Calcifediol

| |
| |
| Names | |
|---|---|
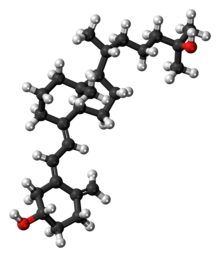
| Preferred IUPAC name
(1S,3Z)-3-[(2E)-2-{(1R,3aS,7aR)-1-[(2R)-6-Hydroxy-6-methylheptan-2-yl]-7a-methyloctahydro-4H-inden-4-ylidene}ethylidene]-4-methylidenecyclohexan-1-ol | |
| Other names | |
| Identifiers | |
3D model (JSmol)
|
|
| ChEBI | |
| ChEMBL | |
| ChemSpider | |
| DrugBank | |
| ECHA InfoCard | 100.039.067 |
| KEGG | |
| MeSH | Calcifediol |
PubChem CID
|
|
| UNII | |
CompTox Dashboard (EPA)
|
|
| |
| |
| Properties | |
| C27H44O2 | |
| Molar mass | 400.64 g/mol |
| Pharmacology | |
| H05BX05 (WHO) | |
| Legal status | |
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa).
| |
Calcifediol, also known as calcidiol, 25-hydroxycholecalciferol, or 25-hydroxyvitamin D3 (abbreviated 25(OH)D3),[1] is a form of vitamin D produced in the liver by hydroxylation of vitamin D3 (cholecalciferol) by the enzyme vitamin D 25-hydroxylase.[3][4][5] Calcifediol can be further hydroxylated by the enzyme 25(OH)D-1α-hydroxylase, primarily in the kidney, to form calcitriol (1,25-(OH)2D3), which is the active hormonal form of vitamin D.[3][4][5]
Calcifediol is strongly bound in blood by the vitamin D-binding protein.[5] Measurement of serum calcifediol is the usual test performed to determine a person's vitamin D status, to show vitamin D deficiency or sufficiency.[4][5] Calcifediol is available as an oral medication in some countries to supplement vitamin D status.[4][6][7]
Biology
[edit]Calcifediol is the precursor for calcitriol, the active form of vitamin D.[3][4] It is synthesized in the liver, by hydroxylation of cholecalciferol (vitamin D3) at the 25-position.[3] This enzymatic 25-hydroxylase reaction is mostly due to the actions of CYP2R1, present in microsomes, although other enzymes such as mitochondrial CYP27A1 can contribute.[5][8] Variations in the expression and activity of CYP2R1, such as low levels in obesity, affect circulating calcifediol.[8] Similarly, vitamin D2, ergocalciferol, can also be 25-hydroxylated to form 25-hydroxyergocalciferol, (ercalcidiol, 25(OH)D2);[1] both forms are measured together in blood as 25(OH)D.[3][4]
At a typical intake of cholecalciferol (up to 2000 IU/day), conversion to calcifediol is rapid. When large doses are given (100,000 IU), it takes 7 days to reach peak calcifediol concentrations.[9] Calcifediol binds in the blood to vitamin D-binding protein (also known as gc-globulin) and is the main circulating vitamin D metabolite.[4][5] Calcifediol has an elimination half-life of around 15 to 30 days.[4][9]
Calcifediol is further hydroxylated at the 1-alpha-position in the kidneys to form 1,25-(OH)2D3, calcitriol.[3][4] This enzymatic 25(OH)D-1α-hydroxylase reaction is performed exclusively by CYP27B1, which is highly expressed in the kidneys where it is principally regulated by parathyroid hormone, but also by FGF23 and calcitriol itself.[3][5][8] CYP27B1 is also expressed in a number of other tissues, including macrophages, monocytes, keratinocytes, placenta and parathyroid gland and extra-renal synthesis of calcitriol from calcifediol has been shown to have biological effects in these tissues.[8][10]
Calcifediol is also converted into 24,25-dihydroxycholecalciferol by 24-hydroxylation.[3] This enzymatic reaction is performed by CYP24A1 which is expressed in many vitamin D target tissues including kidney, and is induced by calcitriol.[5] This will inactivate calcitriol to calcitroic acid, but 24,25-(OH)2D3 may have some biological actions itself.[5]
Blood test for vitamin D deficiency
[edit]In medical practice, a blood test for 25-hydroxy-vitamin D, 25(OH)D, is used to determine an individual's vitamin D status.[11] The name 25(OH)D refers to any combination of calcifediol (25-hydroxy-cholecalciferol), derived from vitamin D3, and ercalcidiol (25-hydroxy-ergocalciferol),[1] derived from vitamin D2. The first of these (also known as 25-hydroxy vitamin D3) is made by the body, or is sourced from certain animal foods or cholecalciferol supplements. The second (25-hydroxy vitamin D2) is from certain vegetable foods or ergocalciferol supplements.[11] Clinical tests for 25(OH)D often measure the total level of both of these two compounds together, generally without differentiating.[12]
This measurement is considered the best indicator of overall vitamin D status.[11][13][14] US labs generally report 25(OH)D levels as ng/mL. Other countries use nmol/L. Multiply ng/mL by 2.5 to convert to nmol/L.[4]
This test can be used to diagnose vitamin D deficiency, and is performed in people with high risk for vitamin D deficiency, when the results of the test can be used to support beginning replacement therapy with vitamin D supplements.[4][15] Patients with osteoporosis, chronic kidney disease, malabsorption, obesity, and some other infections may be at greater risk for being vitamin D-deficient and so are more likely to have this test.[15] Although vitamin D deficiency is common in some populations including those living at higher latitudes or with limited sun exposure, the 25(OH)D test is not usually requested for the entire population.[15] Physicians may advise low risk patients to take over-the-counter vitamin D supplements in place of having screening.[15]
It is the most sensitive measure, though experts have called for improved standardization and reproducibility across different laboratories.[4][13] According to MedlinePlus, the recommended range of 25(OH)D is 20 to 40 ng/mL (50 to 100 nmol/L) though they recognize many experts recommend 30 to 50 ng/mL (75 to 125 nmol/L).[11] The normal range varies widely depending on several factors, including age and geographic location. A broad reference range of 20 to 150 nmol/L (8-60 ng/mL) has also been suggested,[16] while other studies have defined levels below 80 nmol/L (32 ng/mL) as indicative of vitamin D deficiency.[17]
Increasing calcifediol levels up to levels of 80 nmol/L (32 ng/mL) are associated with increasing the fraction of calcium that is absorbed from the gut.[13] Urinary calcium excretion balances intestinal calcium absorption and does not increase with calcifediol levels up to ~400 nmol/L (160 ng/mL).[18]
Supplementation
[edit]Calcifediol supplements have been used in some studies to improve vitamin D status.[4] Indications for their use include vitamin D deficiency or insufficiency, refractory rickets (vitamin D resistant rickets), familial hypophosphatemia, hypoparathyroidism, hypocalcemia and renal osteodystrophy and, with calcium, in primary or corticosteroid-induced osteoporosis.[19]
Calcifediol may have advantages over cholecalciferol for the correction of vitamin D deficiency states.[6] A review of the results of nine randomized control trials which compared oral doses of both, found that calcifediol was 3.2-fold more potent than cholecalciferol.[6] Calcifediol is better absorbed from the intestine and has greater affinity for the vitamin-D-binding protein, both of which increase its bioavailability.[20] Orally administered calcifediol has a much shorter half-life with faster elimination.[20] These properties may be beneficial in people with intestinal malabsorption, obesity, or treated with certain other medications.[20]
In 2016, the FDA approved a formulation of calcifediol (Rayaldee) 60 microgram daily as a prescription medication to treat secondary hyperparathyroidism in patients with chronic kidney disease.[7]
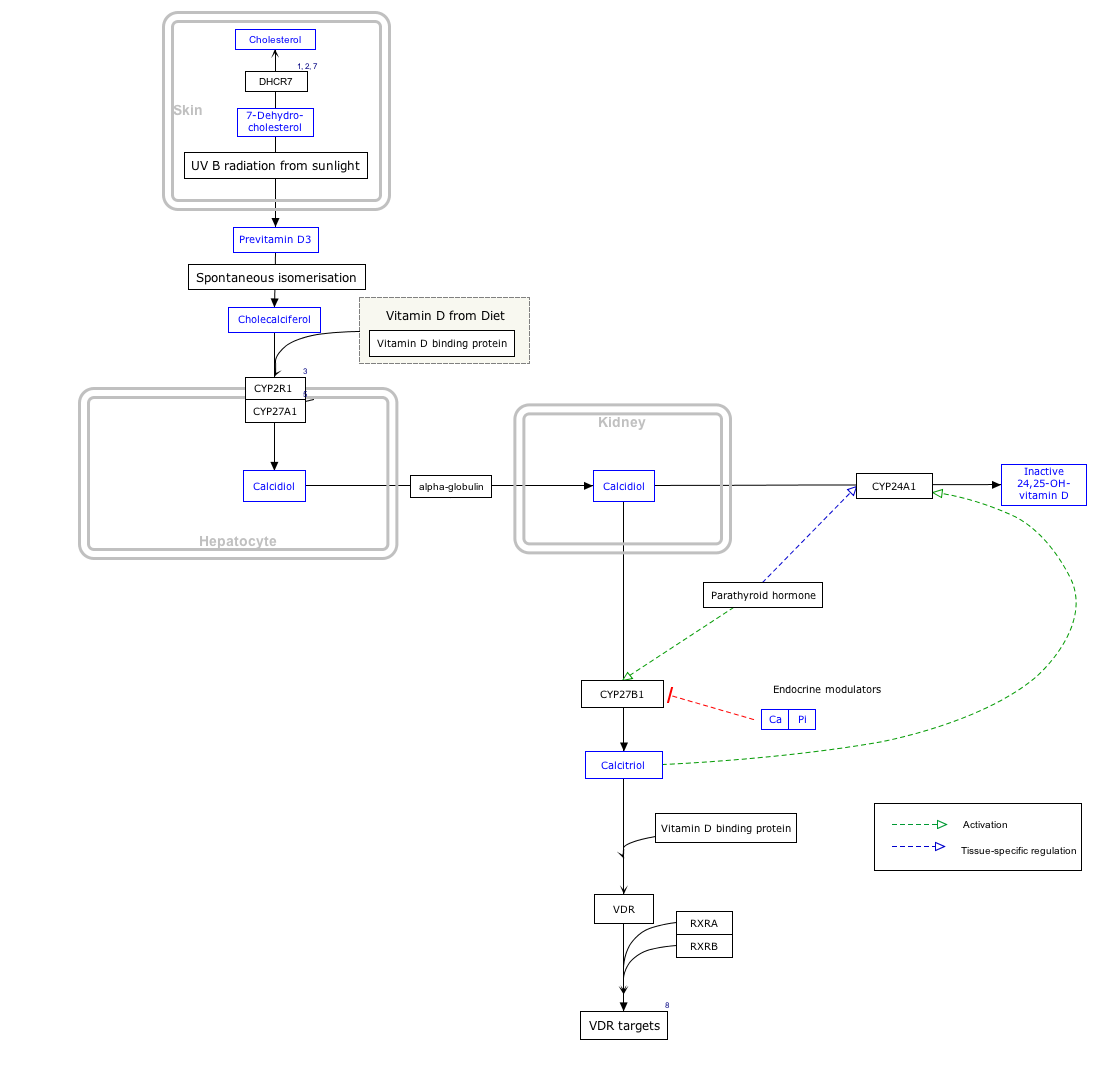
Interactive pathway map
[edit]Click on genes, proteins and metabolites below to link to respective articles. [§ 1]
- ^ The interactive pathway map can be edited at WikiPathways: "VitaminDSynthesis_WP1531".
History
[edit]Research in the laboratory of Hector DeLuca identified 25(OH)D in 1968 and showed that the liver was necessary for its formation.[21] The enzyme responsible for this synthesis, cholecalciferol 25-hydroxylase, was isolated in the same laboratory by Michael F. Holick in 1972.[22]
Research
[edit]Studies are ongoing comparing the effects of calcifediol with other forms of vitamin D including cholecalciferol in prevention and treatment of osteoporosis.[3][20]
Other Organisms
[edit]Teleost Fish
[edit]In teleost fish, calcifediol is predominantly converted to calcitriol in the liver, rather than in the kidneys[23] which means circulating levels of calcifediol can be undetectable and alternative measures of vitamin D status are required. There has been some success in using dietary calcifediol supplementation in salmonids to improve growth and food conversion ratio.[24]
References
[edit]- ^ a b c d "IUPAC-IUB Joint Commission on Biochemical Nomenclature (JCBN): Nomenclature of vitamin D. Recommendations 1981". European Journal of Biochemistry. 124 (2): 223–7. May 1982. doi:10.1111/j.1432-1033.1982.tb06581.x. PMID 7094913.
- ^ "Drug and medical device highlights 2018: Helping you maintain and improve your health". Health Canada. 14 October 2020. Retrieved 17 April 2024.
- ^ a b c d e f g h i "Vitamin D". Micronutrient Information Center, Linus Pauling Institute, Oregon State University, Corvallis. 11 February 2021. Retrieved 14 March 2022.
- ^ a b c d e f g h i j k l m "Office of Dietary Supplements - Vitamin D". ods.od.nih.gov. 9 October 2020. Retrieved 31 October 2020.
- ^ a b c d e f g h i Bikle DD (March 2014). "Vitamin D metabolism, mechanism of action, and clinical applications". Chemistry & Biology. 21 (3): 319–29. doi:10.1016/j.chembiol.2013.12.016. PMC 3968073. PMID 24529992.
- ^ a b c Quesada-Gomez JM, Bouillon R (August 2018). "Is calcifediol better than cholecalciferol for vitamin D supplementation?". Osteoporosis International (review). 29 (8): 1697–1711. doi:10.1007/s00198-018-4520-y. PMID 29713796. S2CID 14005489.
- ^ a b "Rayaldee (calcifediol) FDA Approval History - Drugs.com". Retrieved 4 March 2021.
- ^ a b c d Bouillon R, Bikle D (November 2019). "Vitamin D Metabolism Revised: Fall of Dogmas". Journal of Bone and Mineral Research (Review). 34 (11): 1985–1992. doi:10.1002/jbmr.3884. PMC 9000993. PMID 31589774.
- ^ a b Heaney RP, Armas LA, Shary JR, Bell NH, Binkley N, Hollis BW (June 2008). "25-Hydroxylation of vitamin D3: relation to circulating vitamin D3 under various input conditions". The American Journal of Clinical Nutrition. 87 (6): 1738–42. doi:10.1093/ajcn/87.6.1738. PMID 18541563.
- ^ Adams JS, Hewison M (July 2012). "Extrarenal expression of the 25-hydroxyvitamin D-1-hydroxylase". Arch Biochem Biophys. 523 (1): 95–102. doi:10.1016/j.abb.2012.02.016. PMC 3361592. PMID 22446158.
- ^ a b c d "25-hydroxy vitamin D test: Medline Plus". Retrieved 4 March 2021.
- ^ "25HDN - Clinical: 25-Hydroxyvitamin D2 and D3, Serum". Mayo Clinic Labs. 2021. Retrieved 4 March 2021.
- ^ a b c Heaney RP (December 2004). "Functional indices of vitamin D status and ramifications of vitamin D deficiency". The American Journal of Clinical Nutrition. 80 (6 Suppl): 1706S–9S. doi:10.1093/ajcn/80.6.1706S. PMID 15585791.
- ^ Theodoratou E, Tzoulaki I, Zgaga L, Ioannidis JP (April 2014). "Vitamin D and multiple health outcomes: umbrella review of systematic reviews and meta-analyses of observational studies and randomised trials". BMJ. 348: g2035. doi:10.1136/bmj.g2035. PMC 3972415. PMID 24690624.
- ^ a b c d American Society for Clinical Pathology, "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, American Society for Clinical Pathology, retrieved August 1, 2013, which cites
- Sattar N, Welsh P, Panarelli M, Forouhi NG (January 2012). "Increasing requests for vitamin D measurement: costly, confusing, and without credibility". Lancet. 379 (9811): 95–6. doi:10.1016/S0140-6736(11)61816-3. PMID 22243814. S2CID 12669468.
- Bilinski KL, Boyages SC (July 2012). "The rising cost of vitamin D testing in Australia: time to establish guidelines for testing". The Medical Journal of Australia. 197 (2): 90. doi:10.5694/mja12.10561. PMID 22794049. S2CID 45880893.
- Lu CM (May 2012). "Pathology consultation on vitamin D testing: clinical indications for 25(OH) vitamin D measurement". American Journal of Clinical Pathology. 137 (5). American Society for Clinical Pathology: 831–2. doi:10.1309/ajcp2gp0ghkqrcoe. PMID 22645788., which cites
- Arya SC, Agarwal N (May 2012). "The measurement of vitamin D3 requires maintaining quality control". American Journal of Clinical Pathology. 137 (5): 832, author reply 833. doi:10.1309/AJCP2GP0GHKQRCOE. PMID 22523224.
- Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. (July 2011). "Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline". The Journal of Clinical Endocrinology and Metabolism. 96 (7): 1911–30. doi:10.1210/jc.2011-0385. PMID 21646368.
- ^ Bender DA (2003). "Vitamin D". Nutritional biochemistry of the vitamins. Cambridge: Cambridge University Press. ISBN 978-0-521-80388-5. Retrieved December 10, 2008 through Google Book Search.
- ^ Hollis BW (February 2005). "Circulating 25-hydroxyvitamin D levels indicative of vitamin D sufficiency: implications for establishing a new effective dietary intake recommendation for vitamin D". The Journal of Nutrition. 135 (2): 317–22. doi:10.1093/jn/135.2.317. PMID 15671234.
- ^ Kimball SM, Ursell MR, O'Connor P, Vieth R (September 2007). "Safety of vitamin D3 in adults with multiple sclerosis". The American Journal of Clinical Nutrition. 86 (3): 645–51. doi:10.1093/ajcn/86.3.645. PMID 17823429.
- ^ "Calcifediol". go.drugbank.com. Retrieved 7 March 2021.
- ^ a b c d Cesareo R, Falchetti A, Attanasio R, Tabacco G, Naciu AM, Palermo A (May 2019). "Hypovitaminosis D: Is It Time to Consider the Use of Calcifediol?". Nutrients (Review). 11 (5): 1016. doi:10.3390/nu11051016. PMC 6566727. PMID 31064117.
- ^ Ponchon G, Kennan AL, DeLuca HF (November 1969). ""Activation" of vitamin D by the liver". The Journal of Clinical Investigation. 48 (11): 2032–7. doi:10.1172/JCI106168. PMC 297455. PMID 4310770.
- ^ Holick MF, DeLuca HF, Avioli LV (January 1972). "Isolation and identification of 25-hydroxycholecalciferol from human plasma". Archives of Internal Medicine. 129 (1): 56–61. doi:10.1001/archinte.1972.00320010060005. PMID 4332591.
- ^ Lock, E.-J.; Waagbø, R.; Wendelaar Bonga, S.; Flik, G. (February 2010). "The significance of vitamin D for fish: a review". Aquaculture Nutrition. 16 (1): 100–116. doi:10.1111/j.1365-2095.2009.00722.x.
- ^ Rider, S.; Verlhac-Trichet, V.; Constant, D.; Chenal, E.; Etheve, S.; Riond, B.; Schmidt-Posthaus, H.; Schoop, R. (April 2023). "Calcifediol is a safe and effective metabolite for raising vitamin D status and improving growth and feed conversion in rainbow trout". Aquaculture. 568: 739285. doi:10.1016/j.aquaculture.2023.739285.