Alcoholic liver disease
| Alcoholic liver disease | |
|---|---|
| Other names | Alcohol-related liver disease |
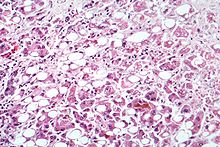 | |
| Microscopy of liver showing fatty change, cell necrosis, Mallory bodies | |
| Specialty | Gastroenterology |
Alcoholic liver disease (ALD), also called alcohol-related liver disease (ARLD), is a term that encompasses the liver manifestations of alcohol overconsumption, including fatty liver, alcoholic hepatitis, and chronic hepatitis with liver fibrosis or cirrhosis.[1]
It is the major cause of liver disease in Western countries, and is the leading cause of death from excessive drinking.[2][3] Although steatosis (fatty liver disease) will develop in any individual who consumes a large quantity of alcoholic beverages over a long period of time, this process is transient and reversible.[1] More than 90% of all heavy drinkers develop fatty liver whilst about 25% develop the more severe alcoholic hepatitis, and 15% liver cirrhosis.[4]
For patients with chronic hepatitis B, a strict adherence to abstinence is highly recommended.[5]
Presentation
[edit]This section is empty. You can help by adding to it. (December 2024) |
Risk factors
[edit]Risk factors known as of 2010 are:
- Quantity of alcohol taken: Consumption of 60–80 g per day (14 g is considered one standard drink in the US, e.g. 1+1⁄2 US fl oz or 44 mL hard liquor, 5 US fl oz or 150 mL wine, 12 US fl oz or 350 mL beer; drinking a six-pack of 5% ABV beer daily would be 84 g and just over the upper limit) for 20 years or more in men, or 20 g/day for women significantly increases the risk of hepatitis and fibrosis by 6% to 41%.[1][6]
- Pattern of drinking: Drinking outside of meal times increases up to 3 times the risk of alcoholic liver disease.[7]
- Sex: Women are twice as susceptible to alcohol-related liver disease, and may develop alcoholic liver disease with shorter durations and doses of chronic consumption. The lesser amount of alcohol dehydrogenase secreted in the gut, higher proportion of body fat in women, and changes in alcohol absorption due to the menstrual cycle may explain this phenomenon.[1][7]
- Ethnicity: Higher rates of alcohol-related liver disease, unrelated to differences in amounts of alcohol consumed, are seen in African-American and Hispanic males compared to Caucasian males.[1]
- Hepatitis C infection: A concomitant hepatitis C infection significantly accelerates the process of liver injury.[7]
- Genetic factors: Genetic factors predispose both to alcoholism and to alcoholic liver disease. Both monozygotic twins are more likely to be alcoholics and to develop liver cirrhosis than both dizygotic twins. Polymorphisms in the enzymes involved in the metabolism of alcohol, such as ADH, ALDH, CYP4502E1, mitochondrial dysfunction, and cytokine polymorphism may partly explain this genetic component. However, no specific polymorphisms have currently been firmly linked to alcoholic liver disease.[1]
- Iron overload (hemochromatosis).[1]
- Diet: Malnutrition, particularly vitamin A and E deficiencies, can worsen alcohol-induced liver damage by preventing regeneration of hepatocytes. This is particularly a concern as alcoholics are usually malnourished because of a poor diet, anorexia, and encephalopathy.[7]
Pathophysiology
[edit]
The mechanism of ALD is not completely understood. 80% of alcohol passes through the liver to be detoxified. Chronic consumption of alcohol results in the secretion of pro-inflammatory cytokines (TNF-alpha, interleukin 6 and interleukin 8), oxidative stress, lipid peroxidation, and acetaldehyde toxicity. These factors cause inflammation, apoptosis and eventually fibrosis of liver cells. Why this occurs in only a few individuals is still unclear. Additionally, the liver has tremendous capacity to regenerate and even when 75% of hepatocytes are dead, it continues to function as normal.[8][failed verification]
Fatty change
[edit]Fatty change, or steatosis, is the accumulation of fatty acids in liver cells. This can be seen as fatty globules under the microscope. Alcoholism causes development of large fatty globules (macro-vesicular steatosis) throughout the liver and can begin to occur after a few days of heavy drinking.[9] Alcohol is metabolized by alcohol dehydrogenase (ADH) into acetaldehyde, then further metabolized by aldehyde dehydrogenase (ALDH) into acetic acid, which is finally oxidized into carbon dioxide (CO2) and water (H2O).[10] This process generates NADH, and increases the NADH/NAD+ ratio. A higher NADH concentration induces fatty acid synthesis while a decreased NAD level results in decreased fatty acid oxidation. Subsequently, the higher levels of fatty acids signal the liver cells to compound it to glycerol to form triglycerides. These triglycerides accumulate, resulting in fatty liver.[citation needed]
Alcoholic hepatitis
[edit]Alcoholic hepatitis is characterized by the inflammation of hepatocytes. Between 10% and 35% of heavy drinkers develop alcoholic hepatitis (NIAAA, 1993). While development of hepatitis is not directly related to the dose of alcohol, some people seem more prone to this reaction than others. This is called alcoholic steato-necrosis and the inflammation appears to predispose to liver fibrosis. Inflammatory cytokines (TNF-alpha, IL-6 and IL-8) are thought to be essential in the initiation and perpetuation of liver injury and cytotoxic hepatomegaly by inducing apoptosis and severe hepatotoxicity. One possible mechanism for the increased activity of TNF-α is the increased intestinal permeability due to liver disease. This facilitates the absorption of the gut-produced endotoxin into the portal circulation. The Kupffer cells of the liver then phagocytose endotoxin, stimulating the release of TNF-α. TNF-α then triggers apoptotic pathways through the activation of caspases, resulting in cell death.[7]
Cirrhosis
[edit]Cirrhosis is a late stage of serious liver disease marked by inflammation (swelling), fibrosis (cellular hardening) and damaged membranes preventing detoxification of chemicals in the body, ending in scarring and necrosis (cell death).[11] Between 10% and 20% of heavy drinkers will develop cirrhosis of the liver (NIAAA, 1993). Acetaldehyde may be responsible for alcohol-induced fibrosis by stimulating collagen deposition by hepatic stellate cells.[7] The production of oxidants derived from NADPH oxi- dase and/or cytochrome P-450 2E1 and the formation of acetaldehyde-protein adducts damage the cell membrane.[7] Symptoms include jaundice (yellowing), liver enlargement, and pain and tenderness from the structural changes in damaged liver architecture. Without total abstinence from alcohol use, cirrhosis will eventually lead to liver failure. Late complications of cirrhosis or liver failure include portal hypertension (high blood pressure in the portal vein due to the increased flow resistance through the damaged liver), coagulation disorders (due to impaired production of coagulation factors), ascites (heavy abdominal swelling due to buildup of fluids in the tissues) and other complications, including hepatic encephalopathy and the hepatorenal syndrome. Cirrhosis can also result from other causes than hazardous alcohol use, such as viral hepatitis and heavy exposure to toxins other than alcohol. The late stages of cirrhosis may look similar medically, regardless of cause. This phenomenon is termed the "final common pathway" for the disease. Fatty change and alcoholic hepatitis with abstinence can be reversible. The later stages of fibrosis and cirrhosis tend to be irreversible, but can usually be contained with abstinence for long periods of time.[citation needed]
Diagnosis
[edit]In the early stages, patients with ALD exhibit subtle and often no abnormal physical findings. It is usually not until development of advanced liver disease that stigmata of chronic liver disease become apparent. Early ALD is usually discovered during routine health examinations when liver enzyme levels are found to be elevated. These usually reflect alcoholic hepatic steatosis. Microvesicular and macrovesicular steatosis with inflammation are seen in liver biopsy specimens. These histologic features of ALD are indistinguishable from those of nonalcoholic fatty liver disease. Steatosis usually resolves after discontinuation of alcohol use. Continuation of alcohol use will result in a higher risk of progression of liver disease and cirrhosis. In patients with acute alcoholic hepatitis, clinical manifestations include fever, jaundice, hepatomegaly, and possible hepatic decompensation with hepatic encephalopathy, variceal bleeding, and ascites accumulation. Tender hepatomegaly may be present, but abdominal pain is unusual. Occasionally, the patient may be asymptomatic.[12]
Laboratory findings
[edit]In people with alcoholic hepatitis, the serum aspartate aminotransferase (AST) to alanine aminotransferase (ALT) ratio is greater than 2:1. AST and ALT levels are almost always less than 500. The elevated AST to ALT ratio is due to deficiency of pyridoxal phosphate, which is required in the ALT enzyme synthetic pathway. Furthermore, alcohol metabolite–induced injury of hepatic mitochondria results in AST isoenzyme release. Other laboratory findings include red blood cell macrocytosis (mean corpuscular volume > 100) and elevations of serum gamma-glutamyl transferase (GGT), alkaline phosphatase, and bilirubin levels. Folate level is reduced in alcoholic patients due to decreased intestinal absorption, increased bone marrow requirement for folate in the presence of alcohol, and increased urinary loss. The magnitude of leukocytopenia (white blood cell depletion) reflects severity of liver injury. Histologic features include Mallory bodies, giant mitochondria, hepatocyte necrosis, and neutrophil infiltration in the area around the veins. Mallory bodies, which are also present in other liver diseases, are condensations of cytokeratin components in the hepatocyte cytoplasm and do not contribute to liver injury. Up to 70% of patients with moderate to severe alcoholic hepatitis already have cirrhosis identifiable on biopsy examination at the time of diagnosis.[13]
Treatment
[edit]Not drinking further alcohol is the most important part of treatment.[14] People with chronic HCV infection should abstain from any alcohol intake, due to the risk for rapid acceleration of liver disease.[13]
Medications
[edit]A 2006 Cochrane review did not find evidence sufficient for the use of androgenic anabolic steroids.[15] Corticosteroids are sometimes used; however, this is recommended only when severe liver inflammation is present.[14]
Silymarin has been investigated as a possible treatment, with ambiguous results.[16][17][18] One review claimed benefit for S-adenosyl methionine in disease models.[19]
The effects of anti-tumor necrosis factor medications such as infliximab and etanercept are unclear and possibly harmful.[20] Evidence is unclear for pentoxifylline.[14][21] Propylthiouracil may result in harm.[22]
Evidence does not support supplemental nutrition in liver disease.[23]
Transplantation
[edit]Although in rare cases liver cirrhosis is reversible, the disease process remains mostly irreversible. Liver transplantation remains the only definitive therapy. Today, survival after liver transplantation is similar for people with ALD and non-ALD. The requirements for transplant listing are the same as those for other types of liver disease, except for a 6-month sobriety prerequisite along with psychiatric evaluation and rehabilitation assistance.[24][clarification needed] Specific requirements vary among the transplant centers. Relapse to alcohol use after transplant listing results in delisting. Re-listing is possible in many institutions, but only after 3–6 months of sobriety. There are limited data on transplant survival in patients transplanted for acute alcoholic hepatitis, but it is believed to be similar to that in nonacute ALD, non-ALD, and alcoholic hepatitis with MDF less than 32.[25]
Prognosis
[edit]The prognosis for people with ALD depends on the liver histology as well as cofactors, such as concomitant chronic viral hepatitis. Among patients with alcoholic hepatitis, progression to liver cirrhosis occurs at 10–20% per year, and 70% will eventually develop cirrhosis. Despite cessation of alcohol use, only 10% will have normalization of histology and serum liver enzyme levels.[26] As previously noted, the MDF has been used to predict short-term mortality (i.e., MDF ≥ 32 associated with spontaneous survival of 50–65% without corticosteroid therapy, and MDF < 32 associated with spontaneous survival of 90%). The Model for End-Stage Liver Disease (MELD) score has also been found to have similar predictive accuracy in 30-day (MELD > 11) and 90-day (MELD > 21) mortality. Liver cirrhosis develops in 6–14% of those who consume more than 60–80 g of alcohol daily for men and more than 20 g daily for women. Even in those who drink more than 120 g daily, only 13.5% will experience a serious alcohol-related liver injury. Nevertheless, alcohol-related mortality was the third leading cause of death in 2003 in the United States. Worldwide mortality is estimated to be 150,000 per year.[27] Alcoholic liver disease can lead to the development of exocrine pancreatic insufficiency.[28]
References
[edit]- ^ a b c d e f g O'Shea RS, Dasarathy S, McCullough AJ (January 2010). "Alcoholic liver disease: AASLD Practice Guidelines" (PDF). Hepatology. 51 (1): 307–28. doi:10.1002/hep.23258. PMID 20034030. S2CID 41729364. Archived from the original (PDF) on 21 October 2014. Retrieved 18 October 2011.
- ^ Smith, Dana G. (4 March 2024). "The Top Cause of Alcohol-Related Deaths Can Go Undetected for Years". The New York Times. ISSN 0362-4331. Retrieved 6 March 2024.
- ^ "ARDI Alcohol-Attributable Deaths, US | CDC". nccd.cdc.gov. Retrieved 6 March 2024.
- ^ Basra, Sarpreet (2011). "Definition, epidemiology and magnitude of alcoholic hepatitis". World Journal of Hepatology. 3 (5): 108–113. doi:10.4254/wjh.v3.i5.108. PMC 3124876. PMID 21731902.
- ^ Iida-Ueno, A; Enomoto, M; Tamori, A; Kawada, N (21 April 2017). "Hepatitis B virus infection and alcohol consumption". World Journal of Gastroenterology. 23 (15): 2651–2659. doi:10.3748/wjg.v23.i15.2651. PMC 5403744. PMID 28487602.
- ^ Mandayam S, Jamal MM, Morgan TR (August 2004). "Epidemiology of alcoholic liver disease". Semin. Liver Dis. 24 (3): 217–32. CiteSeerX 10.1.1.594.1256. doi:10.1055/s-2004-832936. PMID 15349801. S2CID 46350552.
- ^ a b c d e f g Menon KV, Gores GJ, Shah VH (October 2001). "Pathogenesis, diagnosis, and treatment of alcoholic liver disease". Mayo Clin. Proc. 76 (10): 1021–9. doi:10.4065/76.10.1021. PMID 11605686.
- ^ Longstreth, George F.; Zieve, David, eds. (18 October 2009). "Alcoholic Liver Disease". MedLinePlus: Trusted Health Information for You. Bethesda, MD: US National Library of Medicine & National Institutes of Health. Archived from the original on 22 January 2010. Retrieved 27 January 2010.
- ^ Inaba, Darryl; Cohen, William B. (2004). Uppers, downers, all arounders: physical and mental effects of psychoactive drugs (5th ed.). Ashland, Or: CNS Publications. ISBN 978-0-926544-27-7.
- ^ Inaba & Cohen 2004, p. 185
- ^ Loyd, Dr. Stephen (15 February 2020). "What are the early signs of liver damage?". journeypure.com. Retrieved 11 June 2020.
- ^ McCullough, AJ; O'Connor, JF (November 1998). "Alcoholic liver disease: proposed recommendations for the American College of Gastroenterology". The American Journal of Gastroenterology. 93 (11): 2022–36. doi:10.1111/j.1572-0241.1998.00587.x. PMID 9820369. S2CID 1439776.
- ^ a b Niemelä, O (February 2007). "Biomarkers in alcoholism". Clinica Chimica Acta. 377 (1–2): 39–49. doi:10.1016/j.cca.2006.08.035. PMID 17045579.
- ^ a b c Suk, KT; Kim, MY; Baik, SK (28 September 2014). "Alcoholic liver disease: treatment". World Journal of Gastroenterology. 20 (36): 12934–44. doi:10.3748/wjg.v20.i36.12934. PMC 4177474. PMID 25278689.
- ^ Rambaldi, A; Gluud, C (18 October 2006). "Anabolic-androgenic steroids for alcoholic liver disease". The Cochrane Database of Systematic Reviews. 2009 (4): CD003045. doi:10.1002/14651858.CD003045.pub2. PMC 8690167. PMID 17054157.
- ^ Ferenci P, Dragosics B, Dittrich H, Frank H, Benda L, Lochs H, et al. (1989). "Randomized controlled trial of silymarin treatment in patients with cirrhosis of the liver". J Hepatol. 9 (1): 105–113. doi:10.1016/0168-8278(89)90083-4. PMID 2671116.
- ^ Rambaldi A, Jacobs BP, Iaquinto G, Gluud C (November 2005). "Milk thistle for alcoholic and/or hepatitis B or C liver diseases—a systematic cochrane hepato-biliary group review with meta-analyses of randomized clinical trials". Am. J. Gastroenterol. 100 (11): 2583–91. doi:10.1111/j.1572-0241.2005.00262.x. PMID 16279916. S2CID 11757767.
- ^ Bjelakovic G, Gluud LL, Nikolova D, Bjelakovic M, Nagorni A, Gluud C (2011). Bjelakovic G (ed.). "Antioxidant supplements for liver diseases". Cochrane Database Syst Rev (3): CD007749. doi:10.1002/14651858.CD007749.pub2. PMID 21412909.
- ^ Cederbaum AI, Department of Pharmacology and Systems Therapeutics, Box 1603, Icahn School of Medicine at Mount Sinai, One Gustave Levy Place, New York, NY 10029, United States (March 2010). "Hepatoprotective effects of S -adenosyl-L-methionine against alcohol- and cytochrome P450 2E1-induced liver injury". World J Gastroenterol. 16 (11): 1366–1376. doi:10.3748/wjg.v16.i11.1366. PMC 2842529. PMID 20238404.
- ^ Tilg, H; Day, CP (January 2007). "Management strategies in alcoholic liver disease". Nature Clinical Practice Gastroenterology & Hepatology. 4 (1): 24–34. doi:10.1038/ncpgasthep0683. PMID 17203086. S2CID 22443776.
- ^ Whitfield, K; Rambaldi, A; Wetterslev, J; Gluud, C (7 October 2009). "Pentoxifylline for alcoholic hepatitis". The Cochrane Database of Systematic Reviews. 2009 (4): CD007339. doi:10.1002/14651858.CD007339.pub2. PMC 6769169. PMID 19821406.
- ^ Fede, G; Germani, G; Gluud, C; Gurusamy, KS; Burroughs, AK (15 June 2011). "Propylthiouracil for alcoholic liver disease". The Cochrane Database of Systematic Reviews. 2011 (6): CD002800. doi:10.1002/14651858.CD002800.pub3. PMC 7098215. PMID 21678335.
- ^ Koretz, RL; Avenell, A; Lipman, TO (16 May 2012). "Nutritional support for liver disease". The Cochrane Database of Systematic Reviews. 5 (5): CD008344. doi:10.1002/14651858.CD008344.pub2. PMC 6823271. PMID 22592729.
- ^ Stravitz, R. Todd (2006). "Management of the Cirrhotic Patient Before Liver Transplantation: The Role of the Referring Gastroenterologist". Gastroenterology & Hepatology. 2 (5): 346–354. ISSN 1554-7914. PMC 5338188. PMID 28289338.
- ^ Neuberger, J; Schulz, KH; Day, C; Fleig, W; Berlakovich, GA; Berenguer, M; Pageaux, GP; Lucey, M; Horsmans, Y; Burroughs, A; Hockerstedt, K (January 2002). "Transplantation for alcoholic liver disease". Journal of Hepatology. 36 (1): 130–7. doi:10.1016/s0168-8278(01)00278-1. PMC 1837536. PMID 11804676.
- ^ Dunn, W; Jamil, LH; Brown, LS; Wiesner, RH; Kim, WR; Menon, KV; Malinchoc, M; Kamath, PS; Shah, V (February 2005). "MELD accurately predicts mortality in patients with alcoholic hepatitis". Hepatology. 41 (2): 353–8. doi:10.1002/hep.20503. PMID 15660383. S2CID 27208162.
- ^ Sheth, M; Riggs, M; Patel, T (2002). "Utility of the Mayo End-Stage Liver Disease (MELD) score in assessing prognosis of patients with alcoholic hepatitis". BMC Gastroenterology. 2 (1): 2. doi:10.1186/1471-230X-2-2. PMC 65516. PMID 11835693.
- ^ Leeds, John S.; Oppong, Kofi; Sanders, David S. (July 2011). "The role of fecal elastase-1 in detecting exocrine pancreatic disease". Nature Reviews Gastroenterology & Hepatology. 8 (7): 405–415. doi:10.1038/nrgastro.2011.91. PMID 21629239.
