". Physiology & Behavior. 57 (4): 723–729. doi:10.1016/0031-9384(94)00314-9. PMID 7777610. S2CID 927502.
- ^ Yirmiya, R.; Weidenfeld, J.; Pollak, Y.; Morag, M.; Morag, A.; Avitsur, R.; Barak, O.; Reichenberg, A.; Cohen, E.; Shavit, Y.; Ovadia, H. (1999). "Cytokines, "Depression Due to a General Medical Condition," and Antidepressant Drugs". Cytokines, Stress, and Depression. Advances in Experimental Medicine and Biology. Vol. 461. pp. 283–316. doi:10.1007/978-0-585-37970-8_16. ISBN 978-0-306-46135-4. PMID 10442179.
- ^ Dantzer, R.; O'Connor, J. C.; Freund, G. G.; Johnson, R. W.; Kelley, K. W. (2008). "From inflammation to sickness and depression: When the immune system subjugates the brain". Nature Reviews Neuroscience. 9 (1): 46–56. doi:10.1038/nrn2297. PMC 2919277. PMID 18073775.
- ^ Maes, M. (2008). "The cytokine hypothesis of depression: Inflammation, oxidative & nitrosative stress (IO&NS) and leaky gut as new targets for adjunctive treatments in depression". Neuro Endocrinology Letters. 29 (3): 287–291. PMID 18580840.
- ^ Yirmiya, R. (1996). "Endotoxin produces a depressive-like episode in rats". Brain Research. 711 (1–2): 163–174. doi:10.1016/0006-8993(95)01415-2. PMID 8680860. S2CID 46133689.
- ^ a b Harrison NA, Brydon L, Walker C, Gray MA, Steptoe A, Critchley HD (September 2009). "Inflammation causes mood changes through alterations in subgenual cingulate activity and mesolimbic connectivity". Biol Psychiatry. 66 (5): 407–414. doi:10.1016/j.biopsych.2009.03.015. PMC 2885494. PMID 19423079.
- ^ Drevets WC, Savitz J, Trimble M (August 2008). "The subgenual anterior cingulate cortex in mood disorders". CNS Spectr. 13 (8): 663–681. doi:10.1017/s1092852900013754. PMC 2729429. PMID 18704022. PDF:http://mbldownloads.com/0808CNS_BrainRegions.pdf
- ^ Cleeland, C. S.; Bennett, G. J.; Dantzer, R.; Dougherty, P. M.; Dunn, A. J.; Meyers, C. A.; Miller, A. H.; Payne, R.; Reuben, J. M.; Wang, X. S.; Lee, B. N. (2003). "Are the symptoms of cancer and cancer treatment due to a shared biologic mechanism?". Cancer. 97 (11): 2919–2925. doi:10.1002/cncr.11382. PMID 12767108. S2CID 23198802.
- ^ Myers, J. S. (2008). "Proinflammatory Cytokines and Sickness Behavior: Implications for Depression and Cancer-Related Symptoms". Oncology Nursing Forum. 35 (5): 802–807. doi:10.1188/08.ONF.802-807. PMID 18765326.
