Health effects of electronic cigarettes
This article has multiple issues. Please help improve it or discuss these issues on the talk page. (Learn how and when to remove these messages)
|
The health effects of e-cigarettes (e-cigarettes) are generally claimed to be less than those of smoking, but worse than not smoking at all. However, health is a function not only of the inhaled materials, but of how and how often the products are used, over what period, manufacturing/distribution quality control, marketing, the regulatory environment, and the actual user population.[1] Reported risks include exposure to toxic chemicals, increased likelihood of respiratory and cardiovascular diseases, and accelerated cancer development.
The public health community is divided over the use of these devices to reduce/prevent smoking.[2] As of 2017 they were not approved by the US Centers for Disease Control and Prevention (CDC) as a smoking cessation product.[3] In the United Kingdom, a 2021 review by Public Health England (PHE) reported vaping to be around 95% less harmful than smoking.[4]
A 2019 review concluded that the risk of early death was similar to that of smokeless tobacco.[5] In addition, e-cigarette marketing has been attacked for not focusing on smoking cessation.[3]
Vaping carries some level of health risks.[3][6] E-cigarette aerosols can affect drug dependency, as well as psychological, respiratory, cardiovascular, immunologic, and central nervous systems.[7] Studies have reported that e-cigarettes reduce lung function (versus not smoking), reduce cardiac muscle function, and increase inflammation.[8][9]
THC-containing e-cigarettes were deemed responsible for the 2019–20 vaping lung illness outbreak in North America that led to 68 deaths and was linked to vitamin E acetate in the e-liquid.[10] Misuse and accidents increase risks[11] such as nicotine poisoning,[12][13] contact with liquid nicotine,[14] and fires caused by product malfunction.[15]
E-cigarettes
[edit]

An electronic cigarette (e-cigarette), or vape,[note 1][16] is a device that simulates smoking. It consists of an atomizer, a power source such as a battery, and a container such as a cartridge or tank. Instead of smoke, the user inhales vapor.[17] As such, using an e-cigarette is often called "vaping".[18]
The atomizer is a heating element that vaporizes a liquid solution called e-liquid[19] that cools into an aerosol of tiny droplets, vapor and air.[20] The vapor mainly comprises propylene glycol and/or glycerin, usually with nicotine and flavoring. Its exact composition varies, and depends on matters such as user behavior.[note 2] E-cigarettes are activated by taking a puff or pressing a button.[18][21] Some look like traditional cigarettes,[18][22] and most kinds are reusable.[note 3]
Various e-liquids offer different nicotine strengths and flavors.[24][notes 1][26]
Common ingredients are propylene glycol, glycerin, flavorings, and nicotine.[27] Propylene glycol and glycerin typically comprise 95% , with the remaining 5% combining flavorings, nicotine, and other additives.[28][29] Flavorings may contain menthol, sugars, esters, and pyrazines.[29] Flavor components include diacetyl, acetoin, and 2,3-pentanedione (buttery flavor), eucalyptol, camphor and cyclohexanone (minty flavor), cinnamaldehyde (cinnamon flavor), benzaldehyde (cherry or almond flavor), cresol (leathery or medicinal flavor), butyraldehyde (chocolate flavor), and isoamyl acetate (banana flavor), methyl salicylate, pulegone, ethyl salicylate, eugenol, diphenyl ether, and coumarin.[29][30] A 2017 review added 1,3-butanediol, 1,3-propanediol, ethylene and diethylene glycol, safrole, ethyl vanillin, and α-thujone to the list of ingreidents.[31]
Caffeinated e-liquids typically contain considerably less caffeine than dietary products.[32] E-liquids are available with vitamins or cannabis flavors.[33] E-cigarettes (mods) are available that can vaporize herbs, oils, or fruits.[33] Dual-function devices handle both concentrates and e-liquids using multiple cartridges.[33]
More than 90% of e-liquids contain nicotine.[34] Some are unflavored.[35][36] Water replaces propylene glycol in some products.[37] E-liquids may contain THC or other cannabinoids.[38] Some e-liquids contain a little alcohol.[39][40]
E-liquids are not required to use only US Pharmacopeia grade nicotine, a tobacco plant, or tobacco dust extract, or a synthetic nicotine.[41] Nicotine levels vary.[42] A user survey reported that 97% of respondents used nicotine e-liquids.[43][44]
A 2016 study reported that measurable amounts of arsenic, nickel and other metals were present in some e-liquids.[45] Over 80 chemicals, including formaldehyde and metallic nanoparticles were reported in e-liquids (2019).[46] E-liquid can contain toxicants and impurities.[47] A 2013 study reported as high as five times the permitted levels of impurities.[47] E-liquids contained low levels of some of tobacco smoke toxicants and small concentrations of carcinogens.[48]
In 2009, FDA reported tobacco-specific nitrosamines (TSNAs), diethylene glycol, cotinine, anabasine, myosmine, and beta-nicotyrine in e-liquids.[49] TSNAs N-nitrosonornicotine (NNN), 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK), N-nitrosoanabasine, and nitrosoanatabine were detected in five e-liquid samples from two companies at levels comparable to other nicotine replacement products.[49][50] TSNAs present in tobacco smoke were reported in trace amounts.[51] A 2013 review of other e-liquids did not detect diethylene glycol.[48] The majority of the e-liquids analyzed contained NNN from 0.34 to 60.08 μg/L and NNK from 0.22 to 9.84 μg/L.[52] The FDA warned several e-cigarette companies for selling e-cartridges and refill solutions containing active pharmaceutical ingredients such as rimonabant (Zimulti) for weight loss purposes and reducing smoking, and tadalafil (for erictile dysfunction).[53] FDA analyses reported the presence of am,ino-tadalafil rather than tadalafil, and rimonabant and one of its oxidative products.[53]
E-liquids often contain unknown and/or undisclosed substances.[54]
Poor quality control may allow nicotine and TSNAs to be present in e-liquids labelled 'no nicotine'.[55][48][56] Some e-liquid were reported to contain low levels of anthracene, phenanthrene, 1-methyl phenanthrene and pyren.[57] A 2015 study reported hydrocarbons, terpenic compounds and aldehydes, particularly formaldehyde and acrolein in some e-liquids.[58]
A 2014 study reported that e-liquids from a specific manufacturer contained greater amounts of ethylene glycol than glycerin or propylene glycol, possibly the result of improper manufacturing methods.[56] A 2015 study reported finding solvents such as 1,3-butadiene, cyclohexane, and acetone in e-liquids.[58] A 2016 study reported that some e-liquids contained tobacco alkaloids such as nornicotine, anabasine, anatabine, and TSNAs, such as N-nitrosonornicotine (NNN), 4-(methylnitrosamine)-1-(3-pyridyl)-1-butanone (NNK),[26] nitrates, and phenol.[56] A 2014 study reported small quantities of volatile organic compounds (VOCs) such as benzene, toluene, xylene, and styrene.[59] Diethyl phthalate and diethylhexyl phthalate have been found in e-liquids.[60] Some e-liquids contain tin "whiskers," microscopic crystals that originate from tin in solder joints.[26]Risk context
[edit]When evaluating the health effects of some activity, a reasonable question is "what is the practical alternative?" If the answer is smoking, the answer might be different than if the answer is simply avoiding nicotine. This is because the health impacts of smoking are strongly negative, while the impact of avoiding nicotine without any support is unreservedly positive.
In June 2014, the UK Royal College of Physicians stated, "e-cigarettes could lead to significant falls in the prevalence of smoking in the UK, prevent many deaths and episodes of serious illness, and help to reduce the social inequalities in health that tobacco smoking currently exacerbates."[61] A 2017 National Institute for Health and Care Excellence (NICE) guideline did not recommend e-cigarettes due to concerns regarding safety, efficacy, and product quality.[62]
The American Cancer Society stated, "The makers of e-cigarettes say that the ingredients are 'safe,' but this only means the ingredients have been reported to be safe to eat. Inhaling a substance is not the same as swallowing it. There are questions about how safe it is to inhale some substances in the e-cigarette vapor into the lungs."[63]
Smoking
[edit]E-cigarette vapor does not contain tobacco and does not involve combustion, therefore users do not encounter several unquestionably harmful constituents of tobacco smoke,[11] such as ash, tar, and carbon monoxide.[64] A 2014 review concluded that e-cigarette aerosol contains far fewer carcinogens than tobacco smoke, and concluded that e-cigarettes "impart a lower potential disease burden" than traditional cigarettes.[65]
Smokers can use e-cigarettes for various purposes. As an aid to quitting smoking, vaping is a temporary activity that reduces smoking and terminates once the smoker has completed the transition away from nicotine. Alternatively, smokers can substitute or complement smoking with vaping without intending to transition, meaning that any negative effects are not temporary. In the latter context, the relative risks of vaping vs smoking are of great importance.[66] Furthermore, allowing vaping in public places may undermine smoking regulations.[66] Other smoker-transition aids are available and may offer better safety and/or effectiveness profiles then vaping. Given equal effectiveness, relatively safety considerations would become paramount. [65][67]
Abstinence
[edit]
Vaping presents safety risks that are definitionally higher than those of simple abstinence, as they have no independent health benefits. This comparison is relevant because some users adopt e-cigarettes for the nicotine (or cannabinoids), even though they have never smoked. Once nicotine dependence is established, users may be more likely to take up smoking.
Individual effects
[edit]Health effects for non-smokers must be considered in absolute terms for long-term use as well as the risk of transition into traditiion cigarettes, while for smokers the relative risks are paramount, and if used as a quitting aid, any effects of short-term use are most important.
Non-smokers
[edit]E-cigarettes create nicotine dependence in non-smokers.[68][1] E-cigarettes may act as a gateway drug.[69] This is particularly significant among youth who have no experience with addictive drugs.[70][71] A 2016 review concluded that nicotine exposure harms youths' growing brains.[72] Pregnant or nursing women and the elderly are more sensitive to nicotine than other individuals.[73]
Smokers
[edit]Used as a transition to abstinence, e-cigarettes end the consumption of nicotine and the other harmful substances in tobacco smoke and later any harmful e-liquid ingredient. However, if transition is unsuccessful, e-cigarettes could mean increased nicotine dependence (by combining smoking and vaping) and ongoing harm from other e-liquid ingredients.[74][75][76]
Health benefits associated with transitioning from smoking to vaping include decreased post-smoking weight gain and improved exercise tolerance.[77]
Even a partially successful transition may allow smokers to reduce their cigarette consumption and related health effects.[78] A 2022 Cochrane review concluded that vaping increased quit rates compared to e-cigarettes without nicotine and compared to nicotine replacement therapy, although it did not compare vaping to other methods.[79][needs update]
A 2018 review concluded that child vapers had a higher likelihood of more and more significant adverse effects than child smokers. Significant harmful effects included cyanosis, nausea, and coma.[80]
The relative safety of electronic versus conventional cigarettes is disputed. 2015[81] : 76 and 2018 Public Health England (PHE) reports claimed that vaping is "at least 95% less harmful than smoking".[81]: 175 The Royal College of Physicians, the Royal Society for Public Health, and the National Health Service backed these claims.[82] The estimate was limited by "lack of hard evidence for the harms of most products on most of the criteria".[82] The research was funded by EuroSwiss Health and was criticized for its weak methodology,[83] lack of specific evidence,[82] and for financial ties to the tobacco industry.[83][82] The estimate was disputed in medical journals.[84][85] Reviews in 2016 and 2018 claimed that the harm from e-cigarettes is much higher than the "95% safer" figure.[86][82]
A 2025 RCP review[87] reported that e-cigarettes sold in England (which allow nicotine strength[88] of no more than 20 mg/ml[89]) are unlikely to exceed 5% of the harm of cigarettes for non-pregnant adults. This claim is consistent with the 2018 view of the US National Academies of Sciences, Engineering, and Medicine.[90] A 2013 review did not claim that vaping reduced nicotine consumption vs smoking.[91]
General risks
[edit]Battery explosions can be caused by thermal runaway and may cause burns or other injuries.[92]
Nicotine poisoning can occur by ingestion, inhalation, or absorption via the skin or eyes.[13][93][94]
E-liquid exposure can come by leaks or spills.[95]
A 2018 review concluded that exposure to vapor can reduce lung function.[96]
Adverse effects are mostly associated with short-term use and the reported adverse effects decreased over time.[97]
Airways
[edit]Potential adverse effects include airway resistance, irritation of the airways, eyes redness, dry throat,[98] and increase in allergic airway inflammation with elevated infiltration of inflammatory cells including eosinophils into airways. [74] A 2015 study reported that short-term adverse effects reported most often were mouth and throat irritation, dry cough, and nausea.[97] Dryness of the mouth and throat is believed to stem from water absorption by propylene glycol and glycerin.[99] : Humectants (Delivery Solvents), 157
Throat irritation could be the result of exposure to nicotine, nicotine solvents, or toxicants in the aerosol.[13]
A 2016 study reported nose bleeds, change in bronchial gene expression, release of cytokines and proinflammatory mediators.[74]
Neurological
[edit]A 2013 report to the FDA identified minor headache, chest pain, nausea, and cough as side effects. Major adverse events included hospitalizations for pneumonia, congestive heart failure, seizure, rapid heart rate, and burns. However, no causal relationship to vaping was proven.[92] Many effects on the nervous and the sensory systems are possibly related to nicotine overdose or withdrawal.[100]
A 2016 study reported that an e-liquid containing 23% alcohol was linked to reduced performance on the Purdue Pegboard Test.[101]
A 2017 study reported harm to neurons and tremors and spasms.[102]
Injuries
[edit]
E-cigarettes typically use lithium batteries, which may fail if defective[104] or misused.[11] A 2015 PHE report concluded that fire risks from e-cigarettes "appear to be comparable to similar electrical goods".[81]: 83–84 In 2018 PHE reported six UK case studies involving e-cigarettes with burns.[81]: 144 E-liquid ingredients may be flammable.[105] A 2014 review claimed that some users add more or larger batteries to nonadjustable e-cigarettes, which may lead to battery leakage or explosion.[105][106]
A 2016 study reported that the explosion risk was low.[107] Another 2016 study assembled reports of 92 explosion, fire, or overheating events, with related injuries in 47 individuals.[108] Prominent harms included 2 cervical vertebral fractures, 1 palate fracture, 3 instances of damaged teeth, 33 thermal burns, 4 chemical burns, and 5 lacerations.[108] A 2017 study reported that most e-cigarette fires are triggered by batteries overheating and igniting.[99]: Summary, Conclusion 14-1., 9 [109]
An e-cigarette explosion or fire can induce serious burns and harms that need medical treatment.[81]: 149 Explosions have resulted in lost teeth, neck fractures, and burns from combustion and/or battery acid.[107][110] Reported burns covered from 1% to 8% of body area. They were most commonly reported in the lower extremity, hands, head and neck, and genitalia.[111] Explosions in some cases produced 2nd and 3rd degree burns.[112] A review concluded that some 50% needed surgical management.[111] The most common harms are burns as a result of explosion while carrying an e-cigarette.[113]
A 2017 review concluded, "Several of the reported cases show that 'the battery in pocket' precedes the incident. The damp environment in the pocket may have sufficient moisture to start a chemical reaction within the lithium-ion battery and the presence of metal objects can produce short-circuit which can over heat the battery leading to an explosion."[114] Burn risk extends to bystanders.[107] Property may also be damaged.[107]

The United States Fire Administration reported 195 occasions of e-cigarette fires and explosions between January 2009 and December 2016. These incidents resulted in 133 acute injuries, of which 38 (29 percent) were severe.[103] A 2017 review concluded that 80% of e-cigarette explosions occurred during battery charging, many by 3rd-party power adaptors that used inappropriately high charge rates that led to thermal runaway. Some third-party vendors assemble e-cigarettes from incompatible parts that do not meet manufacturers' specifications. Batteries are typically cylindrical, with the least strongest structural points at the ends.[108] Given a battery seal breach, the ends may accelerate away.[108]

Burn events while on home oxygen therapy have been reported, leading Health Canada in 2014 to warn of fire risk. The heating element in vaping devices can get hot enough to ignite in the presence of oxygen.[117]
Poisoning
[edit]
E-cigaratte nicotine poisoning occurs via ingestion, inhalation, or absorption via the skin or eyes.[13][12]
Such poisoning is apparently rare, suggested by the fact that reviews highlight individual cases. In 2014, an infant died from choking on an e-cigarette component.[119] As of 2016 four adults were reported to have died in the US and Europe after intentionally ingesting e-liquid.[120] Two children, one in the US in 2014 and another in Israel in 2013, died after ingesting liquid nicotine.[121] A two-year-old girl in the UK in 2014 was hospitalized after licking an e-cigarette liquid refill.[122]
A 2022 concluded that toxicity can come from aerosols containing toxic chemicals[123] or excessive concentrations of nicotine as an e-liquid.[94]
A 2014 review concluded that users may alter e-liquid contents, adding substances such as alcohol or nicotine, possibly making them toxic.[105]
As of 2014, calls to US poison control centers involved inhalations, eye exposures, skin exposures, and ingestion, in both adults and children.[124] A 2016 study reported minor, moderate, and serious adverse effects.[125] Minor effects correlated with e-liquid poisoning were tachycardia, tremor, chest pain and hypertension. More serious effects were bradycardia, hypotension, nausea, respiratory paralysis, atrial fibrillation and dyspnea.[126] Initial symptoms included rapid heart rate, sweating, feeling sick, and vomiting. Delayed symptoms included low blood pressure, seizures, and hypoventilation.[127] Rare serious effects included coma, seizure, trouble breathing, and heart attack.[128] After examining poison control centers' reports between 2010 and early 2019, FDA reported that, between the poison control centers and FDA, 35 cases of seizures mentioned use of e-cigarettes.[129]
From 2011-2019, cases of accidental poisoning from nicotine e-liquids grew rapidly in the US.[130] From September 1, 2010, to December 31, 2014, 58% of e-cigarette calls to US poison control centers were related to children under 6.[125] In 2014 Centers for Disease Control and Prevention (CDC) reported that 51.1% of the calls to US poison centers due to e-cigarettes were related to children under age 5, and while 42% of calls were related to people age 20 and older.[131] E-cigarette calls had a greater chance to report an adverse effect and a greater chance to report a moderate or major adverse effect than traditional cigarette calls.[125][clarification needed] Severe outcomes were more than 2.5 times more frequent in children exposed to e-cigarettes and nicotine e-liquid than with traditional cigarettes.[132]

US poison control centers reported that 92.5% of children who came in contact with nicotine e-liquid swallowed it during the period from January 2012 to April 2017.[128]
| Effect | Frequency (%) |
|---|---|
| vomiting | 40.4 |
| eye irritation or pain | 20.3 |
| nausea | 16.8 |
| red eye or conjunctivitis | 10.5 |
| dizziness | 7.5 |
| tachycardia | 7.1 |
| drowsiness | 7.1 |
| agitation | 6.3 |
| headache | 4.8 |
| cough | 4.5 |
In 2016 American Association of Poison Control Centers (AAPCC) reported 2,907 exposures regarding e-cigarettes and liquid nicotine.[133] The yearly nicotine exposure rate in the US involving children went up by 1,398% from 2012 to 2015, later dropping by 20% from 2015 to 2016.[128] In 2017 the National Poison Data System stated that exposures to e-cigarettes and liquid nicotine among young children was rising significantly.[134]
Respiratory
[edit]As of 2015, the long-term lung function effects of vaping were unknown.[135][81]: 12 A 2014 study reported that limited evidence suggests that e-cigarettes produce less short-term effects on lung function than traditional cigarettes.[136] As of 2015 many e-liquid ingredients had not been examined in the lung.[106]
As of 2017 e-cigarette effects on asthma and other respiratory diseases had not been assessed.[12][137]
A 2015 review concluded that e-cigarettes may induce acute lung disease.[135]
A 2018 study reported correlations between vaping and pleural effusions.[138] A 2015 study reported that e-cigarette vapors can induce oxidative stress in lung endothelial cells.[94] A 2016 review concluded that e-cigarette vapor that triggered constant lung inflammation could result in lung pathogenesis and induce diseases such as chronic obstructive pulmonary disease and fibrosis.[120] A 2018 review concluded that e-cigarette vapors can result in acute endothelial cell injury, but the long-term effects were uncertain.[99]: Summary, 7 A 2017 review concluded "Exposure to nicotine that was specifically generated by the use of e-cigarettes, was shown to promote oxidative stress and impairment of autophagy, which in turn serves as a potential mechanism leading to development of chronic obstructive pulmonary disease."[139] A 2014 case report observed the correlation between sub-acute bronchiolitis and vaping.[135] After quitting vaping the symptoms improved.[135] Vaping causes bronchospasm.[102] Adolescents who vaped had a higher frequency of chronic bronchitis symptoms.[140]
A 2015 review reported that the long-term effects regarding respiratory flow resistance were unknown.[97] A 2014 review concluded that e-cigarettes reduced lung function, but much less than traditional cigarettes.[141] A 2015 clinician's guide stated that 5 minutes of vaping considerably increased lung airflow resistance.[92] A 2013 review concluded that a single e-cigarette increased airway resistance.[142]
A 2014 study reported higher levels of exhaled nitric oxide, which was associated with lung inflammation.[143] A 2014 review concluded that harmful effects to cardiovascular and respiratory functions after short-term use of e-cigarettes were appreciably milder than traditional cigarettes.[11] A 2015 review concluded that short-term use increased respiratory resistance comparatively [sic][citation needed] to traditional cigarettes.[97]
A 2018 study reported that adolescent vapers with asthma or other respiratory ailments could have greater odds of increasing respiratory symptoms and aggravations.[99]: Vulnerable/Susceptible Populations, Cystic Fibrosis, 448 In 2018 PHE reported "There have been some studies with adolescents suggesting respiratory symptoms among EC experimenters. However, small scale or uncontrolled switching studies from smoking to vaping have demonstrated some respiratory improvements."[144]{: 174 A 2017 review concluded "among a population of 11th-grade and 12th-grade students in California, vaping was associated with twice the risk of respiratory symptoms, and the risk increased with more frequent e-cigarette use."[145]
E-cigarette particles are small enough to enter the alveoli and to go deep in the lungs and enter into systemic circulation.[15] A 2017 study reported that vapor containing particulate matter with a diameter of 2.5 μm enters the circulation via the cardiopulmonary system, with a large deposit in the respiratory tract.[102] A 2014 review concluded that metal nanoparticles can deposit in the alveolar sacs with possible pulmonary toxicity.[15] A 2015 study reported that particle sizes differ across devices with impacts on respiratory tract depositions, and without regard to e-liquid.[146]
A 2019 case study of hard-metal pneumoconiosis cannabis vapers reported cobalt, nickel, aluminum, manganese, lead, and chromium in the vapor. Metal-induced toxicity in the lung can result in long-term/permanent lung scarring.[147]
A 2018 review concluded that exposure to vapor has adverse effects on lungs and pulmonary function. Repeated acrolein exposure causes chronic pulmonary inflammation, reduction of host defense, neutrophil inflammation, mucus hypersecretion, and protease-mediated lung tissue damage, which are linked to the development of chronic obstructive pulmonary disease (COPD).[82] Although e-cigarette aerosol also exposes users to highly oxidizing free radicals,[82] their chemical characteristics is unclear.[148]
It further reported that vapers experienced decreased expression of immune-related genes in their nasal cavities, more so than smokers. By contrast, vaping upregulates expression of platelet-activating factor receptor (PAFR) in nasal epithelial cells; PAFR is an important molecule involved in the ability of S. pneumoniae, (leading cause of bacterial pneumonia), to attach to cells.[82]
A 2020 study reported that vaping led to lung injuries that include hypersensitivity pneumonitis (HP), diffuse alveolar hemorrhage (DAH), acute eosinophilic pneumonia (AEP), diffuse alveolar damage, organizing pneumonia (OP), lipoid pneumonia, and giant cell interstitial pneumonia (GIP).[149]
Adolescents
[edit]vaping is associated with a positive association of vaping and chronic bronchitis among US high school juniors and seniors; which persisted among former users. Vaping was associated with an increased diagnosis of asthma and asthma-related school absences among Korean never-smoker high school students.[82]
2019–2020 vaping lung injury outbreak
[edit]
An outbreak of e-cigarette, or vaping, product use-associated lung injury (EVALI) began in 2019[151] among users of illegal, unregulated cannabis vaping products,[150] almost exclusively in the United States.[152] The first cases were identified in Illinois and Wisconsin in April 2019; as of 18 February 2020, a total of 2,807 hospitalized cases, including 68 deaths, had been confirmed. According to the U.S. Centers for Disease Control (CDC), "Vitamin E acetate is strongly linked to the EVALI outbreak...Evidence is not sufficient to rule out the contribution of other chemicals of concern, including chemicals in either THC or non-THC products".[150]
Cases peaked in September 2019, and declined thereafter. The decline led CDC to stop reporting EVALI cases in February 2020, but as of December 2020, continued to monitor cases arriving in emergency departments.[153] Some states continued to record new EVALI cases. As of January 2022, California had reported at least 40 cases diagnosed after February 2020.[154] As of March 2022, EVALI cases continued to be diagnosed.[155] At least 73 cases were diagnosed in Utah after February 2020.[156]
CDC investigators identified direct exposure to chemicals present in illegal cannabis vaping products as the likely culprit, but did not rule out chemicals in nicotine vapes as possible causes.[157] CDC: "No specific e-cigarette device or substance has been linked to all cases, and e-cigarettes include a variety of chemical and additives".[150] 84% of patients studied by the CDC reported THC use.[153][150] The majority of those affected were adults aged 18–34, the biggest cannabis vapers in the U.S.[158]Cardiovascular
[edit]A 2018 review concluded that the specific role of nicotine in cardiovascular disease had not been established.[82]
A 2023 review concluded that vaping causes significant, potentially harmful effects on many cardiovascular parameters.[159] A 2024 review attributed cardiovascular effects to oxidative stress, inflammation, endothelial dysfunction, atherosclerosis, hemodynamic effects, and platelet function.[160] A 2019 review reported limited evidence of vaping's adverse impacts on endothelial function and arterial hardening.[161] A 2017 review concluded that vaping could exacerbate adverse cardiovascular effects among those who already have cardiovascular disease. Studies of aldehydes, particulates, and flavorings reported mixed impacts on cardiovascular health.[148] A 21017 review stated that low amounts of aldehydes are a health concern, particularly among individuals with cardiovascular disease.[102] A 2014 review concluded that while vaping reduces cardiac muscle function and increases inflammation, these changes were non-significant.[141] A 2017 review concluded that vapor particles can enter circulation via the airways.[102]
Many vapor components impact atherosclerosis.[162] Case reports from 2014 documented possible cardiovascular adverse effects, mostly via improper use. However ,these effects were reduced compared to traditional cigarettes.[163]
A 2016 review concluded that vaping generates sympathomimetic effects.[164] A 2016 review concluded that there could be a risk for conditions such as tachycardia-induced cardiomyopathy.[164] A 20154 clinician's review reported that short-term effects included increases in blood pressure and heart rate.[135] A 2017 review concluded that these increases among smokers who vaped was lower than with smoking.[102] A 2016 study reported vaping increased aortic stiffness in people with no cardiovascular risk factors, an d that the increase was lower than smoking.[148] A 2017 review concluded that habitual vaping was associated with oxidative stress and a shift towards cardiac sympathetic activity, which are both associated with a risk of developing cardiovascular disease.[139][82] A 2017 review highlighted an association between 2.5 μm particulate exposure and cardiovascular disease.[102]
A 2018 review noted that nicotine is not the only biologically active component in e-cigarette aerosol. Vapor particles are of broadly similar size to those in traditional cigarettes. These particles can be biologically active, trigger inflammatory processes, and are directly implicated in causing cardiovascular disease and acute cardiovascular events. Their dose-response effect is nonlinear, with substantial increases in cardiovascular risk with even low exposure levels. Vapor induces platelet activation, aggregation, and adhesion, which are associated with increased cardiovascular risk. These changes produce rapid deterioration of vascular function. E-cigarette and traditional cigarette smoking in individuals with no known cardiovascular disease exhibit similar inhibition of artery dilation in response to the need for more blood flow. This change reflects damage to vascular endothelium and increases the risk of long-term heart disease and an acute event such as a myocardial infarction (heart attack). Vaping is accompanied by a shift in balance of the autonomic (reflex) nervous system toward sympathetic predominance, which is also associated with increased cardiac risk. Daily vaping is correlated with an increased risk of myocardial infarction in health surveys.[82]
Other
[edit]Gastrointestinal (GI) System
[edit]A mucosal intestinal barrier separates the external and internal environments within the body. This barrier allows water, ions, solutes, and nutrients to cross the barrier while excluding bacteria and toxins.[165] Tight junctions (TJ) help with the construction and permeability of the barrier in the gut by firmly securing joints.[166] Chronic, repetitive exposure to e-cigarettes damages this barrier by breaking the TJs, which causes gut inflammation, ,assage of bacteria.[167] altering gene expression.[166][167] A 2021 study reported that chronic use of nicotine-free e-cigarettes still caused inflammation and decreased TJ markers.[168]
A 2022 study reported that cmmon GI health effects include nausea, vomiting, gastrointestinal discomfort, xerostomia, oral mucositis, gum bleeding, gingivitis, gastric burning, altered bowel habits, and acid reflux. Chronic exposure also drives inflammation in the colon.[169]
Nervous System
[edit]A 2024 review concluded that nicotine exposure has detrimental effects on the nervous system, especially during adolescence. Exposure during developmental stages changes brain structure and function. Vaping is linked to impairment of cognitive processes, increased mood disorders and addiction, damage to functions such as memory, reasoning, impulse control, and attention.[170] A 202 study reported lower gene expression, reducing occludin, which compromises the stability and strength of the blood-brain-barrier, resulting in neurovascular dysfunction, neuroinflammation, and cognitive defects.[171] A 2010 study reported that short-term nicotine use excites the autonomic ganglia nerves and autonomic nerves.[172]
Oral Cavity
[edit]A 2018 review reported little evidence indicating that vaping is less damaging than smoking for periodontal disease[99]: Summary, Conclusion 12-1., 9 and can lead to increased risk of periodontal disease.[173]j A 2017 review concluded that nicotine and flavorings may damage periodontal ligaments, stem cells, and gingival fibroblasts in cultures from aldehydes and/or carbonyls from vapor.[173] A 2016 clinicians guide state that e-cigarettes could harm the periodontium because of the effects of nicotine on gum tissues and the immune system.[174] A 2021 study reported that vaping resulted in nicotine stomatitis, hairy tongue, angular cheilitis,[175] and oral mucosal lesions.[176] E-cigarettes are not implicated in cancer.[175]
Cannabinoids
[edit]Cannabinoid-enriched e-liquids require sophisticated processing, and may lack information on quality control, expiry date, conditions of preservation, or toxicological/clinical assessment. It is assumed that vaporizing cannabinoids at lower temperatures is safer because it produces smaller amounts of toxicants than a traditional cigarette. As of 2015 the health effects specific cannabinoid vaping were unknown.[177] However, cannabinoid e-cigarettes mixed with other diluents and chemicals was associated with EVALI,[123] although a 2017 study rejected this.[178]
Public health effects
[edit]Various studies rate the public health impacts of vaping as far less negative than those of smoking.[179]
Second-hand vapor
[edit]E-cigarette emissions are not comparable to cigarette smoke as their chemical composition is completely different.[11] Vapor content varies depending on the e-liquid, the device, and usage.[180] : 84 [102] Exhaled vapor consists of mixtures of nicotine, ultrafine particles, primarily propylene glycol, glycerin, flavorings, and aroma transporters,[12] aldehydes,[102] and volatile organic chemicals (VOC)[163] that form a visible fog.[142] The vapor has a half-life of about 10 seconds; smoke last 100 times longer.[142] A 2014 study reported that e-cigarettes increased levels of carcinogenic polycyclic aromatic hydrocarbons in the surrounding air.[181]
Vapor particles are larger than smoke particles, with a mean droplet size of 600 nm (inhaled) and 300 nm (exhaled)[142] along with particles with a diameter of around 2.5 μm.[102] Exhaled vapor concentration is 5 times lower than cigarette smoke.[136] Particle density measured 6 to 880 times lower.[121][11]
One 2015 study reported that exhaled vapor might have significant adverse effects.[93] Another reported that e-cigarettes that do not contain nicotine may also generate hazardous vapors[182] and could present a second-hand risk.[183] A third reported that vapor may include propylene glycol aerosols at levels that can cause eye and respiratory irritation and exceed California Environmental Protection Agency standards.[184] A 2017 study reported that people living with e‐cigarette users had increased salivary nicotine concentrations.[102] Another reported that some non-users reported adverse effects from second-hand vapor.[7]
A 2016 survey reported that nearly half of middle and high school students had been exposed.[102]
As of 2014 neither the long-term[15] nor short-term[185][186] health effects from exhaled vapor were known. A 2017 review concluded that the few studies that examined the effect of indoor air quality on human test subjects in natural settings produced inconsistent results.[143] As of 2018 limited only information of the effects of exhaled vapor on children was available.[187]

Between January 2012 and December 2014, FDA published 35 adverse effect reports regarding second-hand vapor exposure.[189]
A 2018 study reported PM2.5 levels in a large hotel event room (4,023m3) increased from 2–3 μg/m3 to as high as 819 μg/m3 (interquartile range: 761–975 μg/m3) when 59–86 people were vaping. This level exceeded the US Environmental Protection Agency annual time-weighted standard for PM2.5 of 12 μg/m3.[82]
A 2018 review concluded that bystanders absorb nicotine when people around them use e-cigarettes at levels comparable with exposure to second-hand smoke. It included a study comparing non-smokers living with vapers, with smokers, and non-users (controls). That study found cotinine (a nicotine metabolite) levels in urine were significantly elevated in the first two groups vs the controls, but were not significantly different, despite the fact that air pollution levels in the smokers' homes was much higher than in the vapers' homes (geometric mean air nicotine concentrations of 0.13 μg/m3 in vapers' homes, 0.74 μg/m3 in smokers' homes, and 0.02 μg/m3 in the control homes).[82][136] A 2014 practice guideline by NPS MedicineWise stated that serum cotinine levels were similar in bystanders exposed to either vapour or smoke.[190]
In 2014, several groups came out against e-cigarettes. The International Union Against Tuberculosis and Lung Disease stated, "Adverse health effects for exposed third parties (second-hand exposure) cannot be excluded because the use of e-cigarettes leads to emission of fine and ultrafine inhalable liquid particles, nicotine and cancer-causing substances into indoor air."[191] The American Industrial Hygiene Association concluded that "e-cigarettes are not emission-free and that their pollutants could be of health concern for users and those who are exposed secondhand....[T]heir use in the indoor environment should be restricted, consistent with current smoking bans, until and unless research documents that they will not significantly increase the risk of adverse health effects to room occupants."[192] Similarly, in 2016 the American Society of Heating, Refrigeration and Air-Conditioning Engineers (ASHRAE) updated its standard for "Ventilation for Acceptable Indoor Air Quality" to incorporate emissions from e-cigarettes into the definition of "environmental tobacco smoke," which is incompatible with acceptable indoor air quality. A 2017 French "experts statement" recommended banning vaping indoors in public and working areas.[193]
A 2014 WHO report stated passive exposure was a concern, indicating that current evidence is insufficient to determine whether the levels of exhaled vapor are safe to involuntarily exposed bystanders.[6] The report stated that "it is unknown if the increased exposure to toxicants and particles in exhaled aerosol will lead to an increased risk of disease and death among bystanders."[6] A 2016 WHO report stated, "While some argue that exposure to SHA [second-hand aerosol] is unlikely to cause significant health risks, they concede that SHA can be deleterious to bystanders with some respiratory pre-conditions. It is nevertheless reasonable to assume that the increased concentration of toxicants from SHA over background [air] levels poses an increased risk for the health of all bystanders."[194]: 4
A 2013 British Medical Association (BMA) report stated "concerns that the use of e-cigarettes could threaten the norm of not smoking in public places and workplaces".[195] Several medical organizations advocate that vaping be banned in public places and workplaces.[196] A 2014 review concluded it is safe to infer that their effects on bystanders are minimal in comparison to traditional cigarettes.[11] E-cigarette vapor has notably fewer toxicants than cigarette smoke.[15]

A 2015 California Department of Public Health report stated that vapour "has been reported to contain at least ten chemicals that are on California's Proposition 65 list of chemicals known to cause cancer, birth defects, or other reproductive harm."[197]: 1
A 2017 study reported that some chemicals could violate workplace safety standards.[137] A review of convention studies concluded that second-hand vapor may be significant, particularly for workers who repeatedly encounter it. Exposure studies suggest that indoor vaping is higher than the smoke-free level put forth by the US Surgeon General and the WHO Framework Convention on Tobacco Control.[99]: Secondhand Exposure to E-Cigarette Aerosol, Synthesis, 84
By contrast, a 2014 review concluded that vaping probably much less harmful than traditional cigarettes.[12] Another 2014 review suggested that vapor contaminant levels do not exceed workplace safety standards,[198] and are mostly below 1% of permissible levels.[198] However, workplace standards do not consider more vulnerable groups such as those in poor health, children, and infants.[15] 2 015 PHE report concluded that e-cigarettes "release negligible levels of nicotine into ambient air with no identified health risks to bystanders".[81]: 65
Direct exposure
[edit]Direct exposure happens via e-liquid inhalation, ingestion, skin contact, or vapor residue accumulation on surfaces.[13] Direct exposure is almost always inadvertent, and results from improper product use. Exposure can involve much higher concentrations than exhaled vapor.[93]
Exposure may involve a leaking or spilled e-liquid cartridge or bottle.[95]
E-liquid quickly absorbs into the skin[199] and local irritation can follow.[200] Less than 1 tablespoon can cause adverse effects such as seizures, anoxic brain trauma, vomiting, lactic acidosis,[99]: Summary, Conclusion 14-2., 9 cardiac arrest, seizures, or coma.[201] A potentially fatal dose for a child is 0.1–0.2 mg/kg of body weight,[93] or 6 mg.[76][202] A fatal dose for an adult is 0.5–1 mg/kg[93] or about 30–60 mg.[203] However the widely-used human LD50 estimate of around 0.8 mg/kg was questioned in a 2013 review, in light of documented cases of humans surviving much higher doses; the lower fatal limit was 500–1000 mg of ingested nicotine, which is equivalent to 6.5–13 mg/kg orally.[204]
Vapor build-up
[edit]E‐cigarettes can be unsafe to non-users via third-hand exposure, including children, pregnant women, nursing mothers,[93] casino employees, housekeeping employees, and vulnerable groups.[102]
In one scenario, indoor surfaces can accumulate nicotine-laden vapor residue.[205] However, the extent of such contamination has not been established. A 2015 PHE report stated that an infant would have to lick 30 square meters to be exposed to 1 mg of nicotine.[81]: 65 As with any potential hazard, childhood exploratory behavior creates risks not faced by others.[184][206]
Risks to children
[edit]Children are more likely to mistake a colorful e-liquid container for a juice container.[132][98][125][207][121][208][209] The US mandates child-proof packaging.[210]
Self-harm
[edit]As of 2019 a few incidents of intentional self-harm by ingesting or injecting e-liquids had been reported.[147][211][129][120][14][120] Death from intentional nicotine poisoning is almost unknown.[81]: 63
Pets
[edit]In 2017, FDA stated that e-cigarette aerosols can cause problems for both users and their pets. Some studies reported that aerosols may provide exposure to higher-than-normal amounts of nicotine and other toxic chemicals, such as formaldehyde. E-cigarettes typically use capsules to contain nicotine.[212] Pets may find and bite them or expose themselves to the liquid refilling solution. In a March 15, 2016, letter to the editor of the Journal of the American Veterinary Medical Association, the Texas Poison Center Network[213] reported 11 cases of dog exposures to e-cigarettes or refills.[212] The Animal Poison Control Center stated that among nicotine toxicity cases in 2012, 4.6% related to e-cigarettes, which increased to 13.6% in 2013.[214]
Toxicology
[edit]The long-term health impacts of vaping are unknown,[12] particularly given the variety of EC devices, e‑liquids, and consumption patterns.[148] This specifically applies to nicotine and propylene glycol.[215] Limited peer-reviewed data restricts the scope of toxicological evaluation;[216] their cytotoxicity is unknown.[217] A 2014 review concluded that few e-cigarettes had undergone a thorough toxicology evaluation and testing.[218] A 2013 study claimed that they were similar in toxicity to other nicotine replacement products,[219] but this was disputed.[81]: 87 In 2013 the UK National Health Service noted that toxic chemical levels were 0.1% of cigarette smoke.[220]
Carcinogenicity
[edit]Concerns about carcinogenicity arise from both nicotine[221] and from other vapor chemicals.[1]
Nicotine
[edit]Evidence from in vitro and animal research does not indicate carcinogenicity in vivo.[221] A 2014 Surgeon General report stated that the only relevant randomized trial "does not indicate a strong role for nicotine in promoting carcinogenesis in humans". It concluded that data is insufficient "to conclude that nicotine causes or contributes to cancer in humans, but there is evidence showing possible oral, esophageal, or pancreatic cancer risks".[222] : 116 However, a 2014 study suggested that vaping may be a risk factor for lung cancer.[74] Nicotine in the form of nicotine replacement products is reported to be less of a cancer risk than smoking,[81]: 115 and they vaping had not been shown to be associated with cancer.[221]
As of 2015 it was not possible to conclude that nicotine itself is a complete carcinogen. In mice studies with NNK as an initiator, nicotine was reported to act as a promoter after injection or dermal absorption, but not after oral administration. In drinking water experiments, considerable first-pass metabolism of nicotine occurred before nicotine entered systemic circulation. As a result, serum concentration is much lower after ingestion than after intraperitoneal injection administration.[223]
However, nicotine has been reported to promote metastasis by causing cell cycle progression, epithelial-to-mesenchymal transition, migration, invasion, angiogenesis, and avoidance of apoptosis.[224] Nicotine promotes the growth of blood vessels, which can supply tumors and speed tumor growth.[82] As of 2015, long-term vaping had not been assessed for malignancy in individuals with a susceptibility for tumor growth.[146] The effects of nicotine on the sympathoadrenal system could stimulate growth in cancers already present.[225]
Potential accelerant
[edit]Multiple in vitro experiments reported that nicotine in concentrations as low as 1 μM decreased the anti-proliferative and pro-apoptotic effects exerted by chemotherapeutics on multiple malignant cell lines. These effects were partially reverted by exposure to α-bungarotoxin (α-BTX), a α7-nAChR inhibitor. During radiotherapy (RT), nicotine administration was reported to increase survival of H460 and A549 lung cancer cells. This effect was likewise reduced by addition of α-BTX prior to nicotine addition and radiation. On this basis, it may be expected that use of nicotine products during cancer treatment reduces the effects due to reactions following interaction of nicotine with α7-nAChR.[223]

Evidence from in vitro studies on cell cultures, rodents and humans inclusive of epidemiological studies indicate that nicotine may contribute in cancer development by stimulating important processes. Nicotine acts primarily by activation of nicotine acetylcholine receptors (NAR) and nicotine binds to these receptors with a higher affinity than acetylcholine. Furthermore, the tobacco-specific nitrosamines (TSNAs) NNN (N′-nitrosonornicotine) and the potent lung carcinogen NNK (4-(metylnitrosamino)-1-(3-pyridyl)-1-butanon) may be formed from nicotine after oral administration.[223] E-cigarettes deliver NNK. Some evidence indicates that the NNK dose-response curve for cancer is highly nonlinear, with substantial risk at low doses.[82]
A 2015 study reported that urine from vapers had low levels of NNAL (4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol), which may suggest that endogenous formation of TSNA after nicotine inhalation is negligible. That data indicates that TSNA may be formed internally after absorption of nicotine through the oral mucous membranes and through the skin, while formation after lung absorption may be negligible. Thus, the toxicokinetics of nicotine may depend on the administration route.[223]
The interaction of nicotine with NARs activates signaling pathways that trigger multiple reactions, such as increased cell proliferation and cell survival. Although NARs are the primary receptors, nicotine binding to β-ARs and EGFRs may also be important. Nicotine induces epithelial–mesenchymal transition, which is one of the vital steps for the acquisition of malignant phenotype. This transition allows the cell to acquire migratory properties, which may facilitate cancer metastases.[223]
In May 2014, Cancer Research UK stated that very preliminary unpublished results "suggest that e-cigarettes promote tumour growth in human cells."[215]
Nicotine enhanced tumor growth and progression after injection of malignant cells in mice. Enhancements were reported both after exposure by intraperitoneal injection, oral, and skin administration. Moreover, cotinine did also enhance tumor growth. Nicotine may inhibit antitumor immune response. It has been reported that exposure to nicotine adversely affects dendritic cells, a cell type that has an important role in anticancer immunosurveillance. Moreover, in studies on xenograft in mice, nicotine was reported to reduce the effects of radiotherapy and chemoradiotherapy.[223]
No long-term research considers the cancer risk related to the relatively small level of exposure to the identified carcinogens in e-cigarette vapor.[136][135] Their long-term use is anticipated to raise the risk of developing lung cancer.[226]: 3 A 2015 study reported carcinogenicity was mainly evident in the lungs, mouth, and throat, which may be associated with nitrosamines, propylene glycol, and some flavoring additives.[102] A 2019 review associated vaping with a possible risk of head and neck cancers.[227]
Since e-liquids are made from tobacco they may contain impurities such cotinine, anabasine, anatabine, myosmine and beta-nicotyrine.[12] The health implications of suchimpurities are not known.[184] A 2016 review concluded, "impurities and nicotine degradation products such as nicotine-cis-N-oxide, nicotine-trans-N-oxide, myosmine, anabasine, and anatabine, which are very carcinogenic, can be reported in e-cigarette refill liquids. The molecules can lead to mutations in genes such as Ras (vital function in signal transduction of cell proliferation), p53 and retinoblastoma (with roles as tumour suppressors) as these molecules can form adducts with cellular DNA."[98] The majority of e-cigarettes evaluated included carcinogenic TSNAs; heavy metals such as cadmium, nickel, and lead; and the carcinogen toluene.[93] However, in comparison to traditional cigarette smoke, the toxic substance levels identified in e-cigarette vapor were 9- to 450-fold less.[93]
Nicotine promotes endothelial cell migration, proliferation, survival, tube formation, and nitric oxide (NO) production in vitro, mimicking the effect of other angiogenic growth factors. In 2001, it was reported that nicotine was a potent angiogenic agent at tissue and plasma concentrations similar to those induced by light to moderate smoking. Angiogenic effects on tumor cells were found in breast, colon, and lung cancers. Similar results were demonstrated in in vivo mouse models of lung cancer, where nicotine significantly increased tumor size and numbers in the lung, and enhanced metastasis. At high enough concentration levels, nicotine becomes cytotoxic.[223]
DNA damage
[edit]Nicotine has been reported to damage DMA, assessed by the Escherichia colipol A+/pol− test.[223] A 2015 review concluded that nicotine decreases tumor suppressor Chk2, which is otherwise activated by DNA damage.[223] The Chk2 decrease suggests that nicotine may be capable of overriding DNA damage checkpoint activation, disrupting genetic surveillance, and increasing oncogenesis risks.[223] One 2018 study reported strong evidence that some vapor substances such as formaldehyde and acrolein can induce DNA damage and mutagenesis.[99]: Summary, Conclusion 10-4., 8
Nicotine can induce chromosomal aberration, chromatid exchange, single-strand DNA strand breaks, and micronuclei in vitro. Oxidative stress is probably involved since the effects are reduced in the presence of antioxidants. The effects decrease after co-incubation with a NAR antagonist, indicating a receptor-dependent pathway for oxidative stress induction.[223]
Vapor triggered DNA strand breaks and lowered cell survival in vitro,[120] regardless of nicotine content.[122] A 2013 study reported that some vapor samples had cytotoxic effects on cardiac muscle cells, (albeit less than those of cigarette smoke).[228] A 2016 review concluded that vapor had adverse effects on primary airway epithelial cells and tumor cell lines, and other epithelial cell lines, that ranged from reducing viability, increase in production of inflammatory mediators and oxidative stress, reduced antimicrobial defences and increased pro-carcinogenic events.[229]

Propylene glycol and glycerin
[edit]
The primary base ingredients of e-liquids are propylene glycol and glycerin.[15] About 20% to 27% of propylene glycol and glycerin-based liquid particles are inhaled.[231] A 2016 study reported that 6% of nicotine, 8% of propylene glycol, and 16% of glycerin was exhaled.[81]: 162 As of 2014 the long-term effects of inhaled propylene glycol[207][179] and glycerin were unknown.[202] Exposure to propylene glycol may cause eye and respiratory tract irritation.[15] Heated and aerosolized propylene glycol can turn into propylene oxide, which the International Agency for Research on Cancer (IARC) labels a possible human carcinogen.[15][122] A 2014 review concluded that the risk from propylene glycol and glycerin inhalation is probably low,[12] although they have not been demonstrated to be safe.[202] A 2013 German Cancer Center report stated that long-term indoor inhalation of propylene glycol could increase childhood asthma risks.[76] As of 2014, some companies replaced propylene glycol with water and glycerin.[65] A 2019 study reported that inhaled glycerin could cause lipoid pneumonia.[232] A 2017 review concluded that propylene glycol and glycerin increased the amount of hydrogen peroxide.[139][clarification needed]
Acrolein
[edit]Some e-liquids produced acrolein in the aerosol[12] (a probable carcinogen),[233] possibly from heated glycerin.[12] A 2014 review concluded that acrolein levels were reduced by 60% in dual users and 80% for those that completely switched to e-cigarettes when compared to traditional cigarettes.[12] Another 2014 review concluded that acrolein may induce irritation to the upper respiratory tract,[15] while a 2014 study reported harm to the lining of the lungs.[234] A 2017 review concluded that acrolein induces oxidative stress and inflammation, disrupting lung endothelial cell barrier function and may lead to chronic obstructive pulmonary disease.[139] Another 2017 review stated, "based on the average of 120 puffs/day reported in the literature, our calculated levels of acrolein emitted by e‐cigarette users per day were reported to vary between 0.00792 and 8.94 ppm/day."[102]
Oxidants/reactive oxygen species
[edit]A 2015 study reported that vapor created oxidants and reactive oxygen species (OX/ROS). OX/ROS could react with other vaporized substances because they are highly reactive. E-cigarettes were reported to contain OX/ROS at about 100 times less than in cigarette smoke.[106] A 2014 study reported that e-liquids from a specific manufacturer contained greater amounts of ethylene glycol than glycerin or propylene glycol, although ethylene glycol was not permitted for use in products meant for human consumption.[235]
Flavorings
[edit]
Flavored e-liquids contain additional substances in part to disguise nicotine's bitter taste.[142][106] Their health effects are not entirely known,[236] given limited toxicological data.[137] A 2017 study reported that flavorings can be a significant part of toxicants.[237] Each flavoring has a different chemical composition.[237] A 2015 study reported varied cytotoxicity of e-liquids,[238][142] ranging from little to significant cytotoxicity.[238] The liquids contain aromatic substances such as tobacco, fruit, vanilla, caramel, and coffee.[142] Typically, these additives are imprecisely described, using terms such as "vegetable flavoring". Although they are approved for human consumption no studies assess the short-term or long-term effects of inhaling them.[142][73] As of 2016 their safety had not been assessed by the US Flavor and Extract Manufacturers Association (FEMA).[120] As of 2018 the majority of flavorings in e-liquids had not been investigated for inhalation toxicity.[99]: Summary, 4 A 2017 review stated that FEMAhad identified 1037 flavoring agents as potential respiratory hazards due to volatility and respiratory irritant properties. Common flavoring agents on that list include diacetyl, acetoin, 2,3-pentanedione (buttery), camphor and cyclohexanone (minty), benzaldehyde (cherry or almond), cinnamaldehyde (cinnamon), cresol (leathery) or medicinal (chocolate), and isoamyl acetate (banana).[137] As of 2017 the four most commonly reported flavoring additives were vanillin, ethyl maltol, ethyl vanillin, and menthol.[139] A 2017 review stated, "the implication by manufacturers that flavoring ingredients used in e-cigarettes and related devices (e.g. hookahs) are safe for inhalation because they have FEMA GRAS™ status for use in food has been stated to be 'false and misleading' by FEMA."[239]
Many flavorings are irritants.[226] : 3 The limited available data suggest that the majority of flavorings could lead to significant health risks from long-term use, particularly those that are sweet.[196] Some e-liquids contain large amounts of flavorings.[94] A 2016 study of 30 e-cigarette products in the US market reported that 13 were more than 1% flavoring chemicals by weight, some of which were of potential toxicological concern (e.g., cause respiratory irritation).[240] Some flavorings are toxic and some resemble known carcinogens.[142] A 2016 study of five flavorings across six types of e-cigarettes reported that flavorings significantly affected the in vitro toxicity profile.[240] Some artificial flavorings are known cytotoxins.[142] Unflavored vapor is less cytotoxic than flavored vapor.[180]: 82 A 2012 study reported that in embryonic and adult cellular models, some flavorings not reported in tobacco smoke were cytotoxic.[241] The caffeine exposures from vaping are considerably less than caffeinated beverages. Limited information is available regarding the effects of inhaling caffeine.[99]: Other Toxicants, Caffeine, 197 The evidence is unclear that particular flavorings carry health risks, though some may increase such risks.[81]: 19
Cinnamaldehyde has been described as highly cytotoxic.[92] Cinnamaldehyde has been detected in flavorings such as cinnamon, tobacco, sweet (e.g. caramel), and fruit.[99]: Exposure to Flavorings, 175 A 2014 review concluded that cinnamaldehyde was cytotoxic at amounts 400 times less than those allowed EPA.[11] Coffee and cinnamon flavorings are reported to be the most toxic.[242] A 2017 review concluded that they were carcinogenic or toxic, and could contribute to cardiopulmonary diseases and neurodegenerative disorders.[139] Only sparse evidence directly associates cinnamon inhalations with asthma.[137] Some e-liquids containing cinnamaldehyde stimulate TRPA1, which might induce effects on the lung.[106] In human lung fibroblasts, cinnamon roll flavoring resulted in a noticeable rise in the amount of inflammatory cytokine IL-8.[139]
A 2019 case report described an 18-year-old patient using a Juul device with mint-flavored pods in the days before episodes of pneumothorax.[243] A 2019 study that sampled e-cigarette delivery systems reported that Juul pods were the only product to demonstrate in vitro cytotoxicity from both nicotine and flavoring chemical content, in particular ethyl maltol.[243] As of 2017 limited data described the effects of menthol inhalation.[137] Some flavorings may increase lung toxicity[239] or lung inflammation[140] in part by producing free radicals and inflammation.[122]
E-liquids contain possibly toxic aldehydes and reactive oxygen species (ROS).[106] Many flavorings are known aldehydes, such as anisaldehyde, cinnamaldehyde, and isovaleraldehyde.[106] Saccharides in sweet e-liquid flavorings generate furans and aldehydes when vaporized.[99]: FLAVORINGS, 172 The consequences of aldehyde-containing flavorings on pulmonary surfaces are unknown.[106] A 2012 study reported that butterscotch flavoring was highly toxic with one liquid while two others had low toxicity.[211] A 2014 in vitro study showed that menthol flavorings have a damaging effect on human periodontal ligament fibroblast growth.[231] Methanol increased the amount of hydrogen peroxide.[139] A 2017 study reported a variety of flavoring-initiated inflammatory cytokines in lung cell cultures, of which acetoin and maltol were among the strongest.[140] A 2014 in vitro study demonstrated that vaping of a balsamic flavoring without nicotine activated the release of proinflammatory cytokines in lung epithelial cells and keratinocytes.[93] Other additives may reduce the irritation on the pharynx.[202] It is possible that flavorings may worsen harmful effects such as diminished cell viability, escalated rates of apoptosis, escalated DNA strand breaks, alterations in cell morphology and intensified inflammatory mediator production.[237]
Flavorings that contain diacetyl and acetyl propionyl are used for butter, chocolate, milk, toffee,[244][242] or menthol flavorings.[140] Diacetyl occurs in flavorings such as caramel, butterscotch, watermelon, pina colada, and strawberry.[140] A 2016 study reported that 39 of 51 flavored e-cigarettes contained diacetyl.[245] The American Lung Association recommended in 2016 that the FDA require that diacetyl and other chemicals be banned from e-cigarettes.[245] Diacetyl and acetyl propionyl are associated with bronchiolitis obliterans.[244] A 2018 PHE report stated that e-liquids containing diacetyl are not likely to present a considerable risk.[81]: 159 A 2015 review recommended specific regulation of diacetyl and acetyl propionyl, which have been associated with respiratory harm when inhaled.[246] Exposure to diacetyl produces morphological liver alterations according to animal studies.[98] Diacetyl and acetyl-propionyl have been reported in concentrations above those recommended by the US National Institute for Occupational Safety and Health.[244] Diacetyl is reported at lower levels in e-cigarettes than in traditional cigarettes.[244]
2, 3-pentanedione is an α-diketone that is chemically and structurally similar to diacetyl. A 2016 report stated that it had become a popular replacement for diacetyl, although it had been shown to cause airway epithelial damage similar to diacetyl.[184] A 2016 review concluded that liquids that use butyric acid in place of diacetyl and acetyl propionyl, could have negative health effects.[247] Another 2016 review surfaced concerns that e-liquid additives might lead to diseases such as popcorn lung.[86]
Cherry flavorings contain a benzaldehyde,[242] a main ingredient for many fruit flavorings.[140] Benzaldehyde can irritate the eyes and respiratory mucous membranes.[248] The irritants butyl acetate, diethyl carbonate, benzoic acid, quinoline, bis(2-ethylhexyl) phthalate, and 2,6-dimethyl phenol were present as undeclared ingredients in the e-liquid.[77] A 2010 study reported weight loss drug rimonabant in e-liquids. The drug has been linked to seizures and suicides. The same study reported that e-liquid can contain amino-tadalafil which is a component of Cialis, used for erectile dysfunction. This and other pharmacologic compounds present some degree of risk.[99]: Other Toxicants, Pharmaceutical Drugs, 197
In 2015 CDC tested 36 e-cigarette products for 10 flavoring compounds commonly used as additives in tobacco products.[184] Measurable levels of eucalyptol and pulegone were reported in menthol-flavored varieties for all manufacturers.[184] Menthol concentrations ranged from 3,700 to 12,000 μg/g, similar to those reported in traditional cigarettes.[184] Menthol was reported at low concentrations in 40% of the tobacco-flavored nonmenthol products tested.[184] Other flavoring compounds reported were camphor, methyl, salicylate, pulegone, cinnamaldehyde (CAD), and eugenol. A 2016 study analyzed 30 e-cigarette products and reported that 13 contained more than 1% flavoring chemicals by weight.[184] Among the chemicals identified were aldehydes (e.g., benzaldehyde and vanillin), which are primary respiratory tract irritants.[184] Tobacco-flavored e-liquids were derived from flavoring chemicals (e.g., bubble gum and cotton candy flavoring) rather than tobacco extract.[184] Various candy and fruit flavored e-liquids exhibited cytotoxic or mutagenic effects in vitro.[187]
Formaldehyde
[edit]IARC categorized formaldehyde as a human carcinogen, and acetaldehyde is categorized as a potential human carcinogen.[234] Formaldehyde induced DNA damage and inhibited DNA repair. Acetaldehyde generated DNA crosslinking, which impedes metabolic functions, including DNA replication, repair, recombination, transcription and chromatin remodeling.[249] Aldehydes may cause harm.[234] A 2016 study reported that e-liquids without flavoring generated no aldehydes, which indicated that flavorings were causing the creation of aldehydes, according to a 2018 PHE report.[81]: 160
Chemicals can be inadvertently produced, especially carbonyls such as formaldehyde, acetaldehyde, acrolein, and glyoxal when the nichrome wire (heating element) reaches a high enough temperature.[234][93] Potentially hazardous carbonyls have been identified in aerosols at temperatures above 200 °C.[137] Propylene glycol-containing liquids produced the most amounts of carbonyls.[234] A 2014 study reported toxic chemical vapor levels at 1 to 2 orders of magnitude smaller than with cigarette smoke, but greater than from a nicotine inhaler.[15] A 2015 study reported toxic and irritation-causing carbonyls, although measured levels of toxic chemicals were inconsistent. The study reported that toxicant levels may be higher than with cigarette smoke.[93]
A 2017 study reported that battery output voltage positively influenced carbonyl vapor levels.[234] A 2015 study reported that e-cigarettes using higher voltages (5.0 V)[238] can emit carcinogens including formaldehyde at levels comparable to cigarette smoke,[146] creating a lifetime cancer risk 5 to 15 times greater than long-term smoking.[238] while lower voltages (3.0 V[1]) produce levels of formaldehyde and acetaldehyde roughly 13 and 807-fold less than in cigarette smoke.[234] Elevated aldehyde formation has an unpleasant taste, leading users to avoid it.[106] The average amount of formaldehyde in vapor from high-voltage devices is higher than the average from cigarettes.[250] Another 2015 study reported that "dripping", where the e-liquid is dripped directly onto the atomizer, can create carbonyls.[251]
The amount of formaldehyde expected to be inhaled by the user is disputed.[237] In 2015 PHE reported that normal vaping generates low levels of aldehydes. Normal usage also generates low levels of formaldehyde.[180]: 77, 82 However, users detect and avoid the "dry puff", leading them to conclude, "There is no indication that EC users are exposed to dangerous levels of aldehydes.": 77–78 In 2018 PHE reported that at normal temperatures, aldehyde levels were negligible compared with smoke.[81]: 158
Nicotine
[edit]
Nicotine is classified as a poison,[253][254] and it is "extremely hazardous".[255] However, at doses typically used by consumers, it presents little if any hazard to the user.[256][257][258] A 2018 Cochrane Collaboration review lists nine main adverse events related to nicotine replacement therapy: headache, dizziness, lightheadedness, nausea, vomiting, gastrointestinal symptoms, insomnia, abnormal dreams, non-ischemic palpitations and chest pain, skin reactions, oral/nasal reactions, and hiccups.[259] Many of these were also common in the placebo group without nicotine.[259] Palpitations and chest pain were deemed "rare" and there was no evidence of an increased number of serious cardiac problems compared to the placebo group, even in people with established cardiac disease.[260] The common side effects from nicotine exposure are listed in the table below. Serious adverse events due to the use of nicotine replacement therapy are extremely rare.[260] At low amounts, it has a mild analgesic effect.[261] However, at sufficiently high doses, nicotine may result in nausea, vomiting, diarrhea, salivation, bradycardia, and possibly seizures, hypoventilation, and death.[262]
| Route of administration | Dosage form | Associated side effects of nicotine | Sources |
|---|---|---|---|
| Buccal | Nicotine gum | Indigestion, nausea, hiccups, traumatic injury to oral mucosa or teeth, irritation or tingling of the mouth and throat, oral mucosal ulceration, jaw-muscle ache, burping, gum sticking to teeth, unpleasant taste, dizziness, lightheadedness, headache, and insomnia. | [260][263] |
| Lozenge | Nausea, dyspepsia, flatulence, headache, upper respiratory tract infections, irritation (i.e., a burning sensation), hiccups, sore throat, coughing, dry lips, and oral mucosal ulceration. | [260][263] | |
| Transdermal | Transdermal patch |
Application site reactions (i.e., pruritus, burning, or erythema), diarrhea, dyspepsia, abdominal pain, dry mouth, nausea, dizziness, nervousness or restlessness, headache, vivid dreams or other sleep disturbances, and irritability. | [260][263][264] |
| Intranasal | Nasal spray | Runny nose, nasopharyngeal and ocular irritation, watery eyes, sneezing, and coughing. | [260][263][265] |
| Oral inhalation | Inhaler | Dyspepsia, oropharyngeal irritation (e.g., coughing, irritation of the mouth and throat), rhinitis, and headache. | [260][263][266] |
| All (nonspecific) | Peripheral vasoconstriction, tachycardia (i.e., fast heart rate), elevated blood pressure, increased alertness and cognitive performance. | [263][265] | |
Cigarettes and nicotine replacement products
[edit]E-cigarettes increase serum nicotine levels quicker than nicotine replacement products,[203][13] but more gradually than traditional cigarettes.[267] A 2014 review concluded that e-cigarettes have a pharmacokinetic nicotine profile closer to nicotine replacement products than to traditional cigarettes.[268]
Another 2014 review concluded that serum cotinine levels were comparable to traditional cigarettes,[269] but varied by usage pattern and device.[136]
A 2017 study reported that vaping produced comparable levels of nicotine urinary metabolites to tobacco and smokeless tobacco products.[239] However, oxidative nicotine metabolites were less in vapers.[239]
A 2017 review concluded that some vaping products delivered the same amount of nicotine as traditional cigarettes.[270]
In 2018 the National Academies of Sciences, Engineering, and Medicine reported that the degree of dependence is less for e-cigarettes than traditional cigarettes.[99]: Summary, Conclusion 8-2., 7
Aerosol composition
[edit]The chemical composition of e-cigarette aerosols varies. As of 2014 limited chemistry data existed.[1] E-cigarette aerosol is generated when the e-liquid reaches a temperature of roughly 100–250 °C within a chamber, which causes pyrolysis and possible decomposition of other liquid ingredients.[106] The levels of nicotine, TSNAs, aldehydes, metals, volatile organic compounds (VOCs), flavorings, and tobacco alkaloids in e-cigarette vapors vary greatly.[1] The yield of chemicals reported in the e-cigarette vapor varies depending on, several factors, including the e-liquid contents, puffing rate, and the battery voltage.[122]
E-cigarettes consist of fine and ultrafine particles of particulate matter,[15] in the form of an aerosol.[135][1] The aerosol (mist[142]) produced by an e-cigarette is commonly but inaccurately called vapor.[1] In physics, a vapor is a substance in the gas phase whereas an aerosol is a suspension of tiny particles of liquid, solid or both within a gas.[1] The word "vaping" is not technically accurate when applied to e-cigarettes.[271] The aerosol is made-up of liquid sub-micron particles of condensed vapor; thus, the users of these devices are rather "aerosolizing."[271] This aerosol that is produces looks like cigarette smoke to some extent.[134] After a puff, inhalation of the aerosol travels from the device into the mouth and lungs.[1] The composition of e-liquids varies widely due to the extensive range of nicotine levels and flavoring additives used in these products, which result in a variety of chemical combinations.[137]
A 2014 review concluded that the particles produced from vaping are comparable in particle-size distribution and number of particles to cigarette smoke, with the majority in the ultrafine range.[15] Some e-cigarettes released more particles than cigarette smoke. Fine particles can be chemically intricate and non-uniform. Particle composition and size was mostly unknown. These uncertainties limited the ability to compare e-cigarette vapor and traditional cigarettes.[15] In 2014 WHO reported e-cigarettes release a lower concentration of particles than traditional cigarettes.[6]
Metals
[edit]As of 2014 evidence on the long-term exposure of metals was limited.[11] Metals including nickel,[98] cadmium,[98][272] lead,[211] chromium,[211][15] nickel,[211][15] tin,[93] and silicate[98] have been reported in e-cigarette vapor. The device could contribute small amounts of metals in the liquid and vapor,[251] because their metal parts contact the e-liquid.[11]
A 2014 review concluded that it was unlikely that metal contamination was a serious health risk.[11] A 2018 PHE report stated, "[e-cigarettes] that generate minimal metal emissions should become an industry standard."[81]: 162 In 2014 the American Heart Association referenced low levels of metals in emissions.[211] A 2014 review concluded metal particls from various components of e-cigarettes appeared in vapor, with potential exposures higher than smoke.[93] A 2013 study reported metal particles in the aerosol were at levels 10-50 times less than permitted in inhalation medicines.[12] A 2014 review found no evidence of vapor contamination with metals that would justify a health concern.[198]
A 2016 study reported that metals can be carcinogenic, nephrotoxic, neurotoxic, and hemotoxic.[98] A 2018 study reported that copper nanoparticles can induce mitochondrial and DNA injury in lung fibroblasts.[138] DNA repair can be impeded by vaporized titanium dioxide nanoparticles as demonstrated by single-strand DNA breaks and oxidative stress in the DNA of A549 cells.[273] Heavy metals are correlated with serious health issues.[64] Inhaling lead can induce serious neurologic injury, notably to the growing brains of children.[64]
A 2015 report by the American College of Physicians stated that metals may adversely affect the nervous system.[274] A 2016 review concluded that metals reported in vapor may induce cell damage and initiate inflammatory cytokine such as in human lung fibroblasts.[140] A 2017 review concluded, "E-cigarette aerosols and copper nanoparticles induced mitochondrial ROS production, mitochondrial stress (reduced stability of OxPhos electron transport chain (ETC) complex IV subunit) and DNA fragmentation in lung fibroblasts."[139] A 2013 review concluded that metallic nanoparticles are associated with respiratory distress and disease.[275] A 2017 review linked cadmium to low sperm density.[272]
A 2023 review concluded that the evidence about metals in vapor was not sufficient to create a firm conclusion. It highlighted that prior smoking history was not always appropriately considered in these studies due to long half-life for some metals.[276]
First-generation devices
[edit]Compared to traditional cigarettes, older devices typically produced much lower blood nicotine levels,[236][13] although a 2014 study reported plasma nicotine concentration which comparable to that of traditional cigarettes.[163] A 2014 study reported that nicotine delivered from e-cigarettes entered the body slower than traditional cigarettes.[181] A 2014 review concluded that inexperienced users obtained moderate amounts of nicotine from e-cigarettes.[277]
Tank/adjustable devices
[edit]Tank or adjustable e-cigarettes, as well as concentrated nicotine liquids, may deliver nicotine at levels similar to traditional cigarettes.[236][13][92] The American Heart Association reported in 2014 that some e-cigarette tank devices with stronger batteries achieve higher temperatures, which may raise nicotine levels.[211] A 2017 study reported that nicotine delivery compared to previous generation had increased by 35-72%,[102] elevating heart rates comparable to traditional cigarettes.[278] As of 2017 fourth-generation devices had not been heavily researched.[85]
Concerns
[edit]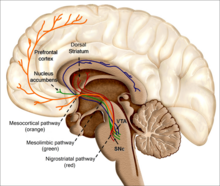
The health effects of long-term nicotine use are unknown.[179] While myriad studies have been conducted, many questions remain unresolved, including impurities in e-liquids,[99]: Minor Tobacco Alkaloids, 193 effects of nicotine,[221][281]
Youth concerns
[edit]Exposure to e-cigarette components in a susceptible time period of brain development could induce persistent behavioral changes.[229] The FDA stated in 2019 that some vapers experienced seizures; most reports involved youth or young adult users.[129]
Toxicant comparisons
[edit]E-cigarettes supply nicotine and other toxins at rates far below traditional cigarettes and other nicotine delivery systems:[238]
| Toxicant | Nicotine inhaler mist (15 puffs∗) | E-cigarettes (15 puffs∗) | 1 cigarette |
|---|---|---|---|
| Formaldehyde (μg) | 0.2 | 0.2-5.61 | 1.6-52 |
| Acetaldehyde (μg) | 0.11 | 0.11-1.36 | 52-140 |
| Acrolein (μg) | ND | 0.07-4.19 | 2.4-62 |
| o-Methylbenzaldehyde (μg) | 0.07 | 0.13-0.71 | — |
| Toluene (μg) | ND | ND-0.63 | 8.3-70 |
| p- and m-Xylene (μg) | ND | ND-0.2 | — |
| NNN (ng) | ND | ND-0.00043 | 0.0005-0.19 |
| Cadmium (ng) | 0.003 | ND-0.022 | — |
| Nickel (ng) | 0.019 | 0.011-0.029 | — |
| Lead (ng) | 0.004 | 0.003-0.057 | — |
Pregnancy/Lactation
[edit]A 2016 review concluded that pregnant and breastfeeding females should substitute cigarettes with e-cigarettes due to the uncertainty about ingredients.[64] Currently, the FDA has not approved e-cigarettes as a smoking cessation aid which is why they discourage use in those pregnant with a developing fetus.[283] e-cigarettes containing chemicals, flavorings, additives, and nicotine can cause permanent, long-term effects on the developing brain of a baby.[284] Because e-cigarettes are unregulated, often the amount of nicotine is not standardized so it is possible that there are higher amounts of nicotine with e-cigarettes compared to traditional cigarettes.[284] One study comparing irritability infants between those exposed to e-cigarettes during pregnancy versus those not exposed to any maternal smoking reported increased irritability among infants in the exposed group.[284]
Currently, it is unclear what impact electronic cigarette use can have on breastfeeding, but it is not recommended to use. Some studies confirm that nicotine is able to transfer into breast milk and can lead to spikes in heart rate and blood pressure for infants drinking nicotine concentrated milk.[284]
Regardless of which stage of pregnancy one is at, the recommendation is to quit smoking cigarettes altogether through smoking cessation therapy rather than turning to e-cigarettes as an alternative.[285] The current recommendation by the U.S. Preventive Services Task Force (USPSTF) for pregnant persons is to seek medical advice from clinicians and use behavioral interventions for cessation.[286] There are many resources and treatments available to help anyone looking to quit e-cigarettes and tobacco cigarettes during pregnancy. Some of these include talking with a healthcare provider team, and utilizing the 1-800-QUIT-NOW (1-800-784-8669) quitline that has resources for those needing advice, support, and referrals.[284]
Public Perceptions
[edit]Marketing and advertisement play a significant role in the public's perception of e-cigarettes.[179] Some tobacco users think vaping is safer than tobacco or other smoking cessation aids.[287] It is generally considered by users that e-cigarettes are safer than tobacco.[288] Emerging research indicates that vaping is not as safe as previously thought.[289] Many users think that e-cigarettes are healthier than traditional cigarettes for personal use or for other people.[207] Many youth believe vaping is a safe substitute to traditional cigarettes.[208] For this reason, e-cigarettes have been thought to negate years of progress in preventing tobacco usage as a whole.[290] A 2016 review suggests "that the perceived health risks, specific product characteristics (such as taste, price and inconspicuous use), and higher levels of acceptance among peers and others potentially make e-cigarettes initially more attractive to adolescents than tobacco cigarettes.[291] Further, there has been a "nonlinear increase" in the use of e-cigarettes from 1.5 to 11.3% within a 6-year time period (2011–2017) among the high school demographic.[290] Youths who have lower harm perceptions may be particularly susceptible to e-cigarette and polytobacco use, conversely those who perceive e-cigarettes as more harmful would be less likely to use them.[292] Usually, only a small proportion of users are concerned about the potential adverse health effects or toxicity of e-cigarettes.[207] A nation-wide US survey among adults reported 11.1% thought vaping during pregnancy was not as harmful as smoking, 51.0% thought it was as harmful, 11.6% thought it would be an increased harm, and 26.2% were unsure.[81]: 190 A 2015 study showed that 60% of all adolescence stated vaping were safe or a minor health risk and that 53.4% considered vaping safer than cigarette smoking.[72] A 2017 review concluded, based on literature from January 2006 to October 2016, examining perceptions regarding vaping during pregnancy, that the majority of respondents perceived vaping can carry health risks to mother and child, but also thought they may be less harmful than traditional cigarettes.[293] Many adolescent asthmatics have a favorable view of vaping.[137] A 2016 survey of people 14 years of age and up in Germany reported that 20.7% of participants consider e-cigarettes to be not as harmful as cigarettes, 46.3% just as harmful, and 16.1% thought they were more harmful, and 17.0% gave no answer.[81]: 189 In terms of harm perception, a 2016 study reported that flavored vaping reduced the prevalence of perception of the dangers of tobacco use among youth.[240] Another 2016 study reported more nuanced results, demonstrating that tobacco flavoring increased harm perception while fruit and sweet flavors decreased harm perception among UK adolescents.[240] Similarly, a 2016 study in the US reported that, for US adolescents, fruit-flavored e-cigarettes were perceived to be less harmful than tobacco flavored ones.[240] There is indication that an individual's perception of a substance's potential harms and benefits and their behavior of use is influenced by the availability of information discussing the health effects of that substance.[294] A 2015 analysis reports that 34.20% (8433/24,658) of American youth sampled believe that e-cigarettes are less harmful than cigarettes, and 45% (11,096/24,658) are not sure.[294]
As of 2018[update], under 50% of adults in the UK believe vaping is less harmful than smoking.[81]: 20 Action on Smoking and Health (ASH) in the UK reported that in 2015, compared to the year before, "there has been a growing false belief that e-cigarettes could be as harmful as smoking".[295] Among smokers who had heard of e-cigarettes but never tried them, this "perception of harm has nearly doubled from 12% in 2014 to 22% in 2015."[295] ASH expressed concern that "The growth of this false perception risks discouraging many smokers from using e-cigarettes to quit and keep them smoking instead which would be bad for their health and the health of those around them."[295] A 2015 PHE report noted that in the US belief among respondents to a survey that vaping was safer than smoking cigarettes fell from 82% in 2010 to 51% in 2014.[81]: 79 The report blamed "misinterpreted research findings", attracting negative media coverage, for the growth in the "inaccurate" belief that e-cigarettes were as harmful as smoking.[81]: 6, 11, 79–80 A 2017 review noted that there is a public misconception that vaping is safer than cigarette smoking.[296] A 2016 review noted that the increasing use of e-cigarettes may be due in part to "the misperception that e-cigarettes are a safer alternative to traditional cigarettes."[297] A 2014 review noted that "users do not appear to fully understand their health risks."[268] Beliefs on vaping may be surpassing our scientific knowledge of these products.[298] Proponents of vaping have stated that nicotine is 'as safe as caffeine'.[299] E-cigarettes are believed to be considerably safer compared with smoking and nicotine is thought to be comparatively harmless.[300] As a consequence, it is believed to be without risk to use them indoors or near babies.[300]
A 2014 worldwide survey reported that 88% of respondents stated that vaping were less harmful than cigarette smoke and 11% believed that vaping were absolutely harmless.[301] A 2013 four-country survey reported higher than 75% of current and former smokers think e-cigarettes are safer than traditional cigarettes.[92] A 2017 study reported that among high income countries, Republic of Korea in 2016 was 66%, the US in 2016 was 37%, Netherlands in 2015 was 32%, Canada in 2016 was 30%, the UK in 2016 was 24%, Australia in 2016 was 22%, Uruguay in 2014 was 19%, and among low income countries, Malaysia in 2013 was 70%, Zambia in 2014 was 57%, Thailand in 2012 was 54%, Mexico from 2014 to 2015 was 38%, Bangladesh from 2014 to 2015 was 37%, Brazil from 2012 to 2013 was 22%, and China from 2013 to 2015 was 15%, for the percentage of respondents of adult smokers believing vaping is just as risky or more risky to health than cigarettes.[81]: 188
A 2016 review concluded that "The vaping communities' apparent lack of acknowledgment of the potential negative impacts of e-cigarettes appears to have discredited them in the eyes of many public health officials. Continuing down this path may generate beliefs that the vaping community cares little for public health, are primarily interested in selling their fast-growing companies to the highest tobacco company bidder, and will oppose any meaningful regulations of their product, however reasonable and necessary they may be—essentially aligning the vaping community's practices to tobacco companies' well-established playbook."[302] A 2017 review concluded that "Although it was originally argued that e‐cigarettes are 'harm free,' the present prevailing belief is that they are 'reduced harm' alternatives to conventional cigarettes. This latter notion is still debatable and not supported by conclusive evidence, especially considering the wide variation between e‐cigarette products."[102] E-cigarette advertisements with warnings could strengthen e-cigarette harm perceptions, and lower the likelihood of buying e-cigarettes.[303]
Overall, e-cigarettes were originally intended to be used as a way to reduce harm and quit smoking in relation to other tobacco products already on the market. Over time, the product became increasingly popular in the youth of the United States due to marketing, accessibility, e-liquid flavorings, amount of delivered tobacco products, and lack of information regarding the effects on health.[304]
The use of e-cigarettes in youth (Middle School and High School) of the United States remains the most commonly used type of device containing tobacco by a significant margin as of the 2023 National Youth Tobacco Survey. While trends have shown a decrease in electronic cigarette use in high school students and an increase in electronic cigarette use in middle school students, it is estimated that about 2.8 million youth currently use any tobacco product.[305] It is thought that youths who were more exposed to negative news about e-cigarettes influenced their beliefs towards harmfulness of them. Other things to take into consideration include: increased vulnerability of youth to marketing, social influence and peer pressure as a way for them to be more incorporated in their communities. As public knowledge about effects of e-cigarettes increase along with their studies, it is thought to contribute to lowering the usage of e-cigarettes.[304]
The largest age group contributing to the use and purchase of e-cigarettes are young adults, which include an age range from teens to 30's. A questionnaire examining college students demonstrated that current users believe that e-cigarettes are more convenient and taste and smell better than traditional tobacco products. Another notable result was the trend among current electronic cigarette users to have reported no previous use of tobacco. This would be contraindicative of what the original claims of e-cigarettes manufacturers when they were introduced to the market. While a majority of electronic cigarette users state the understanding of possible harm to their health, there is also the belief that they are safer than other forms of tobacco.[306]
Gallery
[edit]- Images of E-cigarette battery explosion injuries
See also
[edit]- Health effects of tobacco
- Regulation of e-cigarettes
- Positions of medical organizations on e-cigarettes
Notes
[edit]- ^ Also known as an e-cig, vaporizer, vape pen, hookah pen, e-pipe, or, formally, electronic nicotine delivery system (ENDS).[16]
- ^ A 2014 review found "In addition to the uniqueness of the liquid compositions in each brand, inconsistency of both the device performance properties and the data collection methodologies used by researchers contribute to the observed variation in constituent levels and to the range of particle size distributions among products."[17]
- ^ "Most ENDS consist of a rechargeable, battery-operated heating element and a replaceable or refillable cartridge for the e-liquid. An atomizer heats the liquid in the cartridge to convert it into an aerosol, which is then inhaled by the user. Most of these products are rechargeable, but some are disposable."[23]
References
[edit]- ^ a b c d e f g h i j Cheng T (May 2014). "Chemical evaluation of electronic cigarettes". Tobacco Control. 23 (Supplement 2): ii11 – ii17. doi:10.1136/tobaccocontrol-2013-051482. PMC 3995255. PMID 24732157.
- ^ MacDonald M, O'Leary R, Stockwell T, Reist D (May 2016). "Clearing the air: protocol for a systematic meta-narrative review on the harms and benefits of e-cigarettes and vapour devices". Systematic Reviews. 5 (1): 85. doi:10.1186/s13643-016-0264-y. PMC 4875675. PMID 27209032.
 This article incorporates text by Marjorie MacDonald, Renee O'Leary, Tim Stockwell, and Dan Reist available under the CC BY 4.0 license.
This article incorporates text by Marjorie MacDonald, Renee O'Leary, Tim Stockwell, and Dan Reist available under the CC BY 4.0 license.
- ^ a b c "Electronic Cigarettes". Centers for Disease Control and Prevention. 7 September 2017.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ "E-cigarettes around 95% less harmful than tobacco estimates landmark review". GOV.UK. Retrieved 2021-02-27.
- ^ Brady BR, De La Rosa JS, Nair US, Leischow SJ (January 2019). "Electronic Cigarette Policy Recommendations: A Scoping Review". American Journal of Health Behavior. 43 (1): 88–104. doi:10.5993/AJHB.43.1.8. PMID 30522569. S2CID 54566712.
- ^ a b c d "Electronic nicotine delivery systems" (PDF). World Health Organization. 21 July 2014. pp. 1–13.
- ^ a b Breland A, Soule E, Lopez A, Ramôa C, El-Hellani A, Eissenberg T (April 2017). "Electronic cigarettes: what are they and what do they do?". Annals of the New York Academy of Sciences. 1394 (1): 5–30. Bibcode:2017NYASA1394....5B. doi:10.1111/nyas.12977. PMC 4947026. PMID 26774031.
- ^ Darabseh MZ, Selfe J, Morse CI, Degens H (January 2020). "Is vaping better than smoking for cardiorespiratory and muscle function?". Multidisciplinary Respiratory Medicine. 15 (1): 674. doi:10.4081/mrm.2020.674 (inactive 2024-11-02). PMC 7348661. PMID 32670575.
{{cite journal}}: CS1 maint: DOI inactive as of November 2024 (link) - ^ Münzel T, Hahad O, Kuntic M, Keaney JF, Deanfield JE, Daiber A (November 2020). "Effects of tobacco cigarettes, e-cigarettes, and waterpipe smoking on endothelial function and clinical outcomes". European Heart Journal. 41 (41): 4057–4070. doi:10.1093/eurheartj/ehaa460. PMC 7454514. PMID 32585699.
- ^ CDC's Office on Smoking and Health (2020-11-27). "Smoking and Tobacco Use; Electronic Cigarettes". Centers for Disease Control and Prevention. Retrieved 2021-05-10.
- ^ a b c d e f g h i j k Farsalinos KE, Polosa R (April 2014). "Safety evaluation and risk assessment of electronic cigarettes as tobacco cigarette substitutes: a systematic review". Therapeutic Advances in Drug Safety. 5 (2): 67–86. doi:10.1177/2042098614524430. PMC 4110871. PMID 25083263.
- ^ a b c d e f g h i j k l Hajek P, Etter JF, Benowitz N, Eissenberg T, McRobbie H (November 2014). "Electronic cigarettes: review of use, content, safety, effects on smokers and potential for harm and benefit". Addiction. 109 (11): 1801–1810. doi:10.1111/add.12659. PMC 4487785. PMID 25078252.
- ^ a b c d e f g h Brandon TH, Goniewicz ML, Hanna NH, Hatsukami DK, Herbst RS, Hobin JA, et al. (February 2015). "Electronic nicotine delivery systems: a policy statement from the American Association for Cancer Research and the American Society of Clinical Oncology". Clinical Cancer Research. 21 (3): 514–525. doi:10.1158/1078-0432.CCR-14-2544. PMID 25573384.
- ^ a b Durmowicz EL (May 2014). "The impact of electronic cigarettes on the paediatric population". Tobacco Control. 23 (Supplement 2): ii41 – ii46. doi:10.1136/tobaccocontrol-2013-051468. PMC 3995262. PMID 24732163.
- ^ a b c d e f g h i j k l m n o p Grana R, Benowitz N, Glantz SA (May 2014). "E-cigarettes: a scientific review". Circulation. 129 (19): 1972–1986. doi:10.1161/circulationaha.114.007667. PMC 4018182. PMID 24821826.
- ^ a b "Vaporizers, E-Cigarettes, and other Electronic Nicotine Delivery Systems (ENDS)". United States Food and Drug Administration. 14 February 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ a b Cheng T (2014). "Chemical evaluation of electronic cigarettes". Tobacco Control. 23 (Supplement 2): ii11 – ii17. doi:10.1136/tobaccocontrol-2013-051482. ISSN 0964-4563. PMC 3995255. PMID 24732157.
- ^ a b c Orellana-Barrios MA, Payne D, Mulkey Z, Nugent K (2015). "Electronic cigarettes-a narrative review for clinicians". The American Journal of Medicine. 128 (7): 674–81. doi:10.1016/j.amjmed.2015.01.033. ISSN 0002-9343. PMID 25731134.
- ^ Weaver M, Breland A, Spindle T, Eissenberg T (2014). "Electronic Cigarettes". Journal of Addiction Medicine. 8 (4): 234–240. doi:10.1097/ADM.0000000000000043. ISSN 1932-0620. PMC 4123220. PMID 25089953.
- ^ David G, Parmentier EA, Taurino I, Signorell R (December 2020). "Tracing the composition of single e-cigarette aerosol droplets in situ by laser-trapping and Raman scattering". Scientific Reports. 10 (1): 7929. Bibcode:2020NatSR..10.7929D. doi:10.1038/s41598-020-64886-5. PMC 7220912. PMID 32404884.
- ^ Rahman M, Hann N, Wilson A, Worrall-Carter L (2014). "Electronic cigarettes: patterns of use, health effects, use in smoking cessation and regulatory issues". Tobacco Induced Diseases. 12 (1): 21. doi:10.1186/1617-9625-12-21. PMC 4350653. PMID 25745382.
- ^ Pepper JK, Brewer NT (2013). "Electronic nicotine delivery system (electronic cigarette) awareness, use, reactions and beliefs: a systematic review". Tobacco Control. 23 (5): 375–384. doi:10.1136/tobaccocontrol-2013-051122. ISSN 0964-4563. PMC 4520227. PMID 24259045.
- ^ Drope J, Cahn Z, Kennedy R, Liber AC, Stoklosa M, Henson R, et al. (November 2017). "Key issues surrounding the health impacts of electronic nicotine delivery systems (ENDS) and other sources of nicotine". CA: A Cancer Journal for Clinicians. 67 (6): 449–471. doi:10.3322/caac.21413. ISSN 0007-9235. PMID 28961314. S2CID 32928770.
- ^ Bekki K, Uchiyama S, Ohta K, Inaba Y, Nakagome H, Kunugita N (2014). "Carbonyl Compounds Generated from Electronic Cigarettes". International Journal of Environmental Research and Public Health. 11 (11): 11192–11200. doi:10.3390/ijerph111111192. ISSN 1660-4601. PMC 4245608. PMID 25353061.
- ^ Nansseu JR, Bigna JJ (2016). "Electronic Cigarettes for Curbing the Tobacco-Induced Burden of Noncommunicable Diseases: Evidence Revisited with Emphasis on Challenges in Sub-Saharan Africa". Pulmonary Medicine. 2016: 1–9. doi:10.1155/2016/4894352. ISSN 2090-1836. PMC 5220510. PMID 28116156.
 This article incorporates text by Jobert Richie N. Nansseu and Jean Joel R. Bigna available under the CC BY 4.0 license.
This article incorporates text by Jobert Richie N. Nansseu and Jean Joel R. Bigna available under the CC BY 4.0 license.
- ^ a b c Bhatnagar A, Whitsel LP, Ribisl KM, Bullen C, Chaloupka F, Piano MR, et al. (2014). "Electronic Cigarettes: A Policy Statement From the American Heart Association" (PDF). Circulation. 130 (16): 1418–1436. doi:10.1161/CIR.0000000000000107. ISSN 0009-7322. PMC 7643636. PMID 25156991. S2CID 16075813.
- ^ Caponnetto P, Russo C, Bruno C, Alamo A, Amaradio M, Polosa R (March 2013). "Electronic cigarette: a possible substitute for cigarette dependence". Monaldi Archives for Chest Disease. 79 (1): 12–19. doi:10.4081/monaldi.2013.104. ISSN 1122-0643. PMID 23741941.
- ^ Jimenez Ruiz CA, Solano Reina S, de Granda Orive JI, Signes-Costa Minaya J, de Higes Martinez E, Riesco Miranda JA, et al. (August 2014). "The electronic cigarette. Official statement of the Spanish Society of Pneumology and Thoracic Surgery (SEPAR) on the efficacy, safety and regulation of electronic cigarettes". Archivos de Bronconeumologia. 50 (8): 362–7. doi:10.1016/j.arbres.2014.02.006. PMID 24684764.
- ^ a b c Schick SF, Blount BC, Jacob P, Saliba NA, Bernert JT, El Hellani A, et al. (2017). "Biomarkers of Exposure to New and Emerging Tobacco and Nicotine Delivery Products". American Journal of Physiology. Lung Cellular and Molecular Physiology. 313 (3): L425 – L452. doi:10.1152/ajplung.00343.2016. ISSN 1040-0605. PMC 5626373. PMID 28522563.
- ^ Clapp PW, Jaspers I (2017). "Electronic Cigarettes: Their Constituents and Potential Links to Asthma". Current Allergy and Asthma Reports. 17 (11): 79. doi:10.1007/s11882-017-0747-5. ISSN 1529-7322. PMC 5995565. PMID 28983782.
- ^ Naskar S, Jakati P (2017). ""Vaping:" Emergence of a new paraphernalia". Indian Journal of Psychological Medicine. 39 (5): 566–572. doi:10.4103/IJPSYM.IJPSYM_142_17. ISSN 0253-7176. PMC 5688881. PMID 29200550.
- ^ Stratton 2018, p. Other Toxicants, Caffeine; 197.
- ^ a b c Staal YC, van de Nobelen S, Havermans A, Talhout R (2018). "New Tobacco and Tobacco-Related Products: Early Detection of Product Development, Marketing Strategies, and Consumer Interest". JMIR Public Health and Surveillance. 4 (2): e55. doi:10.2196/publichealth.7359. ISSN 2369-2960. PMC 5996176. PMID 29807884.
 This article incorporates text by Yvonne CM Staal, Suzanne van de Nobelen, Anne Havermans, and Reinskje Talhout available under the CC BY 4.0 license.
This article incorporates text by Yvonne CM Staal, Suzanne van de Nobelen, Anne Havermans, and Reinskje Talhout available under the CC BY 4.0 license.
- ^ Lynne Dawkins, John Turner, Amanda Roberts, Kirstie Soar (2013). "Vaping' profiles and preferences: an online survey of electronic cigarette users" (PDF). School of Psychology-University of East London.
- ^ Wilder N, Daley C, Sugarman J, Partridge J (April 2016). "Nicotine without smoke: Tobacco harm reduction". UK: Royal College of Physicians. p. 82.
- ^ Leduc C, Quoix E (2016). "Is there a role for e-cigarettes in smoking cessation?". Therapeutic Advances in Respiratory Disease. 10 (2): 130–135. doi:10.1177/1753465815621233. ISSN 1753-4658. PMC 5933562. PMID 26668136.
- ^ Oh AY, Kacker A (December 2014). "Do electronic cigarettes impart a lower potential disease burden than conventional tobacco cigarettes?: Review on e-cigarette vapor versus tobacco smoke". The Laryngoscope. 124 (12): 2702–2706. doi:10.1002/lary.24750. PMID 25302452. S2CID 10560264.
- ^ Giroud C, de Cesare M, Berthet A, Varlet V, Concha-Lozano N, Favrat B (2015). "E-Cigarettes: A Review of New Trends in Cannabis Use". International Journal of Environmental Research and Public Health. 12 (8): 9988–10008. doi:10.3390/ijerph120809988. ISSN 1660-4601. PMC 4555324. PMID 26308021.
- ^ Xiaolong Zheng, Daniel Dajun Zeng, Hsinchun Chen, Scott J. Leischow (22 January 2016). Smart Health: International Conference, ICSH 2015, Phoenix, AZ, USA, November 17-18, 2015. Revised Selected Papers. Springer. pp. 279–. ISBN 978-3-319-29175-8.
- ^ DeVito EE, Krishnan-Sarin S (2018). "E-cigarettes: Impact of E-Liquid Components and Device Characteristics on Nicotine Exposure". Current Neuropharmacology. 16 (4): 438–459. doi:10.2174/1570159X15666171016164430. ISSN 1570-159X. PMC 6018193. PMID 29046158.
- ^ Chang H (2014). "Research gaps related to the environmental impacts of electronic cigarettes". Tobacco Control. 23 (Supplement 2): ii54 – ii58. doi:10.1136/tobaccocontrol-2013-051480. ISSN 0964-4563. PMC 3995274. PMID 24732165.
- ^ Burstyn I (9 January 2014). "Peering through the mist: systematic review of what the chemistry of contaminants in electronic cigarettes tells us about health risks". BMC Public Health. 14: 18. doi:10.1186/1471-2458-14-18. PMC 3937158. PMID 24406205.
- ^ Brandon TH, Goniewicz ML, Hanna NH, Hatsukami DK, Herbst RS, Hobin JA, et al. (2015). "Electronic Nicotine Delivery Systems: A Policy Statement from the American Association for Cancer Research and the American Society of Clinical Oncology". Clinical Cancer Research. 21 (3): 514–525. doi:10.1158/1078-0432.CCR-14-2544. ISSN 1078-0432. PMID 25573384.
- ^ Tomashefski A (2016). "The perceived effects of electronic cigarettes on health by adult users: A state of the science systematic literature review". Journal of the American Association of Nurse Practitioners. 28 (9): 510–5. doi:10.1002/2327-6924.12358. ISSN 2327-6886. PMID 26997487. S2CID 42900184.
- ^ Chun LF, Moazed F, Calfee CS, Matthay MA, Gotts JE (2017). "Pulmonary Toxicity of E-cigarettes". American Journal of Physiology. Lung Cellular and Molecular Physiology. 313 (2): L193 – L206. doi:10.1152/ajplung.00071.2017. ISSN 1040-0605. PMC 5582932. PMID 28522559.
- ^ Thirión-Romero I, Pérez-Padilla R, Zabert G, Barrientos-Gutiérrez I (2019). "Respiratory Impact of Electronic Cigarettes and Low-Risk Tobacco". Revista de investigación Clínica. 71 (1): 17–27. doi:10.24875/RIC.18002616. ISSN 0034-8376. PMID 30810544. S2CID 73511138.
- ^ a b Weaver M, Breland A, Spindle T, Eissenberg T (2014). "Electronic Cigarettes". Journal of Addiction Medicine. 8 (4): 234–240. doi:10.1097/ADM.0000000000000043. ISSN 1932-0620. PMC 4123220. PMID 25089953.
- ^ a b c Hajek P, Etter JF, Benowitz N, Eissenberg T, McRobbie H (31 July 2014). "Electronic cigarettes: review of use, content, safety, effects on smokers and potential for harm and benefit". Addiction. 109 (11): 1801–10. doi:10.1111/add.12659. PMC 4487785. PMID 25078252.
- ^ a b Jerry JM, Collins GB, Streem D (2015). "E-cigarettes: Safe to recommend to patients?". Cleve Clin J Med. 82 (8): 521–6. doi:10.3949/ccjm.82a.14054. PMID 26270431.
- ^ Naik P, Cucullo L (2015). "Pathobiology of tobacco smoking and neurovascular disorders: untied strings and alternative products". Fluids and Barriers of the CNS. 12 (1): 25. doi:10.1186/s12987-015-0022-x. ISSN 2045-8118. PMC 4628383. PMID 26520792.
- ^ Breland AB, Spindle T, Weaver M, Eissenberg T (2014). "Science and Electronic Cigarettes". Journal of Addiction Medicine. 8 (4): 223–233. doi:10.1097/ADM.0000000000000049. ISSN 1932-0620. PMC 4122311. PMID 25089952.
- ^ Zulkifli A, Abidin EZ, Abidin NZ, Amer Nordin AS, Praveena SM, Syed Ismail SN, et al. (2016). "Electronic cigarettes: a systematic review of available studies on health risk assessment" (PDF). Reviews on Environmental Health. 33 (1): 43–52. doi:10.1515/reveh-2015-0075. ISSN 2191-0308. PMID 27101543. S2CID 3702954.
- ^ a b Palazzolo DL (November 2013). "Electronic cigarettes and vaping: a new challenge in clinical medicine and public health. A literature review". Frontiers in Public Health. 1 (56): 56. doi:10.3389/fpubh.2013.00056. PMC 3859972. PMID 24350225.
 This article incorporates text by Dominic L. Palazzolo available under the CC BY 3.0 license.
This article incorporates text by Dominic L. Palazzolo available under the CC BY 3.0 license.
- ^ Jenssen BP, Wilson KM (2017). "Tobacco Control and Treatment for the Pediatric Clinician: Practice, Policy, and Research Updates". Academic Pediatrics. 17 (3): 233–242. doi:10.1016/j.acap.2016.12.010. ISSN 1876-2859. PMID 28069410.
- ^ Bertholon J, Becquemin M, Annesi-Maesano I, Dautzenberg B (2013). "Electronic Cigarettes: A Short Review". Respiration. 86 (5): 433–8. doi:10.1159/000353253. ISSN 1423-0356. PMID 24080743.
- ^ a b c Dinakar C, Longo DL, O'Connor GT (2016). "The Health Effects of Electronic Cigarettes". New England Journal of Medicine. 375 (14): 1372–1381. doi:10.1056/NEJMra1502466. ISSN 0028-4793. PMID 27705269.
- ^ Orr MS (2014). "Electronic cigarettes in the USA: a summary of available toxicology data and suggestions for the future: Table 1". Tobacco Control. 23 (suppl 2): ii18 – ii22. doi:10.1136/tobaccocontrol-2013-051474. ISSN 0964-4563. PMC 3995288. PMID 24732158.
- ^ a b Varlet V, Farsalinos K, Augsburger M, Thomas A, Etter JF (2015). "Toxicity Assessment of Refill Liquids for Electronic Cigarettes". International Journal of Environmental Research and Public Health. 12 (5): 4796–4815. doi:10.3390/ijerph120504796. ISSN 1660-4601. PMC 4454939. PMID 25941845.
- ^ Famele M, Ferranti C, Abenavoli C, Palleschi L, Mancinelli R, Draisci R (2014). "The Chemical Components of Electronic Cigarette Cartridges and Refill Fluids: Review of Analytical Methods". Nicotine & Tobacco Research. 17 (3): 271–279. doi:10.1093/ntr/ntu197. ISSN 1462-2203. PMC 5479507. PMID 25257980.
- ^ Stratton 2018, p. Other Toxicants, Phthalates; 196.
- ^ "RCP statement on e-cigarettes". Royal College of Physicians. 25 June 2014.
- ^ "Nicotine products can help people to cut down before quitting smoking". National Institute for Health and Care Excellence. June 2013. Archived from the original on 2015-11-19. Retrieved 2015-02-24.
- ^ "What about electronic cigarettes? Aren't they safe?". American Cancer Society. Archived from the original on 2014-09-23. Retrieved 2015-02-24.
- ^ a b c d Smith L, Brar K, Srinivasan K, Enja M, Lippmann S (June 2016). "E-cigarettes: How "safe" are they?". The Journal of Family Practice. 65 (6): 380–385. PMID 27474819.
- ^ a b c Oh AY, Kacker A (December 2014). "Do electronic cigarettes impart a lower potential disease burden than conventional tobacco cigarettes? Review on E-cigarette vapor versus tobacco smoke". The Laryngoscope. 124 (12): 2702–2706. doi:10.1002/lary.24750. PMID 25302452. S2CID 10560264.
- ^ a b Palazzolo DL (November 2013). "Electronic cigarettes and vaping: a new challenge in clinical medicine and public health. A literature review". Frontiers in Public Health. 1 (56): 56. doi:10.3389/fpubh.2013.00056. PMC 3859972. PMID 24350225.
 This article incorporates text by Dominic L. Palazzolo available under the CC BY 3.0 license.
This article incorporates text by Dominic L. Palazzolo available under the CC BY 3.0 license.
- ^ Kalkhoran S, Glantz SA (February 2016). "E-cigarettes and smoking cessation in real-world and clinical settings: a systematic review and meta-analysis". The Lancet. Respiratory Medicine. 4 (2): 116–128. doi:10.1016/S2213-2600(15)00521-4. PMC 4752870. PMID 26776875.
- ^ CDC (2024-05-28). "Health Effects of Vaping". Smoking and Tobacco Use. Retrieved 2025-01-03.
- ^ "Regulation of Electronic Cigarettes ("E-Cigarettes")" (PDF). National Association of County and City Health Officials. Archived from the original (PDF) on 6 November 2014.
- ^ Banks E, Yazidjoglou A, Brown S, Nguyen M, Martin M, Beckwith K, et al. (2022). "Electronic cigarettes and health outcomes: systematic review of global evidence". ANU Research Publications- Open Research Repository. doi:10.25911/XV0F-6C42.
- ^ Smith N (20 January 2016). "Headlines about e-cigarettes don't mean they're 'not safer than tobacco'". Cancer Research UK. Archived from the original on 14 February 2019. Retrieved 13 February 2019.
- ^ a b Greenhill R, Dawkins L, Notley C, Finn MD, Turner JJ (December 2016). "Adolescent Awareness and Use of Electronic Cigarettes: A Review of Emerging Trends and Findings". The Journal of Adolescent Health. 59 (6): 612–619. doi:10.1016/j.jadohealth.2016.08.005. PMID 27693128.
- ^ a b Schraufnagel DE (March 2015). "Electronic Cigarettes: Vulnerability of Youth". Pediatric Allergy, Immunology, and Pulmonology. 28 (1): 2–6. doi:10.1089/ped.2015.0490. PMC 4359356. PMID 25830075.
- ^ a b c d Nansseu JR, Bigna JJ (2016). "Electronic Cigarettes for Curbing the Tobacco-Induced Burden of Noncommunicable Diseases: Evidence Revisited with Emphasis on Challenges in Sub-Saharan Africa". Pulmonary Medicine. 2016: 4894352. doi:10.1155/2016/4894352. PMC 5220510. PMID 28116156.
 This article incorporates text by Jobert Richie N. Nansseu and Jean Joel R. Bigna available under the CC BY 4.0 license.
This article incorporates text by Jobert Richie N. Nansseu and Jean Joel R. Bigna available under the CC BY 4.0 license.
- ^ Jankowski M, Krzystanek M, Zejda JE, Majek P, Lubanski J, Lawson JA, et al. (June 2019). "E-Cigarettes are More Addictive than Traditional Cigarettes-A Study in Highly Educated Young People". International Journal of Environmental Research and Public Health. 16 (13): 2279. doi:10.3390/ijerph16132279. PMC 6651627. PMID 31252671.
- ^ a b c "Electronic Cigarettes – An Overview" (PDF). German Cancer Research Center. 2013.
- ^ a b Sanford Z, Goebel L (2014). "E-cigarettes: an up to date review and discussion of the controversy". The West Virginia Medical Journal. 110 (4): 10–15. PMID 25322582.
- ^ Smith L, Brar K, Srinivasan K, Enja M, Lippmann S (June 2016). "E-cigarettes: How "safe" are they?". The Journal of Family Practice. 65 (6): 380–385. PMID 27474819.
- ^ Hartmann-Boyce J, Lindson N, Butler AR, McRobbie H, Bullen C, Begh R, et al. (November 2022). "Electronic cigarettes for smoking cessation". The Cochrane Database of Systematic Reviews. 11 (11): CD010216. doi:10.1002/14651858.CD010216.pub7. PMC 9668543. PMID 36384212.
- ^ Lødrup Carlsen KC, Skjerven HO, Carlsen KH (September 2018). "The toxicity of E-cigarettes and children's respiratory health". Paediatric Respiratory Reviews. 28: 63–67. doi:10.1016/j.prrv.2018.01.002. PMID 29580719. S2CID 4368058.
- ^ a b c d e f g h i j k l m n o p q r s t u v w McNeill A, Brose LS, Calder R, Hitchman SC, Hajek P, McRobbie H (August 2015). "E-cigarettes: an evidence update" (PDF). UK: Public Health England. pp. 1–113.
- ^ a b c d e f g h i j k l m n o p Glantz SA, Bareham DW (April 2018). "E-Cigarettes: Use, Effects on Smoking, Risks, and Policy Implications". Annual Review of Public Health. 39 (1): 215–235. doi:10.1146/annurev-publhealth-040617-013757. PMC 6251310. PMID 29323609.
 This article incorporates text by Stanton A. Glantz and David W. Bareham available under the CC BY 4.0 license.
This article incorporates text by Stanton A. Glantz and David W. Bareham available under the CC BY 4.0 license.
- ^ a b Couch ET, Chaffee BW, Gansky SA, Walsh MM (July 2016). "The changing tobacco landscape: What dental professionals need to know". Journal of the American Dental Association. 147 (7): 561–569. doi:10.1016/j.adaj.2016.01.008. PMC 4925234. PMID 26988178.
- ^ Camenga DR, Tindle HA (July 2018). "Weighing the Risks and Benefits of Electronic Cigarette Use in High-Risk Populations". The Medical Clinics of North America. 102 (4): 765–779. doi:10.1016/j.mcna.2018.03.002. PMID 29933828. S2CID 49389902.
- ^ a b Drope J, Cahn Z, Kennedy R, Liber AC, Stoklosa M, Henson R, et al. (November 2017). "Key issues surrounding the health impacts of electronic nicotine delivery systems (ENDS) and other sources of nicotine". CA. 67 (6): 449–471. doi:10.3322/caac.21413. PMID 28961314.
- ^ a b Bhatnagar A (June 2016). "Cardiovascular Perspective of the Promises and Perils of E-Cigarettes". Circulation Research. 118 (12): 1872–1875. doi:10.1161/CIRCRESAHA.116.308723. PMC 5505630. PMID 27283531.
- ^ "Promote e-cigarettes widely as substitute for smoking says new RCP report". www.rcp.ac.uk. May 12, 2016. Retrieved 2025-01-15.
- ^ Katie Hunt (17 September 2019). "The US and UK see vaping very differently. Here's why". CNN.
- ^ "E-cigarettes: regulations for consumer products". GOV.UK. 12 July 2022.
- ^ "Public Health Consequences of E-Cigarettes" (PDF).
- ^ Palazzolo DL (November 2013). "Electronic cigarettes and vaping: a new challenge in clinical medicine and public health. A literature review". Frontiers in Public Health. 1: 56. doi:10.3389/fpubh.2013.00056. PMC 3859972. PMID 24350225.
- ^ a b c d e f Ebbert JO, Agunwamba AA, Rutten LJ (January 2015). "Counseling patients on the use of electronic cigarettes". Mayo Clinic Proceedings. 90 (1): 128–134. doi:10.1016/j.mayocp.2014.11.004. PMID 25572196.
- ^ a b c d e f g h i j k l m Rom O, Pecorelli A, Valacchi G, Reznick AZ (March 2015). "Are E-cigarettes a safe and good alternative to cigarette smoking?". Annals of the New York Academy of Sciences. 1340 (1): 65–74. Bibcode:2015NYASA1340...65R. doi:10.1111/nyas.12609. PMID 25557889. S2CID 26187171.
- ^ a b c d Kaisar MA, Prasad S, Liles T, Cucullo L (July 2016). "A decade of e-cigarettes: Limited research & unresolved safety concerns". Toxicology. 365: 67–75. Bibcode:2016Toxgy.365...67K. doi:10.1016/j.tox.2016.07.020. PMC 4993660. PMID 27477296.
- ^ a b Yang L, Rudy SF, Cheng JM, Durmowicz EL (May 2014). "Electronic cigarettes: incorporating human factors engineering into risk assessments". Tobacco Control. 23 (Supplement 2): ii47 – ii53. doi:10.1136/tobaccocontrol-2013-051479. PMC 3995290. PMID 24732164.
- ^ Khan MS, Khateeb F, Akhtar J, Khan Z, Lal A, Kholodovych V, et al. (March 2018). "Organizing pneumonia related to electronic cigarette use: A case report and review of literature". The Clinical Respiratory Journal. 12 (3): 1295–1299. doi:10.1111/crj.12775. PMID 29392888. S2CID 4316261.
- ^ a b c d Gualano MR, Passi S, Bert F, La Torre G, Scaioli G, Siliquini R (September 2015). "Electronic cigarettes: assessing the efficacy and the adverse effects through a systematic review of published studies". Journal of Public Health. 37 (3): 488–497. doi:10.1093/pubmed/fdu055. PMID 25108741.
- ^ a b c d e f g h Singh J, Luquet E, Smith DP, Potgieter HJ, Ragazzon P (December 2016). "Toxicological and analytical assessment of e-cigarette refill components on airway epithelia" (PDF). Science Progress. 99 (4): 351–398. doi:10.3184/003685016X14773090197706. PMC 10365464. PMID 28742478. S2CID 4573125.
- ^ a b c d e f g h i j k l m n o Stratton K, Kwan LY, Eaton DL (January 2018). Stratton K, Kwan LY, Eaton DL (eds.). Public Health Consequences of E-Cigarettes (PDF). National Academies of Sciences, Engineering, and Medicine (National Academies Press). pp. 1–774. doi:10.17226/24952. ISBN 978-0-309-46834-3. PMID 29894118.
- ^ Lauterstein D, Hoshino R, Gordon T, Watkins BX, Weitzman M, Zelikoff J (2014). "The changing face of tobacco use among United States youth". Current Drug Abuse Reviews. 7 (1): 29–43. doi:10.2174/1874473707666141015220110. PMC 4469045. PMID 25323124.
- ^ MacLean RR, Valentine GW, Jatlow PI, Sofuoglu M (February 2017). "Inhalation of Alcohol Vapor: Measurement and Implications". Alcoholism: Clinical and Experimental Research. 41 (2): 238–250. doi:10.1111/acer.13291. PMC 6143144. PMID 28054395.
- ^ a b c d e f g h i j k l m n o p q Qasim H, Karim ZA, Rivera JO, Khasawneh FT, Alshbool FZ (August 2017). "Impact of Electronic Cigarettes on the Cardiovascular System". Journal of the American Heart Association. 6 (9): e006353. doi:10.1161/JAHA.117.006353. PMC 5634286. PMID 28855171.
- ^ a b c d e f "Electronic Cigarette Fires and Explosions in the United States 2009 – 2016" (PDF). United States Fire Administration. July 2017. pp. 1–56.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ "Know the Risks". Surgeon General of the United States. 2016.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ a b c Weaver M, Breland A, Spindle T, Eissenberg T (2014). "Electronic cigarettes: a review of safety and clinical issues". Journal of Addiction Medicine. 8 (4): 234–240. doi:10.1097/ADM.0000000000000043. PMC 4123220. PMID 25089953.
- ^ a b c d e f g h i j Rowell TR, Tarran R (December 2015). "Will chronic e-cigarette use cause lung disease?". American Journal of Physiology. Lung Cellular and Molecular Physiology. 309 (12): L1398 – L1409. doi:10.1152/ajplung.00272.2015. PMC 4683316. PMID 26408554.
- ^ a b c d Paley GL, Echalier E, Eck TW, Hong AR, Farooq AV, Gregory DG, et al. (July 2016). "Corneoscleral Laceration and Ocular Burns Caused by Electronic Cigarette Explosions". Cornea. 35 (7): 1015–1018. doi:10.1097/ICO.0000000000000881. PMC 4900417. PMID 27191672.
- ^ a b c d Vaught B, Spellman J, Shah A, Stewart A, Mullin D (March 2017). "Facial trauma caused by electronic cigarette explosion". Ear, Nose, & Throat Journal. 96 (3): 139–142. doi:10.1177/014556131709600314. PMID 28346645.
- ^ Serror K, Chaouat M, Legrand MM, Depret F, Haddad J, Malca N, et al. (May 2018). "Burns caused by electronic vaping devices (e-cigarettes): A new classification proposal based on mechanisms". Burns. 44 (3): 544–548. doi:10.1016/j.burns.2017.09.005. PMID 29056367.
- ^ Makadia LD, Roper PJ, Andrews JO, Tingen MS (August 2017). "Tobacco Use and Smoke Exposure in Children: New Trends, Harm, and Strategies to Improve Health Outcomes". Current Allergy and Asthma Reports. 17 (8): 55. doi:10.1007/s11882-017-0723-0. PMID 28741144. S2CID 22360961.
- ^ a b Harshman J, Vojvodic M, Rogers AD (October 2018). "Burns associated with e-cigarette batteries: A case series and literature review". CJEM. 20 (S2): S20 – S28. doi:10.1017/cem.2017.32. PMID 28566106.
- ^ Hickey S, Goverman J, Friedstat J, Sheridan R, Schulz J (August 2018). "Thermal injuries from exploding electronic cigarettes". Burns. 44 (5): 1294–1301. doi:10.1016/j.burns.2018.02.008. PMID 29503045. S2CID 3709168.
- ^ Patterson SB, Beckett AR, Lintner A, Leahey C, Greer A, Brevard SB, et al. (2017). "A Novel Classification System for Injuries After Electronic Cigarette Explosions". Journal of Burn Care & Research. 38 (1): e95 – e100. doi:10.1097/BCR.0000000000000471. PMID 27893577. S2CID 3433324.
- ^ Arnaout A, Khashaba H, Dobbs T, Dewi F, Pope-Jones S, Sack A, et al. (June 2017). "The Southwest UK Burns Network (SWUK) experience of electronic cigarette explosions and review of literature". Burns. 43 (4): e1 – e6. doi:10.1016/j.burns.2017.01.008. PMID 28412133.
- ^ Caplan D (22 December 2016). "Man Suffers 3rd-Degree Burns After E-Cigarette Explodes in His Pocket While Riding Bus". ABC News.
- ^ Sheckter C, Chattopadhyay A, Paro J, Karanas Y (2016). "Burns resulting from spontaneous combustion of electronic cigarettes: a case series". Burns & Trauma. 4 (1): 35. doi:10.1186/s41038-016-0061-9. PMC 5151131. PMID 27995151.
 This article incorporates text by Clifford Sheckter, Arhana Chattopadhyay, John Paro and Yvonne Karanas available under the CC BY 4.0 license.
This article incorporates text by Clifford Sheckter, Arhana Chattopadhyay, John Paro and Yvonne Karanas available under the CC BY 4.0 license.
- ^ Lacasse Y, Légaré M, Maltais F (2015). "E-cigarette use in patients receiving home oxygen therapy". Canadian Respiratory Journal. 22 (2): 83–85. doi:10.1155/2015/215932. PMC 4390016. PMID 25848719.
 This article incorporates text by Yves Lacasse, Martin Légaré, and François Maltais available under the CC BY 4.0 license.
This article incorporates text by Yves Lacasse, Martin Légaré, and François Maltais available under the CC BY 4.0 license.
- ^ Detailed reference list is located at a separate image page.
- ^ Jo CL, Ambs A, Dresler CM, Backinger CL (February 2017). "Child-resistant and tamper-resistant packaging: A systematic review to inform tobacco packaging regulation". Preventive Medicine. 95: 89–95. doi:10.1016/j.ypmed.2016.11.013. PMC 5299541. PMID 27939602.
- ^ a b c d e f Hua M, Talbot P (December 2016). "Potential health effects of electronic cigarettes: A systematic review of case reports". Preventive Medicine Reports. 4: 169–178. doi:10.1016/j.pmedr.2016.06.002. PMC 4929082. PMID 27413679.
 This article incorporates text available under the CC BY 4.0 license.
This article incorporates text available under the CC BY 4.0 license.
- ^ a b c Biyani S, Derkay CS (August 2015). "E-cigarettes: Considerations for the otolaryngologist". International Journal of Pediatric Otorhinolaryngology. 79 (8): 1180–1183. doi:10.1016/j.ijporl.2015.04.032. PMID 25998217.
- ^ a b c d e Kim KH, Kabir E, Jahan SA (October 2016). "Review of electronic cigarettes as tobacco cigarette substitutes: Their potential human health impact". Journal of Environmental Science and Health. Part C, Environmental Carcinogenesis & Ecotoxicology Reviews. 34 (4): 262–275. Bibcode:2016JESHC..34..262K. doi:10.1080/10590501.2016.1236604. PMID 27635466. S2CID 42660975.
- ^ a b Gordon T, Karey E, Rebuli ME, Escobar YN, Jaspers I, Chen LC (2022-01-06). "E-Cigarette Toxicology". Annual Review of Pharmacology and Toxicology. 62: 301–322. doi:10.1146/annurev-pharmtox-042921-084202. ISSN 0362-1642. PMC 9386787. PMID 34555289.
- ^ Chatham-Stephens K, Law R, Taylor E, Melstrom P, Bunnell R, Wang B, et al. (April 2014). "Notes from the field: calls to poison centers for exposures to electronic cigarettes--United States, September 2010-February 2014". MMWR. Morbidity and Mortality Weekly Report. 63 (13): 292–293. PMC 5779356. PMID 24699766.
- ^ a b c d e Chatham-Stephens K, Law R, Taylor E, Kieszak S, Melstrom P, Bunnell R, et al. (December 2016). "Exposure Calls to U. S. Poison Centers Involving Electronic Cigarettes and Conventional Cigarettes-September 2010-December 2014". Journal of Medical Toxicology. 12 (4): 350–357. doi:10.1007/s13181-016-0563-7. PMC 5135675. PMID 27352081.
- ^ Nelluri BK, Murphy K, Mookadam F (May 2015). "Electronic cigarettes and cardiovascular risk: hype or up in smoke?". Future Cardiology. 11 (3): 271–273. doi:10.2217/fca.15.13. PMID 26021631.
- ^ Chatham-Stephens K (20 October 2014). "Young Children and e-Cigarette Poisoning". Medscape.
- ^ a b c Govindarajan P, Spiller HA, Casavant MJ, Chounthirath T, Smith GA (May 2018). "E-Cigarette and Liquid Nicotine Exposures Among Young Children". Pediatrics. 141 (5): e20173361. doi:10.1542/peds.2017-3361. PMID 29686144.
- ^ a b c "Some E-cigarette Users Are Having Seizures, Most Reports Involving Youth and Young Adults". United States Food and Drug Administration. 3 April 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ Jenssen BP, Walley SC (February 2019). "E-Cigarettes and Similar Devices". Pediatrics. 143 (2): e20183652. doi:10.1542/peds.2018-3652. PMC 6644065. PMID 30835247.
- ^ a b "New CDC study finds dramatic increase in e-cigarette-related calls to poison centers". Centers for Disease Control and Prevention. 3 April 2014.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ a b Kamboj A, Spiller HA, Casavant MJ, Chounthirath T, Smith GA (June 2016). "Pediatric Exposure to E-Cigarettes, Nicotine, and Tobacco Products in the United States". Pediatrics. 137 (6): e20160041. doi:10.1542/peds.2016-0041. PMID 27244861.
- ^ "E-Cigarettes and Liquid Nicotine". American Association of Poison Control Centers. 2018.
- ^ a b Peterson LA, Hecht SS (April 2017). "Tobacco, e-cigarettes, and child health". Current Opinion in Pediatrics. 29 (2): 225–230. doi:10.1097/MOP.0000000000000456. PMC 5598780. PMID 28059903.
- ^ a b c d e f g Orellana-Barrios MA, Payne D, Mulkey Z, Nugent K (July 2015). "Electronic Cigarettes—A Narrative Review for Clinicians". The American Journal of Medicine. 128 (7): 674–681. doi:10.1016/j.amjmed.2015.01.033. PMID 25731134.
- ^ a b c d e Drummond MB, Upson D (February 2014). "Electronic cigarettes. Potential harms and benefits". Annals of the American Thoracic Society. 11 (2): 236–242. doi:10.1513/annalsats.201311-391fr. PMC 5469426. PMID 24575993.
- ^ a b c d e f g h i Clapp PW, Jaspers I (October 2017). "Electronic Cigarettes: Their Constituents and Potential Links to Asthma". Current Allergy and Asthma Reports. 17 (11): 79. doi:10.1007/s11882-017-0747-5. PMC 5995565. PMID 28983782.
- ^ a b Wyman AE, Hines SE (April 2018). "Update on metal-induced occupational lung disease". Current Opinion in Allergy and Clinical Immunology. 18 (2): 73–79. doi:10.1097/ACI.0000000000000420. PMID 29337701. S2CID 3613573.
- ^ a b c d e f g h i Cai H, Wang C (October 2017). "Graphical review: The redox dark side of e-cigarettes; exposure to oxidants and public health concerns". Redox Biology. 13: 402–406. doi:10.1016/j.redox.2017.05.013. PMC 5493817. PMID 28667909.
- ^ a b c d e f g Shields PG, Berman M, Brasky TM, Freudenheim JL, Mathe E, McElroy JP, et al. (August 2017). "A Review of Pulmonary Toxicity of Electronic Cigarettes in the Context of Smoking: A Focus on Inflammation". Cancer Epidemiology, Biomarkers & Prevention. 26 (8): 1175–1191. doi:10.1158/1055-9965.EPI-17-0358. PMC 5614602. PMID 28642230.
- ^ a b Harrell PT, Simmons VN, Correa JB, Padhya TA, Brandon TH (September 2014). "Electronic nicotine delivery systems ("e-cigarettes"): review of safety and smoking cessation efficacy". Otolaryngology–Head and Neck Surgery. 151 (3): 381–393. doi:10.1177/0194599814536847. PMC 4376316. PMID 24898072.
- ^ a b c d e f g h i j k Bertholon JF, Becquemin MH, Annesi-Maesano I, Dautzenberg B (2013). "Electronic cigarettes: a short review". Respiration; International Review of Thoracic Diseases. 86 (5): 433–438. doi:10.1159/000353253. PMID 24080743. S2CID 20521181.
- ^ a b Zainol Abidin N, Zainal Abidin E, Zulkifli A, Karuppiah K, Syed Ismail SN, Amer Nordin AS (September 2017). "Electronic cigarettes and indoor air quality: a review of studies using human volunteers" (PDF). Reviews on Environmental Health. 32 (3): 235–244. doi:10.1515/reveh-2016-0059. PMID 28107173. S2CID 6885414.
- ^ Cite error: The named reference
msn18was invoked but never defined (see the help page). - ^ Barraza LF, Weidenaar KE, Cook LT, Logue AR, Halpern MT (August 2017). "Regulations and policies regarding e-cigarettes". Cancer. 123 (16): 3007–3014. doi:10.1002/cncr.30725. PMID 28440949. S2CID 45269159.
- ^ a b c Collaco JM, Drummond MB, McGrath-Morrow SA (February 2015). "Electronic cigarette use and exposure in the pediatric population". JAMA Pediatrics. 169 (2): 177–182. doi:10.1001/jamapediatrics.2014.2898. PMC 5557497. PMID 25546699.
- ^ a b Boudi FB, Patel S, Boudi A, Chan C (December 2019). "Vitamin E Acetate as a Plausible Cause of Acute Vaping-related Illness". Cureus. 11 (12): e6350. doi:10.7759/cureus.6350. PMC 6952050. PMID 31938636.
 This article incorporates text by F Brian Boudi, Sonia Patel, Ava Boudi, Connie Chan available under the CC BY 3.0 license.
This article incorporates text by F Brian Boudi, Sonia Patel, Ava Boudi, Connie Chan available under the CC BY 3.0 license.
- ^ a b c d Benowitz NL, Fraiman JB (August 2017). "Cardiovascular effects of electronic cigarettes". Nature Reviews. Cardiology. 14 (8): 447–456. doi:10.1038/nrcardio.2017.36. PMC 5519136. PMID 28332500.
- ^ Henry TS, Kligerman SJ, Raptis CA, Mann H, Sechrist JW, Kanne JP (March 2020). "Imaging Findings of Vaping-Associated Lung Injury". AJR. American Journal of Roentgenology. 214 (3): 498–505. doi:10.2214/AJR.19.22251. PMID 31593518. S2CID 203985885.
- ^ a b c d e "Outbreak of Lung Injury Associated with E-Cigarette Use, or Vaping". Centers for Disease Control and Prevention. 28 January 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ Layden JE, Ghinai I, Pray I, Kimball A, Layer M, Tenforde MW, et al. (5 March 2020). "Pulmonary Illness Related to E-Cigarette Use in Illinois and Wisconsin — Final Report". New England Journal of Medicine. 382 (10): 903–916. doi:10.1056/NEJMoa1911614. ISSN 0028-4793. PMID 31491072.
{{cite journal}}: CS1 maint: overridden setting (link) - ^ Kelland K (14 October 2019). "Vaping illness, deaths likely very rare beyond U.S., experts say". Reuters.
- ^ a b "New CDC Report Provides First Analysis of Lung Injury Deaths Associated with Use of E-cigarette, or Vaping, Products | CDC". www.cdc.gov. 28 October 2019. Retrieved 19 June 2020.
- ^ "E-cigarette, or Vaping, Associated Lung Injury (EVALI) California Brief Update". cdph.ca.gov. 4 January 2022. Retrieved 3 June 2022.
- ^ Klenske N (March 10, 2022). "Differentiating EVALI from COVID-19 on Imaging Proves Challenging". Radiological Society of North America. Retrieved August 1, 2022.
- ^ Blagev DP, Callahan SJ, Harris D, Collingridge DS, Hopkins RO, Eve JR, et al. (9 May 2022). "Prospectively Assessed Long-Term Outcomes of Patients with E-cigarette or Vaping-associated Lung Injury (EVALI)". Annals of the American Thoracic Society. 19 (11): AnnalsATS.202201–049OC. doi:10.1513/AnnalsATS.202201-049OC. PMC 9667811. PMID 35533314. S2CID 248669259.
- ^ "Transcript of September 6, 2019, Telebriefing: Investigation of Pulmonary Disease Among People Who Use E-cigarettes". Centers for Disease Control and Prevention. 6 September 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ King BA, Jones CM, Baldwin GT, Briss PA (2020). "The EVALI and Vaping Epidemics — Implications for Public Health". New England Journal of Medicine. 382 (8): 689–691. doi:10.1056/NEJMp1916171. ISSN 0028-4793. PMC 7122126. PMID 31951683.
- ^ Siddiqi TJ, Rashid AM, Siddiqi AK, Anwer A, Usman MS, Sakhi H, et al. (September 2023). "Cardiovascular effects of electronic cigarettes: A systematic review and meta-analysis". Current Problems in Cardiology. 48 (9): 101748. doi:10.1016/j.cpcardiol.2023.101748. PMID 37088177.
- ^ Zong H, Hu Z, Li W (20 February 2024). "Electronic cigarettes and cardiovascular disease: epidemiological and biological links". European Journal of Physiology. 476 (6): 875–888. doi:10.1007/s00424-024-02925-0. PMC 11139732. PMID 38376568.
- ^ Skotsimara G, Antonopoulos AS, Oikonomou E, Siasos G, Ioakeimidis N, Tsalamandris S, et al. (July 2019). "Cardiovascular effects of electronic cigarettes: A systematic review and meta-analysis". European Journal of Preventive Cardiology. 26 (11): 1219–1228. doi:10.1177/2047487319832975. PMID 30823865. S2CID 73506976.
- ^ Knura M, Dragon J, Łabuzek K, Okopień B (January 2018). "The impact of electronic cigarettes usage on the endothelial function and the progression of atherosclerosis". Polski Merkuriusz Lekarski. 44 (259): 26–30. PMID 29374420.
- ^ a b c Lippi G, Favaloro EJ, Meschi T, Mattiuzzi C, Borghi L, Cervellin G (February 2014). "E-cigarettes and cardiovascular risk: beyond science and mysticism". Seminars in Thrombosis and Hemostasis. 40 (1): 60–65. doi:10.1055/s-0033-1363468. PMID 24343348.
- ^ a b Nelluri B, Murphy K, Mookadam F, Mookadam M (March 2016). "The current literature regarding the cardiovascular effects of electronic cigarettes". Future Cardiology. 12 (2): 167–179. doi:10.2217/fca.15.83. PMID 26916427.
- ^ Turner JR (November 2009). "Intestinal mucosal barrier function in health and disease". Nature Reviews Immunology. 9 (11): 799–809. doi:10.1038/nri2653. ISSN 1474-1741. PMID 19855405.
- ^ a b Oshima T, Miwa H (August 2016). "Gastrointestinal mucosal barrier function and diseases". Journal of Gastroenterology. 51 (8): 768–778. doi:10.1007/s00535-016-1207-z. ISSN 1435-5922. PMID 27048502.
- ^ a b Sharma A, Lee J, Fonseca AG, Moshensky A, Kothari T, Sayed IM, et al. (2021-01-06). "E-cigarettes compromise the gut barrier and trigger inflammation". iScience. 24 (2): 102035. Bibcode:2021iSci...24j2035S. doi:10.1016/j.isci.2021.102035. ISSN 2589-0042. PMC 7841355. PMID 33537654.
- ^ Sharma A, Lee J, Fonseca A, Crotty-Alexander L, Ghosh P (February 19, 2021). "E-cigarettes compromise the gut barrier and trigger inflammation". iScience. 24 (2). Bibcode:2021iSci...24j2035S. doi:10.1016/j.isci.2021.102035. PMC 7841355. PMID 33537654.
- ^ Debnath M, Debnath D, Singh P, Wert Y, Nookala V (July 24, 2022). "Effect of Electronic Cigarettes on the Gastrointestinal System". Cureus. 14 (7): e27210. doi:10.7759/cureus.27210. ISSN 2168-8184. PMC 9322142. PMID 35903484.
- ^ López-Ojeda W, Hurley RA (January 2024). "Vaping and the Brain: Effects of Electronic Cigarettes and E-Liquid Substances". The Journal of Neuropsychiatry and Clinical Neurosciences. 36 (1): A5–5. doi:10.1176/appi.neuropsych.20230184. ISSN 0895-0172. PMID 38226910.
- ^ Heldt NA, Seliga A, Winfield M, Gajghate S, Reichenbach N, Yu X, et al. (August 2020). "Electronic cigarette exposure disrupts blood-brain barrier integrity and promotes neuroinflammation". Brain, Behavior, and Immunity. 88: 363–380. doi:10.1016/j.bbi.2020.03.034. ISSN 1090-2139. PMC 7899242. PMID 32243899.
- ^ Toda N, Toda H (December 2010). "Nitric oxide-mediated blood flow regulation as affected by smoking and nicotine". European Journal of Pharmacology. 649 (1–3): 1–13. doi:10.1016/j.ejphar.2010.09.042. PMID 20868673.
- ^ a b Javed F, Kellesarian SV, Sundar IK, Romanos GE, Rahman I (November 2017). "Recent updates on electronic cigarette aerosol and inhaled nicotine effects on periodontal and pulmonary tissues". Oral Diseases. 23 (8): 1052–1057. doi:10.1111/odi.12652. PMC 5545167. PMID 28168771.
- ^ Chaffee BW, Couch ET, Ryder MI (June 2016). "The tobacco-using periodontal patient: role of the dental practitioner in tobacco cessation and periodontal disease management". Periodontology 2000. 71 (1): 52–64. doi:10.1111/prd.12120. PMC 4842013. PMID 27045430.
- ^ a b Sultan AS, Jessri M, Farah CS (March 2021). "Electronic nicotine delivery systems: Oral health implications and oral cancer risk". Journal of Oral Pathology & Medicine. 50 (3): 316–322. doi:10.1111/jop.12810. PMID 30507043. S2CID 54527046.
- ^ Visconti MJ, Ashack KA (October 2019). "Dermatologic manifestations associated with electronic cigarette use". Journal of the American Academy of Dermatology. 81 (4): 1001–1007. doi:10.1016/j.jaad.2019.03.088. PMID 30965061. S2CID 106409405.
- ^ Giroud C, de Cesare M, Berthet A, Varlet V, Concha-Lozano N, Favrat B (August 2015). "E-Cigarettes: A Review of New Trends in Cannabis Use". International Journal of Environmental Research and Public Health. 12 (8): 9988–10008. doi:10.3390/ijerph120809988. PMC 4555324. PMID 26308021.
 This article incorporates text by Christian Giroud, Mariangela de Cesare, Aurélie Berthet, Vincent Varlet, Nicolas Concha-Lozano, and Bernard Favrat available under the CC BY 4.0 license.
This article incorporates text by Christian Giroud, Mariangela de Cesare, Aurélie Berthet, Vincent Varlet, Nicolas Concha-Lozano, and Bernard Favrat available under the CC BY 4.0 license.
- ^ Boakye E, El Shahawy O, Obisesan O, Dzaye O, Osei AD, Erhabor J, et al. (2022-10-17). "The inverse association of state cannabis vaping prevalence with the e-cigarette or vaping product-use associated lung injury". PLOS ONE. 17 (10): e0276187. Bibcode:2022PLoSO..1776187B. doi:10.1371/journal.pone.0276187. ISSN 1932-6203. PMC 9576092. PMID 36251673.
- ^ a b c d Franck C, Filion KB, Kimmelman J, Grad R, Eisenberg MJ (May 2016). "Ethical considerations of e-cigarette use for tobacco harm reduction". Respiratory Research. 17 (1): 53. doi:10.1186/s12931-016-0370-3. PMC 4869264. PMID 27184265.
 This article incorporates text by Caroline Franck, Kristian B. Filion, Jonathan Kimmelman, Roland Grad and Mark J. Eisenberg available under the CC BY 4.0 license.
This article incorporates text by Caroline Franck, Kristian B. Filion, Jonathan Kimmelman, Roland Grad and Mark J. Eisenberg available under the CC BY 4.0 license.
- ^ a b c Wilder N, Daley C, Sugarman J, Partridge J (April 2016). "Nicotine without smoke: Tobacco harm reduction". UK: Royal College of Physicians. pp. 1–191.
- ^ a b Nowak D, Jörres RA, Rüther T (May 2014). "E-cigarettes--prevention, pulmonary health, and addiction". Deutsches Ärzteblatt International. 111 (20): 349–355. doi:10.3238/arztebl.2014.0349. PMC 4047602. PMID 24882626.
- ^ Neuberger M (May 2015). "The electronic cigarette: a wolf in sheep's clothing". Wiener Klinische Wochenschrift. 127 (9–10): 385–387. doi:10.1007/s00508-015-0753-3. PMID 26230008. S2CID 10172525.
- ^ Hess IM, Lachireddy K, Capon A (April 2016). "A systematic review of the health risks from passive exposure to electronic cigarette vapour". Public Health Research & Practice. 26 (2). doi:10.17061/phrp2621617. PMID 27734060.
- ^ a b c d e f g h i j k "E-Cigarette Use Among Youth and Young Adults: A Report of the Surgeon General" (PDF). Surgeon General of the United States. 2016. pp. 1–298.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ Fernández E, Ballbè M, Sureda X, Fu M, Saltó E, Martínez-Sánchez JM (December 2015). "Particulate Matter from Electronic Cigarettes and Conventional Cigarettes: a Systematic Review and Observational Study". Current Environmental Health Reports. 2 (4): 423–429. Bibcode:2015CEHR....2..423F. doi:10.1007/s40572-015-0072-x. PMID 26452675.
- ^ "American Lung Association Statement on E-Cigarettes". American Lung Association. 25 August 2014.
- ^ a b Collaco JM, McGrath-Morrow SA (April 2018). "Electronic Cigarettes: Exposure and Use Among Pediatric Populations". Journal of Aerosol Medicine and Pulmonary Drug Delivery. 31 (2): 71–77. doi:10.1089/jamp.2017.1418. PMC 5915214. PMID 29068754.
- ^ "Surgeon General Reports Youth and Young Adult E-Cigarette Use Poses a Public Health Threat". United States Department of Health and Human Services. 8 December 2016. Archived from the original on 28 January 2017. Retrieved 13 March 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ Glasser AM, Collins L, Pearson JL, Abudayyeh H, Niaura RS, Abrams DB, et al. (February 2017). "Overview of Electronic Nicotine Delivery Systems: A Systematic Review". American Journal of Preventive Medicine. 52 (2): e33 – e66. doi:10.1016/j.amepre.2016.10.036. PMC 5253272. PMID 27914771.
- ^ "e-Cigarettes: a safe way to quit?". NPS MedicineWise. 11 June 2014. Archived from the original on 19 March 2017.
- ^ Bam TS, Bellew W, Berezhnova I, Jackson-Morris A, Jones A, Latif E, et al. (January 2014). "Position statement on electronic cigarettes or electronic nicotine delivery systems". The International Journal of Tuberculosis and Lung Disease. 18 (1): 5–7. doi:10.5588/ijtld.13.0815. PMID 24365545. S2CID 26481455.
- ^ "White Paper: Electronic Cigarettes in the Indoor Environment" (PDF). American Industrial Hygiene Association. 19 October 2014. Archived from the original (PDF) on 25 January 2017. Retrieved 18 August 2016.
- ^ Dautzenberg B, Adler M, Garelik D, Loubrieu JF, Mathern G, Peiffer G, et al. (February 2017). "Practical guidelines on e-cigarettes for practitioners and others health professionals. A French 2016 expert's statement". Revue des Maladies Respiratoires. 34 (2): 155–164. doi:10.1016/j.rmr.2017.01.001. PMID 28189437.
- ^ Cite error: The named reference
who16was invoked but never defined (see the help page). - ^ "E-cigarettes not proven quitting aid, says BMA". British Medical Association. 30 January 2013. Archived from the original on 26 February 2013.
- ^ a b Kaur J, Rinkoo AV (September 2017). "Getting real with the upcoming challenge of electronic nicotine delivery systems: The way forward for the South-East Asia region". Indian Journal of Public Health. 61 (Suppl 1): S7 – S11. doi:10.4103/ijph.IJPH_240_17. PMID 28928312.
- ^ Cite error: The named reference
chap20was invoked but never defined (see the help page). - ^ a b c Burstyn I (January 2014). "Peering through the mist: systematic review of what the chemistry of contaminants in electronic cigarettes tells us about health risks". BMC Public Health. 14 (1): 18. doi:10.1186/1471-2458-14-18. PMC 3937158. PMID 24406205.
- ^ Meo SA, Al Asiri SA (2014). "Effects of electronic cigarette smoking on human health" (PDF). European Review for Medical and Pharmacological Sciences. 18 (21): 3315–3319. PMID 25487945.
- ^ Biyani S, Derkay CS (March 2017). "E-cigarettes: An update on considerations for the otolaryngologist". International Journal of Pediatric Otorhinolaryngology. 94: 14–16. doi:10.1016/j.ijporl.2016.12.027. PMID 28167004.
- ^ Frey LT, Tilburg WC (February 2016). "Child-Resistant Packaging for E-Liquid: A Review of US State Legislation". American Journal of Public Health. 106 (2): 266–268. doi:10.2105/AJPH.2015.302957. PMC 4815607. PMID 26691114.
- ^ a b c d Jimenez Ruiz CA, Solano Reina S, de Granda Orive JI, Signes-Costa Minaya J, de Higes Martinez E, Riesco Miranda JA, et al. (August 2014). "The electronic cigarette. Official statement of the Spanish Society of Pneumology and Thoracic Surgery (SEPAR) on the efficacy, safety and regulation of electronic cigarettes". Archivos de Bronconeumologia. 50 (8): 362–367. doi:10.1016/j.arbres.2014.02.006. PMID 24684764.
- ^ a b Dagaonkar RS, Udwadi ZF (April 2014). "Water pipes and E-cigarettes: new faces of an ancient enemy" (PDF). The Journal of the Association of Physicians of India. 62 (4): 324–328. PMID 25327035. Archived from the original (PDF) on 2016-03-04. Retrieved 2015-02-25.
- ^ Mayer B (January 2014). "How much nicotine kills a human? Tracing back the generally accepted lethal dose to dubious self-experiments in the nineteenth century". Archives of Toxicology. 88 (1): 5–7. Bibcode:2014ArTox..88....5M. doi:10.1007/s00204-013-1127-0. PMC 3880486. PMID 24091634.
- ^ England LJ, Bunnell RE, Pechacek TF, Tong VT, McAfee TA (August 2015). "Nicotine and the Developing Human: A Neglected Element in the Electronic Cigarette Debate". American Journal of Preventive Medicine. 49 (2): 286–293. doi:10.1016/j.amepre.2015.01.015. PMC 4594223. PMID 25794473.
- ^ Brown CJ, Cheng JM (May 2014). "Electronic cigarettes: product characterisation and design considerations". Tobacco Control. 23 (Supplement 2): ii4 – i10. doi:10.1136/tobaccocontrol-2013-051476. PMC 3995271. PMID 24732162.
- ^ a b c d Pepper JK, Brewer NT (September 2014). "Electronic nicotine delivery system (electronic cigarette) awareness, use, reactions and beliefs: a systematic review". Tobacco Control. 23 (5): 375–384. doi:10.1136/tobaccocontrol-2013-051122. PMC 4520227. PMID 24259045.
- ^ a b Modesto-Lowe V, Alvarado C (September 2017). "E-cigs . . . Are They Cool? Talking to Teens About E-Cigarettes". Clinical Pediatrics. 56 (10): 947–952. doi:10.1177/0009922817705188. PMID 28443340. S2CID 44423931.
- ^ "Do You Vape? See These Tips on How to Keep E-Liquids Away from Children". United States Food and Drug Administration. 2 May 2018.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ "E-Cigarette Poisonings Among Toddlers Skyrocketed 1500% Over 3 Years". Yahoo! News. 9 May 2016.
- ^ a b c d e f g Bhatnagar A, Whitsel LP, Ribisl KM, Bullen C, Chaloupka F, Piano MR, et al. (October 2014). "Electronic cigarettes: a policy statement from the American Heart Association". Circulation. 130 (16): 1418–1436. doi:10.1161/CIR.0000000000000107. PMC 7643636. PMID 25156991.
- ^ a b "Be Smoke-free and Help Your Pets Live Longer, Healthier Lives - Electronic Nicotine Delivery Systems". United States Food and Drug Administration. 19 October 2017.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ https://www.poisoncontrol.org/home/ Texas Poison Control Network
- ^ "E-cigarettes and Pet Safety". VCA Corporate. 2019.
- ^ a b "Cancer Research UK Briefing: Electronic Cigarettes" (PDF). Cancer Research UK. May 2014.
- ^ Orr MS (May 2014). "Electronic cigarettes in the USA: a summary of available toxicology data and suggestions for the future". Tobacco Control. 23 (Supplement 2): ii18 – ii22. doi:10.1136/tobaccocontrol-2013-051474. PMC 3995288. PMID 24732158.
- ^ Rahman MA, Hann N, Wilson A, Worrall-Carter L (2014). "Electronic cigarettes: patterns of use, health effects, use in smoking cessation and regulatory issues". Tobacco Induced Diseases. 12 (1): 21. doi:10.1186/1617-9625-12-21. PMC 4350653. PMID 25745382.
- ^ Xu Y, Guo Y, Liu K, Liu Z, Wang X (2016). "E-Cigarette Awareness, Use, and Harm Perception among Adults: A Meta-Analysis of Observational Studies". PLOS ONE. 11 (11): e0165938. Bibcode:2016PLoSO..1165938X. doi:10.1371/journal.pone.0165938. PMC 5115669. PMID 27861501.
- ^ Caponnetto P, Russo C, Bruno CM, Alamo A, Amaradio MD, Polosa R (March 2013). "Electronic cigarette: a possible substitute for cigarette dependence". Monaldi Archives for Chest Disease = Archivio Monaldi per le Malattie del Torace. 79 (1): 12–19. doi:10.4081/monaldi.2013.104. PMID 23741941.
- ^ "E-cigarettes to be regulated as medicines". National Health Service. 12 June 2013. Archived from the original on 17 December 2015. Retrieved 21 November 2014.
- ^ a b c d Jerry JM, Collins GB, Streem D (August 2015). "E-cigarettes: Safe to recommend to patients?". Cleveland Clinic Journal of Medicine. 82 (8): 521–526. doi:10.3949/ccjm.82a.14054. PMID 26270431.
- ^ National Center for Chronic Disease Prevention Health Promotion (US) Office on Smoking Health (2014). The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Surgeon General of the United States. pp. 1–943. PMID 24455788.
- ^ a b c d e f g h i j k l Sanner T, Grimsrud TK (2015). "Nicotine: Carcinogenicity and Effects on Response to Cancer Treatment - A Review". Frontiers in Oncology. 5: 196. doi:10.3389/fonc.2015.00196. PMC 4553893. PMID 26380225.
 This article incorporates text available under the CC BY 4.0 license.
This article incorporates text available under the CC BY 4.0 license.
- ^ Schaal C, Chellappan SP (January 2014). "Nicotine-mediated cell proliferation and tumor progression in smoking-related cancers". Molecular Cancer Research. 12 (1): 14–23. doi:10.1158/1541-7786.MCR-13-0541. PMC 3915512. PMID 24398389.
- ^ Mravec B, Tibensky M, Horvathova L, Babal P (February 2020). "E-Cigarettes and Cancer Risk". Cancer Prevention Research. 13 (2): 137–144. doi:10.1158/1940-6207.CAPR-19-0346. PMID 31619443.
- ^ a b "Electronic Nicotine Delivery Systems and Electronic Non-Nicotine Delivery Systems (ENDS/ENNDS)" (PDF). World Health Organization WHO. August 2016. pp. 1–11.
- ^ Flach S, Maniam P, Manickavasagam J (September 2019). "E-cigarettes and head and neck cancers: A systematic review of the current literature". Clinical Otolaryngology. 44 (5): 749–756. doi:10.1111/coa.13384. PMID 31148389. S2CID 171094189.
- ^ Knorst MM, Benedetto IG, Hoffmeister MC, Gazzana MB (October 2014). "The electronic cigarette: the new cigarette of the 21st century?". Jornal Brasileiro de Pneumologia. 40 (5): 564–572. doi:10.1590/S1806-37132014000500013. PMC 4263338. PMID 25410845.
- ^ a b Hiemstra PS, Bals R (October 2016). "Basic science of electronic cigarettes: assessment in cell culture and in vivo models". Respiratory Research. 17 (1): 127. doi:10.1186/s12931-016-0447-z. PMC 5055681. PMID 27717371.
 This article incorporates text available under the CC BY 4.0 license.
This article incorporates text available under the CC BY 4.0 license.
- ^ Arnold C (September 2014). "Vaping and health: what do we know about e-cigarettes?". Environmental Health Perspectives. 122 (9): A244 – A249. doi:10.1289/ehp.122-A244. PMC 4154203. PMID 25181730.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ a b Alawsi F, Nour R, Prabhu S (August 2015). "Are e-cigarettes a gateway to smoking or a pathway to quitting?". British Dental Journal. 219 (3): 111–115. doi:10.1038/sj.bdj.2015.591. PMID 26271862. S2CID 24120636.
- ^ Papaefstathiou E, Stylianou M, Agapiou A (May 2019). "Main and side stream effects of electronic cigarettes". Journal of Environmental Management. 238: 10–17. Bibcode:2019JEnvM.238...10P. doi:10.1016/j.jenvman.2019.01.030. PMID 30836280. S2CID 73462201.
- ^ "Known and Probable Human Carcinogens".
- ^ a b c d e f g Bekki K, Uchiyama S, Ohta K, Inaba Y, Nakagome H, Kunugita N (October 2014). "Carbonyl compounds generated from electronic cigarettes". International Journal of Environmental Research and Public Health. 11 (11): 11192–11200. doi:10.3390/ijerph111111192. PMC 4245608. PMID 25353061.
- ^ Dinakar C, O'Connor GT (October 2016). "The Health Effects of Electronic Cigarettes". The New England Journal of Medicine. 375 (14): 1372–1381. doi:10.1056/NEJMra1502466. PMID 27705269.
- ^ a b c Schick SF, Blount BC, Jacob P, Saliba NA, Bernert JT, El Hellani A, et al. (September 2017). "Biomarkers of exposure to new and emerging tobacco delivery products". American Journal of Physiology. Lung Cellular and Molecular Physiology. 313 (3): L425 – L452. doi:10.1152/ajplung.00343.2016. PMC 5626373. PMID 28522563.
- ^ a b c d Ramôa CP, Eissenberg T, Sahingur SE (October 2017). "Increasing popularity of waterpipe tobacco smoking and electronic cigarette use: Implications for oral healthcare". Journal of Periodontal Research. 52 (5): 813–823. doi:10.1111/jre.12458. PMC 5585021. PMID 28393367.
- ^ a b c d e f Cooke A, Fergeson J, Bulkhi A, Casale TB (2015). "The Electronic Cigarette: The Good, the Bad, and the Ugly". The Journal of Allergy and Clinical Immunology. In Practice. 3 (4): 498–505. doi:10.1016/j.jaip.2015.05.022. PMID 26164573.
- ^ a b c d Wolff MS, Buckley JP, Engel SM, McConnell RS, Barr DB (April 2017). "Emerging exposures of developmental toxicants". Current Opinion in Pediatrics. 29 (2): 218–224. doi:10.1097/MOP.0000000000000455. PMC 5473289. PMID 28059904.
- ^ a b c d e Zare S, Nemati M, Zheng Y (2018). "A systematic review of consumer preference for e-cigarette attributes: Flavor, nicotine strength, and type". PLOS ONE. 13 (3): e0194145. Bibcode:2018PLoSO..1394145Z. doi:10.1371/journal.pone.0194145. PMC 5854347. PMID 29543907.
 This article incorporates text available under the CC BY 4.0 license.
This article incorporates text available under the CC BY 4.0 license.
- ^ Naik P, Cucullo L (October 2015). "Pathobiology of tobacco smoking and neurovascular disorders: untied strings and alternative products". Fluids and Barriers of the CNS. 12 (1): 25. doi:10.1186/s12987-015-0022-x. PMC 4628383. PMID 26520792.
- ^ a b c Jankowski M, Brożek G, Lawson J, Skoczyński S, Zejda JE (May 2017). "E-smoking: Emerging public health problem?". International Journal of Occupational Medicine and Environmental Health. 30 (3): 329–344. doi:10.13075/ijomeh.1896.01046. PMID 28481369.
- ^ a b Bonilla A, Blair AJ, Alamro SM, Ward RA, Feldman MB, Dutko RA, et al. (September 2019). "Recurrent spontaneous pneumothoraces and vaping in an 18-year-old man: a case report and review of the literature". Journal of Medical Case Reports. 13 (1): 283. doi:10.1186/s13256-019-2215-4. PMC 6732835. PMID 31495337.
 This article incorporates text available under the CC BY 4.0 license.
This article incorporates text available under the CC BY 4.0 license.
- ^ a b c d Hildick-Smith GJ, Pesko MF, Shearer L, Hughes JM, Chang J, Loughlin GM, et al. (December 2015). "A Practitioner's Guide to Electronic Cigarettes in the Adolescent Population". The Journal of Adolescent Health. 57 (6): 574–579. doi:10.1016/j.jadohealth.2015.07.020. PMID 26422289.
- ^ a b Editorial Staff (7 July 2016). "Popcorn Lung: A Dangerous Risk of Flavored E-Cigarettes". American Lung Association.
- ^ Farsalinos KE, Le Houezec J (2015). "Regulation in the face of uncertainty: the evidence on electronic nicotine delivery systems (e-cigarettes)". Risk Management and Healthcare Policy. 8: 157–167. doi:10.2147/RMHP.S62116. PMC 4598199. PMID 26457058.
- ^ Farsalinos KE, Gillman IG, Hecht SS, Polosa R, Thornburg J (16 November 2016). Analytical Assessment of e-Cigarettes: From Contents to Chemical and Particle Exposure Profiles. Elsevier Science. p. 22. ISBN 978-0-12-811242-7.
- ^ Dhand R (July 2017). "Inhaled Drug Therapy 2016: The Year in Review". Respiratory Care. 62 (7): 978–996. doi:10.4187/respcare.05624. PMID 28559466.
- ^ Huang SJ, Xu YM, Lau AT (June 2018). "Electronic cigarette: A recent update of its toxic effects on humans". Journal of Cellular Physiology. 233 (6): 4466–4478. doi:10.1002/jcp.26352. PMID 29215738. S2CID 3556795.
- ^ Zborovskaya Y (February 2017). "E-Cigarettes and Smoking Cessation: A Primer for Oncology Clinicians". Clinical Journal of Oncology Nursing. 21 (1): 54–63. doi:10.1188/17.CJON.54-63. PMID 28107337. S2CID 206992720.
- ^ a b Born H, Persky M, Kraus DH, Peng R, Amin MR, Branski RC (July 2015). "Electronic Cigarettes: A Primer for Clinicians". Otolaryngology–Head and Neck Surgery. 153 (1): 5–14. doi:10.1177/0194599815585752. PMID 26002957. S2CID 10199442.
- ^ Detailed reference list is located on a separate image page.
- ^ Vij K (2014). Textbook of Forensic Medicine & Toxicology: Principles & Practice (5th ed.). Elsevier Health Sciences. p. 525. ISBN 978-81-312-3623-9. Extract of page 525
- ^ "NICOTINE: Systemic Agent". 8 July 2021.
- ^ "Nicotine", Dictionary of Toxicology, Singapore: Springer Nature, p. 691, 2024, doi:10.1007/978-981-99-9283-6_1860, ISBN 978-981-99-9282-9, retrieved 2024-10-19,
Nicotine is a colorless, water-soluble, and extremely hazardous alkaloid. It also has a terrible taste.
- ^ Royal College of Physicians. "Nicotine Without Smoke -- Tobacco Harm Reduction". p. 125. Retrieved 30 September 2020.
Use of nicotine alone, in the doses used by smokers, represents little if any hazard to the user.
- ^ Douglas CE, Henson R, Drope J, Wender RC (July 2018). "The American Cancer Society public health statement on eliminating combustible tobacco use in the United States". CA. 68 (4): 240–245. doi:10.3322/caac.21455. PMID 29889305. S2CID 47016482.
It is the smoke from combustible tobacco products—not nicotine—that injures and kills millions of smokers.
- ^ Dinakar C, O'Connor GT (October 2016). "The Health Effects of Electronic Cigarettes". The New England Journal of Medicine. 375 (14): 1372–1381. doi:10.1056/NEJMra1502466. PMID 27705269.
Beyond its addictive properties, short-term or long-term exposure to nicotine in adults has not been established as dangerous
- ^ a b Hartmann-Boyce J, Chepkin SC, Ye W, Bullen C, Lancaster T (May 2018). "Nicotine replacement therapy versus control for smoking cessation". The Cochrane Database of Systematic Reviews. 5 (5): CD000146. doi:10.1002/14651858.CD000146.pub5. PMC 6353172. PMID 29852054.
- ^ a b c d e f g Cite error: The named reference
Nicotine Cochrane NRT 2018was invoked but never defined (see the help page). - ^ Schraufnagel DE (March 2015). "Electronic Cigarettes: Vulnerability of Youth". Pediatric Allergy, Immunology, and Pulmonology. 28 (1): 2–6. doi:10.1089/ped.2015.0490. PMC 4359356. PMID 25830075.
- ^ England LJ, Bunnell RE, Pechacek TF, Tong VT, McAfee TA (August 2015). "Nicotine and the Developing Human: A Neglected Element in the Electronic Cigarette Debate". American Journal of Preventive Medicine. 49 (2): 286–293. doi:10.1016/j.amepre.2015.01.015. PMC 4594223. PMID 25794473.
- ^ a b c d e f "Nicotine". Drugs.com. American Society of Health-System Pharmacists. Retrieved 24 January 2019.
- ^ "Nicotine Transdermal Patch" (PDF). United States Food and Drug Administration. Retrieved 24 January 2019.
- ^ a b "Nicotrol NS" (PDF). United States Food and Drug Administration. Retrieved 24 January 2019.
- ^ "Nicotrol" (PDF). Pfizer. Retrieved 24 January 2019.
- ^ Marsot A, Simon N (March 2016). "Nicotine and Cotinine Levels With Electronic Cigarette: A Review". International Journal of Toxicology. 35 (2): 179–185. doi:10.1177/1091581815618935. PMID 26681385. S2CID 12969599.
- ^ a b Schivo M, Avdalovic MV, Murin S (February 2014). "Non-cigarette tobacco and the lung". Clinical Reviews in Allergy & Immunology. 46 (1): 34–53. doi:10.1007/s12016-013-8372-0. PMID 23673789. S2CID 23626872.
- ^ Callahan-Lyon P (May 2014). "Electronic cigarettes: human health effects". Tobacco Control. 23 (Supplement 2): ii36 – ii40. doi:10.1136/tobaccocontrol-2013-051470. PMC 3995250. PMID 24732161.
- ^ England LJ, Aagaard K, Bloch M, Conway K, Cosgrove K, Grana R, et al. (January 2017). "Developmental toxicity of nicotine: A transdisciplinary synthesis and implications for emerging tobacco products". Neuroscience and Biobehavioral Reviews. 72: 176–189. doi:10.1016/j.neubiorev.2016.11.013. PMC 5965681. PMID 27890689.
- ^ a b Offermann F (June 2014). "The Hazards of E-Cigarettes". ASHRAE Journal. 56 (6).[permanent dead link]
- ^ a b Bourke L, Bauld L, Bullen C, Cumberbatch M, Giovannucci E, Islami F, et al. (June 2017). "E-cigarettes and Urologic Health: A Collaborative Review of Toxicology, Epidemiology, and Potential Risks". European Urology. 71 (6): 915–923. doi:10.1016/j.eururo.2016.12.022. hdl:1893/24937. PMID 28073600.
- ^ Kaur G, Pinkston R, Mclemore B, Dorsey WC, Batra S (March 2018). "Immunological and toxicological risk assessment of e-cigarettes". European Respiratory Review. 27 (147): 170119. doi:10.1183/16000617.0119-2017. PMC 9489161. PMID 29491036.
- ^ Crowley RA (April 2015). "Electronic nicotine delivery systems: executive summary of a policy position paper from the American College of Physicians". Annals of Internal Medicine. 162 (8): 583–584. doi:10.7326/M14-2481. PMID 25894027. S2CID 207538290.
- ^ Kleinstreuer C, Feng Y (September 2013). "Lung deposition analyses of inhaled toxic aerosols in conventional and less harmful cigarette smoke: a review". International Journal of Environmental Research and Public Health. 10 (9): 4454–4485. doi:10.3390/ijerph10094454. PMC 3799535. PMID 24065038.
- ^ Jia-You G, Ghosh M, Hoet P (October 2023). "Association between metal exposure from e-cigarette components and toxicity endpoints: A literature review". Regulatory Toxicology and Pharmacology. 144 (105488). doi:10.1016/j.yrtph.2023.105488. PMID 37657743.
- ^ Schroeder MJ, Hoffman AC (May 2014). "Electronic cigarettes and nicotine clinical pharmacology". Tobacco Control. 23 (Supplement 2): ii30 – ii35. doi:10.1136/tobaccocontrol-2013-051469. PMC 3995273. PMID 24732160.
- ^ Benowitz NL, Burbank AD (August 2016). "Cardiovascular toxicity of nicotine: Implications for electronic cigarette use". Trends in Cardiovascular Medicine. 26 (6): 515–523. doi:10.1016/j.tcm.2016.03.001. PMC 4958544. PMID 27079891.
- ^ Di Matteo V, Pierucci M, Di Giovanni G, Benigno A, Esposito E (2007). "The neurobiological bases for the pharmacotherapy of nicotine addiction". Current Pharmaceutical Design. 13 (12): 1269–1284. doi:10.2174/138161207780618920. PMID 17504235.
- ^ a b c d e f "Electronic Cigarettes (E-cigarettes)". National Institute on Drug Abuse. March 2018.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ Mishra A, Chaturvedi P, Datta S, Sinukumar S, Joshi P, Garg A (2015). "Harmful effects of nicotine". Indian Journal of Medical and Paediatric Oncology. 36 (1): 24–31. doi:10.4103/0971-5851.151771. PMC 4363846. PMID 25810571.
- ^ "FDA's Plan for Tobacco and Nicotine Regulation". United States Food and Drug Administration. 15 March 2018.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ CDC (2024-05-20). "E-Cigarettes and Pregnancy". Maternal Infant Health. Retrieved 2024-07-31.
- ^ a b c d e "E-cigarettes (Vaping)", Mother To Baby | Fact Sheets, Brentwood (TN): Organization of Teratology Information Specialists (OTIS), 1994, PMID 35951787, retrieved 2024-07-30
- ^ Hajek P, Przulj D, Pesola F, Griffiths C, Walton R, McRobbie H, et al. (May 2022). "Electronic cigarettes versus nicotine patches for smoking cessation in pregnancy: a randomized controlled trial". Nature Medicine. 28 (5): 958–964. doi:10.1038/s41591-022-01808-0. ISSN 1546-170X. PMC 9117131. PMID 35577966.
- ^ "Tobacco Smoking Cessation in Adults, Including Pregnant Persons: Interventions". U.S. Preventative Services Task Force. January 19, 2021. Retrieved July 31, 2024.
- ^ Carroll Chapman SL, Wu LT (July 2014). "E-cigarette prevalence and correlates of use among adolescents versus adults: a review and comparison". Journal of Psychiatric Research. 54: 43–54. doi:10.1016/j.jpsychires.2014.03.005. PMC 4055566. PMID 24680203.
- ^ Schraufnagel DE, Blasi F, Drummond MB, Lam DC, Latif E, Rosen MJ, et al. (September 2014). "Electronic cigarettes. A position statement of the forum of international respiratory societies". American Journal of Respiratory and Critical Care Medicine. 190 (6): 611–618. doi:10.1164/rccm.201407-1198PP. PMID 25006874. S2CID 43763340.
- ^ Chen IL, Todd I, Fairclough LC (September 2019). "Immunological and pathological effects of electronic cigarettes". Basic & Clinical Pharmacology & Toxicology. 125 (3): 237–252. doi:10.1111/bcpt.13225. PMID 30861614.
- ^ a b Sapru S, Vardhan M, Li Q, Guo Y, Li X, Saxena D (October 2020). "E-cigarettes use in the United States: reasons for use, perceptions, and effects on health". BMC Public Health. 20 (1): 1518. doi:10.1186/s12889-020-09572-x. PMC 7545933. PMID 33032554.
- ^ Schneider S, Diehl K (May 2016). "Vaping as a Catalyst for Smoking? An Initial Model on the Initiation of Electronic Cigarette Use and the Transition to Tobacco Smoking Among Adolescents". Nicotine & Tobacco Research. 18 (5): 647–653. doi:10.1093/ntr/ntv193. PMID 26386472.
- ^ Perikleous EP, Steiropoulos P, Paraskakis E, Constantinidis TC, Nena E (2018). "E-Cigarette Use Among Adolescents: An Overview of the Literature and Future Perspectives". Frontiers in Public Health. 6: 86. doi:10.3389/fpubh.2018.00086. PMC 5879739. PMID 29632856.
 This article incorporates text by Evanthia P. Perikleous, Paschalis Steiropoulos, Emmanouil Paraskakis, Theodoros C. Constantinidis, and Evangelia Nena available under the CC BY 4.0 license.
This article incorporates text by Evanthia P. Perikleous, Paschalis Steiropoulos, Emmanouil Paraskakis, Theodoros C. Constantinidis, and Evangelia Nena available under the CC BY 4.0 license.
- ^ McCubbin A, Fallin-Bennett A, Barnett J, Ashford K (February 2017). "Perceptions and use of electronic cigarettes in pregnancy". Health Education Research. 32 (1): 22–32. doi:10.1093/her/cyw059. PMC 5914445. PMID 28158490.
- ^ a b McCausland K, Maycock B, Leaver T, Jancey J (February 2019). "The Messages Presented in Electronic Cigarette-Related Social Media Promotions and Discussion: Scoping Review". Journal of Medical Internet Research. 21 (2): e11953. doi:10.2196/11953. PMC 6379814. PMID 30720440.
 This article incorporates text by Kahlia McCausland, Bruce Maycock, Tama Leaver, and Jonine Jancey available under the CC BY 4.0 license.
This article incorporates text by Kahlia McCausland, Bruce Maycock, Tama Leaver, and Jonine Jancey available under the CC BY 4.0 license.
- ^ a b c "Electronic cigarette use among smokers slows as perceptions of harm increase". ASH UK. 22 May 2015.
- ^ Fracol M, Dorfman R, Janes L, Kulkarni S, Bethke K, Hansen N, et al. (November 2017). "The Surgical Impact of E-Cigarettes: A Case Report and Review of the Current Literature". Archives of Plastic Surgery. 44 (6): 477–481. doi:10.5999/aps.2017.00087. PMC 5801784. PMID 29069879.
- ^ Camenga DR, Klein JD (July 2016). "Tobacco Use Disorders". Child and Adolescent Psychiatric Clinics of North America. 25 (3): 445–460. doi:10.1016/j.chc.2016.02.003. PMC 4920978. PMID 27338966.
- ^ Correa JB, Ariel I, Menzie NS, Brandon TH (February 2017). "Documenting the emergence of electronic nicotine delivery systems as a disruptive technology in nicotine and tobacco science". Addictive Behaviors. 65: 179–184. doi:10.1016/j.addbeh.2016.10.021. PMC 5140675. PMID 27816664.
- ^ McKee M (November 2014). "Electronic cigarettes: peering through the smokescreen". Postgraduate Medical Journal. 90 (1069): 607–609. doi:10.1136/postgradmedj-2014-133029. PMID 25294933.
- ^ a b de Andrade M, Angus K, Hastings G (September 2016). "Teenage perceptions of electronic cigarettes in Scottish tobacco-education school interventions: co-production and innovative engagement through a pop-up radio project". Perspectives in Public Health. 136 (5): 288–293. doi:10.1177/1757913915612109. PMID 26543156. S2CID 3792825.
- ^ Tomashefski A (September 2016). "The perceived effects of electronic cigarettes on health by adult users: A state of the science systematic literature review". Journal of the American Association of Nurse Practitioners. 28 (9): 510–515. doi:10.1002/2327-6924.12358. PMID 26997487. S2CID 42900184.
- ^ Wagener TL, Meier E, Tackett AP, Matheny JD, Pechacek TF (May 2016). "A Proposed Collaboration Against Big Tobacco: Common Ground Between the Vaping and Public Health Community in the United States". Nicotine & Tobacco Research. 18 (5): 730–736. doi:10.1093/ntr/ntv241. PMC 6959509. PMID 26508399.
- ^ Collins L, Glasser AM, Abudayyeh H, Pearson JL, Villanti AC (January 2019). "E-Cigarette Marketing and Communication: How E-Cigarette Companies Market E-Cigarettes and the Public Engages with E-cigarette Information". Nicotine & Tobacco Research. 21 (1): 14–24. doi:10.1093/ntr/ntx284. PMC 6610165. PMID 29315420.
- ^ a b Aly AS, Mamikutty R, Marhazlinda J (2022-10-31). "Association between Harmful and Addictive Perceptions of E-Cigarettes and E-Cigarette Use among Adolescents and Youth—A Systematic Review and Meta-Analysis". Children. 9 (11): 1678. doi:10.3390/children9111678. ISSN 2227-9067. PMC 9689130. PMID 36360406.
- ^ Products Cf (2024-06-26). "Results from the Annual National Youth Tobacco Survey". FDA.
- ^ Kelsh S, Ottney A, Young M, Kelly M, Larson R, Sohn M (2023-03-07). "Young Adults' Electronic Cigarette Use and Perceptions of Risk". Tobacco Use Insights. 16: 1179173X231161313. doi:10.1177/1179173X231161313. ISSN 1179-173X. PMC 9996725. PMID 36911177.
External links
[edit] Media related to Electronic cigarettes at Wikimedia Commons
Media related to Electronic cigarettes at Wikimedia Commons


