Universal health care
Universal health care (also called universal health coverage, universal coverage, or universal care) is a health care system in which all residents of a particular country or region are assured access to health care. It is generally organized around providing either all residents or only those who cannot afford on their own, with either health services or the means to acquire them, with the end goal of improving health outcomes.[1]
Universal healthcare does not imply coverage for all cases and for all people – only that all people have access to healthcare when and where needed without financial hardship. Some universal healthcare systems are government-funded, while others are based on a requirement that all citizens purchase private health insurance. Universal healthcare can be determined by three critical dimensions: who is covered, what services are covered, and how much of the cost is covered.[1] It is described by the World Health Organization as a situation where citizens can access health services without incurring financial hardship.[2] Then-Director General of the WHO Margaret Chan described universal health coverage as the "single most powerful concept that public health has to offer" since it unifies "services and delivers them in a comprehensive and integrated way".[3] One of the goals with universal healthcare is to create a system of protection which provides equality of opportunity for people to enjoy the highest possible level of health.[4] Critics say that universal healthcare leads to longer wait times and worse quality healthcare.[5]
As part of Sustainable Development Goals, United Nations member states have agreed to work toward worldwide universal health coverage by 2030.[6][better source needed] Therefore, the inclusion of the universal health coverage (UHC) within the SDGs targets can be related to the reiterated endorsements operated by the WHO.[7]
History
[edit]| Country | Year |
|---|---|
| 1975 | |
| 1967 | |
| 1957 | |
| 1945 | |
| 1970 | |
| 1988 | |
| 1958 | |
| 1966 | |
| 2009 | |
| 1980 | |
| 1973 | |
| 1972 | |
| 1974 | |
| 1941 | |
| 1983 | |
| 1993 | |
| 1990 | |
| 1977 | |
| 1995 | |
| 1978 | |
| 1938 | |
| 1950 | |
| 1973 | |
| 1980s | |
| 1966 | |
| 1938 | |
| 1912 | |
| 1979 | |
| 1993 | |
| 2019 | |
| 1993 | |
| 1972 | |
| 1988 | |
| 1986 | |
| 1955 | |
| 1994 | |
| 1995 | |
| 2003 | |
| 1971 | |
| 1948 |
The first move towards a national health insurance system was launched in Germany in 1883, with the Sickness Insurance Law. Industrial employers were mandated to provide injury and illness insurance for their low-wage workers, and the system was funded and administered by employees and employers through "sick funds", which were drawn from deductions in workers' wages and from employers' contributions. This social health insurance model, named the Bismarck Model after Prussian Chancellor Otto von Bismarck, was the first form of universal care in modern times.[11] Other countries soon began to follow suit. In the United Kingdom, the National Insurance Act 1911 provided coverage for primary care (but not specialist or hospital care) for wage earners, covering about one-third of the population. The Russian Empire established a similar system in 1912, and other industrialized countries began following suit. By the 1930s, similar systems existed in virtually all of Western and Central Europe. Japan introduced an employee health insurance law in 1927, expanding further upon it in 1935 and 1940. Following the Russian Revolution of 1917, a fully public and centralized health care system was established in Soviet Russia in 1920.[12][13] However, it was not a truly universal system at that point, as rural residents were not covered.
In New Zealand, a universal health care system was created in a series of steps, from 1938 to 1941.[14][15] In Australia, the state of Queensland introduced a free public hospital system in 1946.
Following World War II, universal health care systems began to be set up around the world. On July 5, 1948, the United Kingdom launched its universal National Health Service. Universal health care was next introduced in the Nordic countries of Sweden (1955),[16] Iceland (1956),[17] Norway (1956),[18] Denmark (1961)[19] and Finland (1964).[20] Universal health insurance was introduced in Japan in 1961, and in Canada through stages, starting with the province of Saskatchewan in 1962, followed by the rest of Canada from 1968 to 1972.[14][21] A public healthcare system was introduced in Egypt following the Egyptian revolution of 1952. Centralized public healthcare systems were set up in the Eastern bloc countries. The Soviet Union extended universal health care to its rural residents in 1969.[14][22] Kuwait and Bahrain introduced their universal healthcare systems in 1950 and 1957 respectively (prior to independence).[23] Italy introduced its Servizio Sanitario Nazionale (National Health Service) in 1978. Universal health insurance was implemented in Australia in 1975 with the Medibank, which led to universal coverage under the current Medicare system from 1984.[citation needed]
From the 1970s to the 2000s, Western European countries began introducing universal coverage, most of them building upon previous health insurance programs to cover the whole population. For example, France built upon its 1928 national health insurance system, with subsequent legislation covering a larger and larger percentage of the population, until the remaining 1% of the population that was uninsured received coverage in 2000.[24][25] Single payer healthcare systems were introduced in Finland (1972), Portugal (1979), Cyprus (1980), Spain (1986) and Iceland (1990). Switzerland introduced a universal healthcare system based on an insurance mandate in 1994.[26][23] In addition, universal health coverage was introduced in some Asian countries, including Malaysia (1980s),[27] South Korea (1989), Taiwan (1995), Singapore (1993), Israel (1995) and Thailand (2001).
Following the collapse of the Soviet Union, Russia retained and reformed its universal health care system,[28] as did other now-independent former Soviet republics and Eastern bloc countries.
Beyond the 1990s, many countries in Latin America, the Caribbean, Africa and the Asia-Pacific region, including developing countries, took steps to bring their populations under universal health coverage, including China which has the largest universal health care system in the world[29] and Brazil's SUS[30] which improved coverage up to 80% of the population.[31] India introduced a tax-payer funded decentralised universal healthcare system as well as comprehensive public and private health insurances that helped reduce mortality rates drastically and improved healthcare infrastructure across the country dramatically.[32] A 2012 study examined progress being made by these countries, focusing on nine in particular: Ghana, Rwanda, Nigeria, Mali, Kenya, Indonesia, the Philippines and Vietnam.[33][34]
Currently, most industrialized countries and many developing countries operate some form of publicly funded health care with universal coverage as the goal. According to the National Academy of Medicine and others, the United States is the only wealthy, industrialized nation that does not provide universal health care. The only forms of government-provided healthcare available are Medicare (for elderly patients as well as people with disabilities), Medicaid (for low-income people),[35][36] the Military Health System (active, reserve, and retired military personnel and dependants), and the Indian Health Service (members of federally recognized Native American tribes).
Funding models
[edit]
Universal health care in most countries has been achieved by a mixed model of funding. General taxation revenue is the primary source of funding, but in many countries it is supplemented by specific charge (which may be charged to the individual or an employer) or with the option of private payments (by direct or optional insurance) for services beyond those covered by the public system. Almost all European systems are financed through a mix of public and private contributions.[39] Most universal health care systems are funded primarily by tax revenue (as in Portugal,[39] India, Spain, Denmark and Sweden). Some nations, such as Germany, France,[40] and Japan,[41] employ a multi-payer system in which health care is funded by private and public contributions. However, much of the non-government funding comes from contributions from employers and employees to regulated non-profit sickness funds. Contributions are compulsory and defined according to law. A distinction is also made between municipal and national healthcare funding. For example, one model is that the bulk of the healthcare is funded by the municipality, specialty healthcare is provided and possibly funded by a larger entity, such as a municipal co-operation board or the state, and medications are paid for by a state agency. A paper by Sherry A. Glied from Columbia University found that universal health care systems are modestly redistributive and that the progressivity of health care financing has limited implications for overall income inequality.[42]
Compulsory insurance
[edit]This is usually enforced via legislation requiring residents to purchase insurance, but sometimes the government provides the insurance. Sometimes there may be a choice of multiple public and private funds providing a standard service (as in Germany) or sometimes just a single public fund (as in the Canadian provinces). Healthcare in Switzerland is based on compulsory insurance.[43][44]
In some European countries where private insurance and universal health care coexist, such as Germany, Belgium and the Netherlands, the problem of adverse selection is overcome by using a risk compensation pool to equalize, as far as possible, the risks between funds. Thus, a fund with a predominantly healthy, younger population has to pay into a compensation pool and a fund with an older and predominantly less healthy population would receive funds from the pool. In this way, sickness funds compete on price and there is no advantage in eliminating people with higher risks because they are compensated for by means of risk-adjusted capitation payments. Funds are not allowed to pick and choose their policyholders or deny coverage, but they compete mainly on price and service. In some countries, the basic coverage level is set by the government and cannot be modified.[45]
The Republic of Ireland at one time had a "community rating" system by VHI, effectively a single-payer or common risk pool. The government later opened VHI to competition, but without a compensation pool. That resulted in foreign insurance companies entering the Irish market and offering much less expensive health insurance to relatively healthy segments of the market, which then made higher profits at VHI's expense. The government later reintroduced community rating by a pooling arrangement and at least one main major insurance company, BUPA, withdrew from the Irish market.[citation needed]
In Poland, people are obliged to pay a percentage of the average monthly wage to the state, even if they are covered by private insurance.[46] People working under a employment contract pay a percentage of their wage, while entrepreneurs pay a fixed rate, based on the average national wage. Unemployed people are insured by the labor office.
Among the potential solutions posited by economists are single-payer systems as well as other methods of ensuring that health insurance is universal, such as by requiring all citizens to purchase insurance or by limiting the ability of insurance companies to deny insurance to individuals or vary price between individuals.[47][48]
Single-payer
[edit]Single-payer health care is a system in which the government, rather than private insurers, pays for all health care costs.[49] Single-payer systems may contract for healthcare services from private organizations, or own and employ healthcare resources and personnel (as was the case in England before the introduction of the Health and Social Care Act). In some instances, such as Italy and Spain, both these realities may exist at the same time.[11] "Single-payer" thus describes only the funding mechanism and refers to health care financed by a single public body from a single fund and does not specify the type of delivery or for whom doctors work. Although the fund holder is usually the state, some forms of single-payer use a mixed public-private system.[citation needed]
Tax-based financing
[edit]In tax-based financing, individuals contribute to the provision of health services through various taxes. These are typically pooled across the whole population unless local governments raise and retain tax revenues. Some countries (notably Spain, the United Kingdom, Ireland, New Zealand, Italy, Brazil, Portugal, India and the Nordic countries) choose to fund public health care directly from taxation alone. Other countries with insurance-based systems effectively meet the cost of insuring those unable to insure themselves via social security arrangements funded from taxation, either by directly paying their medical bills or by paying for insurance premiums for those affected.[citation needed]
Social health insurance
[edit]In a social health insurance system, contributions from workers, the self-employed, enterprises and governments are pooled into single or multiple funds on a compulsory basis. This is based on risk pooling.[50] The social health insurance model is also referred to as the Bismarck Model, after Chancellor Otto von Bismarck, who introduced the first universal health care system in Germany in the 19th century.[51] The funds typically contract with a mix of public and private providers for the provision of a specified benefit package. Preventive and public health care may be provided by these funds or responsibility kept solely by the Ministry of Health. Within social health insurance, a number of functions may be executed by parastatal or non-governmental sickness funds, or in a few cases, by private health insurance companies. Social health insurance is used in a number of Western European countries and increasingly in Eastern Europe as well as in Israel and Japan.[52]
Private insurance
[edit]In private health insurance, premiums are paid directly from employers, associations, individuals and families to insurance companies, which pool risks across their membership base. Private insurance includes policies sold by commercial for-profit firms, non-profit companies and community health insurers. Generally, private insurance is voluntary in contrast to social insurance programs, which tend to be compulsory.[53]
In some countries with universal coverage, private insurance often excludes certain health conditions that are expensive and the state health care system can provide coverage. For example, in the United Kingdom, one of the largest private health care providers is BUPA, which has a long list of general exclusions even in its highest coverage policy,[54] most of which are routinely provided by the National Health Service. In the Netherlands, which has regulated competition for its main insurance system (but is subject to a budget cap), insurers must cover a basic package for all enrollees, but may choose which additional services they offer in supplementary plans; which most people possess [citation needed].
The Planning Commission of India has also suggested that the country should embrace insurance to achieve universal health coverage.[55] General tax revenue is currently used to meet the essential health requirements of all people.
Community-based health insurance
[edit]A particular form of private health insurance that has often emerged, if financial risk protection mechanisms have only a limited impact, is community-based health insurance.[56] Individual members of a specific community pay to a collective health fund which they can draw from when they need medical care. Contributions are not risk-related and there is generally a high level of community involvement in the running of these plans. Community-based health insurance generally only play a limited role in helping countries move towards universal health coverage. Challenges includes inequitable access by the poorest[57] that health service utilization of members generally increase after enrollment.[56]
Implementation and comparisons
[edit]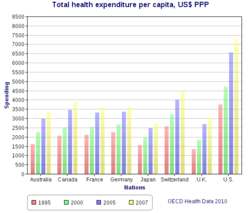
Universal health care systems vary according to the degree of government involvement in providing care or health insurance. In some countries, such as Canada, the UK, Italy, Australia, and the Nordic countries, the government has a high degree of involvement in the commissioning or delivery of health care services and access is based on residence rights, not on the purchase of insurance. Others have a much more pluralistic delivery system, based on obligatory health with contributory insurance rates related to salaries or income and usually funded by employers and beneficiaries jointly.[citation needed]
Sometimes, the health funds are derived from a mixture of insurance premiums, salary-related mandatory contributions by employees or employers to regulated sickness funds, and by government taxes. These insurance based systems tend to reimburse private or public medical providers, often at heavily regulated rates, through mutual or publicly owned medical insurers. A few countries, such as the Netherlands and Switzerland, operate via privately owned but heavily regulated private insurers, which are not allowed to make a profit from the mandatory element of insurance but can profit by selling supplemental insurance.[citation needed]
Universal health care is a broad concept that has been implemented in several ways. The common denominator for all such programs is some form of government action aimed at extending access to health care as widely as possible and setting minimum standards. Most implement universal health care through legislation, regulation, and taxation. Legislation and regulation direct what care must be provided, to whom, and on what basis. Usually, some costs are borne by the patient at the time of consumption, but the bulk of costs come from a combination of compulsory insurance and tax revenues. Some programs are paid for entirely out of tax revenues. In others, tax revenues are used either to fund insurance for the very poor or for those needing long-term chronic care.
A critical concept in the delivery of universal healthcare is that of population healthcare. This is a way of organizing the delivery, and allocating resources, of healthcare (and potentially social care) based on populations in a given geography with a common need (such as asthma, end of life, urgent care). Rather than focus on institutions such as hospitals, primary care, community care etc. the system focuses on the population with a common as a whole. This includes people currently being treated, and those that are not being treated but should be (i.e. where there is health inequity). This approach encourages integrated care and a more effective use of resources.[58]
The United Kingdom National Audit Office in 2003 published an international comparison of ten different health care systems in ten developed countries, nine universal systems against one non-universal system (the United States), and their relative costs and key health outcomes.[59] A wider international comparison of 16 countries, each with universal health care, was published by the World Health Organization in 2004.[60] In some cases, government involvement also includes directly managing the health care system, but many countries use mixed public-private systems to deliver universal health care.
Overview of Health Coverage Reports
[edit]The 2023 report from the WHO and the World Bank indicates that the advancement towards Universal Health Coverage (UHC) by the year 2030 has not progressed since 2015. The UHC Service Coverage Index (SCI) has remained constant at a score of 68 from 2019 to 2021. It is reported that catastrophic out-of-pocket (OOP) health expenditures have impacted over 1 billion individuals globally. Additionally, in the year 2019, it was found that 2 billion people experienced financial difficulties due to health expenses, with ongoing, significant disparities in coverage. The report suggests several strategies to mitigate these challenges: it calls for the acceleration of essential health services, sustained attention to infectious disease management, improvement in health workforce and infrastructure, the elimination of financial barriers to care, an increase in pre-paid and pooled health financing, policy initiatives to curtail OOP expenses, a focus on primary healthcare to reinforce overall health systems, and the fortification of collaborative efforts to achieve UHC. These measures aim to increase health service coverage by an additional 477 million individuals by the year 2023 and to continue progress towards covering an extra billion people by the 2030 deadline.[61][62]
Criticism and support
[edit]This section has multiple issues. Please help improve it or discuss these issues on the talk page. (Learn how and when to remove these messages)
|
Critics of universal healthcare say that it leads to longer wait times and a decrease in the quality of healthcare.[5] Critics of implementing universal healthcare in the United States say that it would require healthy people to pay for the medical care of unhealthy people, which they say goes against the American values of individual choice and personal responsibility; it would raise healthcare expenditures due to the high cost of implementation that the United States government supposedly cannot pay; and represents unnecessary government overreach into the lives of American citizens, healthcare, the health insurance industry, and employers' rights to choose what health coverage they want to offer to their employees.[5]
Most contemporary studies posit that a single payer universal healthcare system would benefit the United States. According to a 2020 study published in The Lancet, the proposed Medicare for All Act would save 68,000 lives and $450 billion in national healthcare expenditure annually.[63] A 2022 study published in the PNAS found that a single-payer universal healthcare system would have saved 212,000 lives and averted over $100 billion in medical costs during the COVID-19 pandemic in the United States in 2020 alone.[64]
See also
[edit]- Acronyms in healthcare
- Cultural competence in health care
- Euro Health Consumer Index
- Global health
- Health care
- Health promotion
- Health law
- Health insurance cooperative
- Health spending as a percent of GDP by country (gross domestic product)
- Healthcare reform debate in the United States
- List of countries by health insurance coverage
- List of countries by total health expenditure per capita
- List of countries with universal health care
- National health insurance
- Primary healthcare
- Public health
- Publicly funded health care
- Right to health
- Single-payer healthcare
- Socialized medicine
- Two-tier healthcare
- Universal Health Coverage Day
References
[edit]- ^ a b World Health Organization (November 22, 2010). The world health report: health systems financing: the path to universal coverage. Geneva: World Health Organization. ISBN 978-92-4-156402-1. Archived from the original on August 20, 2010. Retrieved April 11, 2012.
- ^ "Universal health coverage (UHC)". Retrieved November 30, 2016.
- ^ Matheson, Don * (January 1, 2015). "Will Universal Health Coverage (UHC) Lead to the Freedom to Lead Flourishing and Healthy Lives? Comment on "Inequities in the Freedom to Lead a Flourishing and Healthy Life: Issues for Healthy Public Policy"". International Journal of Health Policy and Management. 4 (1): 49–51. doi:10.15171/ijhpm.2015.09. PMC 4289038. PMID 25584354.
- ^ Abiiro, Gilbert Abotisem; De Allegri, Manuela (July 4, 2015). "Universal health coverage from multiple perspectives: a synthesis of conceptual literature and global debates". BMC International Health and Human Rights. 15: 17. doi:10.1186/s12914-015-0056-9. ISSN 1472-698X. PMC 4491257. PMID 26141806.
- ^ a b c "Universal Health Care Topic Overview". Gale. 2019. Retrieved May 9, 2022.
- ^ "Universal health coverage (UHC)". World Health Organization. December 12, 2016. Retrieved September 14, 2017.
- ^ {{cite web Greco, S., Putans, R., & Springe, L. (2022). Antimicrobial and antibiotic resistance in developing countries: Health economics, global governance, and sustainable development goals. In Antimicrobial Resistance: Collaborative Measures of Control (pp. 113-140). CRC Press. https://doi.org/10.1201/9781003313175}}
- ^ Foreign Countries with Universal Health Care. By New York State Department of Health.
- ^ "Chapter 5. Reorganizing the Health Care System in Brazil: International Development Research Centre". February 11, 2008. Archived from the original on February 11, 2008.
- ^ Atun R (2015). "Transforming Turkey's Health System--Lessons for Universal Coverage". N Engl J Med. 373 (14): 1285–9. doi:10.1056/NEJMp1410433. PMID 26422719.
- ^ a b Butticè, Claudio (2019). Universal Health Care. Santa Barbara, California: Greenwood Publishing Group. pp. 20, 25. ISBN 978-1-4408-6844-3.
- ^ Rowland, Diane; Telyukov, Alexandre V. (Fall 1991). "Soviet Healthcare From Two Perspectives" (PDF). Health Affairs. 10 (3): 71–86. doi:10.1377/hlthaff.10.3.71. PMID 1748393.
- ^ "OECD Reviews of Health Systems OECD Reviews of Health Systems: Russian Federation 2012": 38.
{{cite journal}}: Cite journal requires|journal=(help) - ^ a b c Abel-Smith, Brian (1987). "Social welfare; Social security; Benefits in kind; National health schemes". The new Encyclopædia Britannica (15th ed.). Chicago: Encyclopædia Britannica. ISBN 978-0-85229-443-7. Retrieved September 30, 2013.
- ^ Richards, Raymond (1993). "Two Social Security Acts". Closing the door to destitution: the shaping of the Social Security Acts of the United States and New Zealand. University Park: Pennsylvania State University Press. p. 14. ISBN 978-0-271-02665-7. Retrieved March 11, 2013.
Mein Smith, Philippa (2012). "Making New Zealand 1930–1949". A concise history of New Zealand (2nd ed.). Cambridge: Cambridge University Press. pp. 164–65. ISBN 978-1-107-40217-1. Retrieved March 11, 2013. - ^ Serner, Uncas (1980). "Swedish health legislation: milestones in reorganisation since 1945". In Heidenheimer, Arnold J.; Elvander, Nils; Hultén, Charly (eds.). The shaping of the Swedish health system. New York: St. Martin's Press. p. 103. ISBN 978-0-312-71627-1.
Universal and comprehensive health insurance was debated at intervals all through the Second World War, and in 1946 such a bill was voted in Parliament. For financial and other reasons, its promulgation was delayed until 1955, at which time coverage was extended to include drugs and sickness compensation, as well.
- ^ Kuhnle, Stein; Hort, Sven E.O. (September 1, 2004). "The developmental welfare state in Scandinavia: lessons to the developing world". Geneva: United Nations Research Institute for Social Development. p. 7. Retrieved March 11, 2013.
- ^ Evang, Karl (1970). Health services in Norway. English version by Dorothy Burton Skårdal (3rd ed.). Oslo: Norwegian Joint Committee on International Social Policy. p. 23. OCLC 141033.
Since 2 July 1956 the entire population of Norway has been included under the obligatory health national insurance program.
- ^ Gannik, Dorte; Holst, Erik; Wagner, Mardsen (1976). "Primary health care". The national health system in Denmark. DHEW publication ; no. (NIH) 77-673. Bethesda: National Institutes of Health. pp. 43–44. hdl:2027/pur1.32754081249264.
- ^ Alestalo, Matti; Uusitalo, Hannu (1987). "Finland". In Flora, Peter (ed.). Growth to limits: the Western European welfare states since World War II, Vol. 4 Appendix (synopses, bibliographies, tables). Berlin: Walter de Gruyter. pp. 137–40. ISBN 978-3-11-011133-0. Retrieved March 11, 2013.
- ^ Taylor, Malcolm G. (1990). "Saskatchewan medical care insurance". Insuring national health care: the Canadian experience. Chapel Hill: University of North Carolina Press. pp. 96–130. ISBN 978-0-8078-1934-0.
Maioni, Antonia (1998). "The 1960s: the political battle". Parting at the crossroads: the emergence of health insurance in the United States and Canada. Princeton: Princeton University Press. pp. 121–22. ISBN 978-0-691-05796-5. Retrieved September 30, 2013. - ^ Kaser, Michael (1976). "The USSR". Health care in the Soviet Union and Eastern Europe. Boulder, Colo.: Westview Press. pp. 38–39, 43. ISBN 978-0-89158-604-3.
Roemer, Milton Irwin (1993). "Social security for medical care". National health systems of the world: Volume II: The issues. Oxford: Oxford University Press. p. 94. ISBN 978-0-19-507845-9. Retrieved September 30, 2013.
Denisova, Liubov N. (2010). "Protection of childhood and motherhood in the countryside". In Mukhina, Irina (ed.). Rural women in the Soviet Union and post-Soviet Russia. New York: Routledge. p. 167. ISBN 978-0-203-84684-1. Retrieved September 30, 2013. - ^ a b Perrin, Karen (Kay) M. (September 8, 2016). Principles of Health Navigation. Jones & Bartlett Publishers. ISBN 978-1-284-09076-5.
- ^ "Austerity and the Unraveling of European Universal Health Care". Dissent Magazine. Retrieved November 30, 2016.
- ^ Bärnighausen, Till; Sauerborn, Rainer (May 2002). "One hundred and eighteen years of the German health insurance system: are there any lessons for middle- and low-income countries?". Social Science & Medicine. 54 (10): 1559–87. doi:10.1016/S0277-9536(01)00137-X. PMID 12061488.
Busse, Reinhard; Riesberg, Annette (2004). "Germany" (PDF). Health Care Systems in Transition. 6 (9). ISSN 1020-9077. Archived from the original (PDF) on March 21, 2020. Retrieved October 8, 2013.
Carrin, Guy; James, Chris (January 2005). "Social health insurance: key factors affecting the transition towards universal coverage" (PDF). International Social Security Review. 58 (1): 45–64. doi:10.1111/j.1468-246X.2005.00209.x. S2CID 154659524. Retrieved October 8, 2013.
Hassenteufel, Patrick; Palier, Bruno (December 2007). "Towards neo-Bismarckian health care states? Comparing health insurance reforms in Bismarckian welfare systems" (PDF). Social Policy & Administration. 41 (6): 574–96. doi:10.1111/j.1467-9515.2007.00573.x. Archived from the original (PDF) on April 12, 2019. Retrieved October 8, 2013.
Green, David; Irvine, Benedict; Clarke, Emily; Bidgood, Elliot (January 23, 2013). "Healthcare systems: Germany" (PDF). London: Civitas. Archived from the original (PDF) on October 5, 2013. Retrieved October 8, 2013. - ^ Hilmy, Ashraf A. (November 14, 2012). Health-Care Reform: A Surgeon'S Perspective. iUniverse. ISBN 978-1-4759-5231-5.
- ^ Savedoff, W and Smith, A. Achieving Universal Health Coverage: Learning from Chile, Japan, Malaysia and Sweden. Working paper of the Results for Development Institute, 2011.
- ^ "WHO - Rocky road from the Semashko to a new health model". Archived from the original on October 18, 2014. Retrieved November 30, 2016.
- ^ Yu, Hao (2015). "Universal health insurance coverage for 1.3 billion people: What accounts for China's success?". Health Policy. 119 (9): 1145–52. doi:10.1016/j.healthpol.2015.07.008. PMC 7114832. PMID 26251322.
- ^ Gómez, Eduardo J. (July 13, 2012). "In Brazil, health care is a right". CNN. Retrieved August 20, 2018.
- ^ Muzaka, Valbona (2017). "Lessons from Brazil: on the difficulties of building a universal health care system". Journal of Global Health. 7 (1): 010303. doi:10.7189/jogh.07.010303. ISSN 2047-2978. PMC 5344008. PMID 28382207.
- ^ "India | Commonwealth Fund". June 5, 2020.
- ^ Eagle, William (September 20, 2012). "Developing Countries Strive to Provide Universal Health Care". Retrieved November 30, 2016.
- ^ "Universal Healthcare on the rise in Latin America". Retrieved November 30, 2016.
- ^ Insuring America's Health: Principles and Recommendations Archived 2007-08-18 at the Wayback Machine, Institute of Medicine at the National Academies of Science, 2004-01-14, accessed 2007-10-22
- ^ "The Case for Universal Health Care in the United States". cthealth.server101.com. Archived from the original on April 23, 2018. Retrieved April 27, 2018.
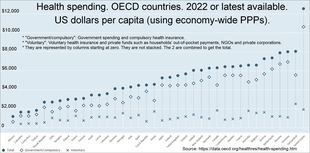
- ^ a b OECD Data. Health resources - Health spending. doi:10.1787/8643de7e-en. 2 bar charts: For both: From bottom menus: Countries menu > choose OECD. Check box for "latest data available". Perspectives menu > Check box to "compare variables". Then check the boxes for government/compulsory, voluntary, and total. Click top tab for chart (bar chart). For GDP chart choose "% of GDP" from bottom menu. For per capita chart choose "US dollars/per capita". Click fullscreen button above chart. Click "print screen" key. Click top tab for table, to see data.
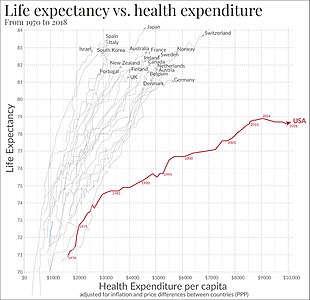
- ^ Link between health spending and life expectancy: US is an outlier. May 26, 2017. By Max Roser at Our World in Data. Click the sources tab under the chart for info on the countries, healthcare expenditures, and data sources. See the later version of the chart here.
- ^ a b Bentes, Margarida; Dias, Carlos Matias; Sakellarides, Sakellarides; Bankauskaite, Vaida (2004). "Health care systems in transition: Portugal" (PDF). Copenhagen: WHO Regional Office for Europe on behalf of the European Observatory on Health Systems and Policies. Archived from the original (PDF) on January 26, 2010. Retrieved August 30, 2006.
- ^ Physicians for a National Health Program (2004). "International health systems". Chicago: Physicians for a National Health Program. Retrieved November 7, 2006.
- ^ Chua, Kao-Ping (February 10, 2006). "Single payer 101" (PDF). Sterling, Virginia: American Medical Student Association. Archived from the original (PDF) on October 24, 2006. Retrieved November 7, 2006.
- ^ Glied, Sherry A. (March 2008). "Health Care Financing, Efficiency and Equity". NBER Working Paper No. 13881. doi:10.3386/w13881.
- ^ Tomasky, Michael (March 21, 2010). "Healthcare vote: Barack Obama passes US health reform by narrow margin". Michael Tomasky's blog. London: The Guardian. Retrieved March 23, 2010.
- ^ Roy, Avik. "Switzerland – a case study in consumer driven health care". Forbes.
- ^ Varkevisser, Marco; van der Geest, Stéphanie (2002). "Competition among social health insurers: a case study for the Netherlands, Belgium and Germany" (PDF). Research in Healthcare Financial Management. 7 (1): 65–84. Archived from the original (PDF) on May 16, 2013. Retrieved November 28, 2007.
- ^ "Ubezpieczenie dobrowolne". NFZ. January 22, 2024. Archived from the original on December 4, 2023.
- ^ Rothschild, Michael; Stiglitz, Joseph (November 1976). "Equilibrium in competitive insurance markets: an essay on the economics of imperfect information" (PDF). Quarterly Journal of Economics. 90 (4): 629–49. doi:10.2307/1885326. JSTOR 1885326. Archived from the original (PDF) on October 20, 2017. Retrieved March 20, 2007.
- ^ Belli, Paolo (March 2001). "How adverse election affects the health insurance market. Policy Research Working Paper 2574" (PDF). Washington, D.C.: World Bank. Retrieved March 20, 2007.
- ^ "single-payer", Merriam Webster Dictionary.
- ^ "Social Health Insurance Report of a Regional Expert Group Meeting" (PDF). World Health Organization Regional Office for South-East Asia. June 2003. Archived from the original (PDF) on March 18, 2017. Retrieved January 17, 2022.
- ^ "Health Care Systems - Four Basic Models". Physicians for a National Health Program. Archived from the original on February 13, 2024.
- ^ Saltman, Richard B.; Busse, Reinhard; Figueras, Josep (eds.). "Social health insurance systems in western Europe" (PDF). World Health Organization. Archived from the original (PDF) on March 31, 2022.
- ^ "Health financing mechanisms: private health insurance". Geneva: World Health Organization. Archived from the original on October 9, 2010. Retrieved April 11, 2012.
- ^ "Health and life cover: Health care select 1: Key features of this health insurance plan: What's covered? What's not covered?". London: Bupa. Archived from the original on April 9, 2010. Retrieved April 11, 2010.
- ^ Varshney, Vibha; Gupta, Alok; Pallavi, Aparna (September 30, 2012). "Universal health scare". Down To Earth. New Delhi: Society for Environmental Communications. Archived from the original on September 20, 2012. Retrieved September 25, 2012.
- ^ a b "Community based health insurance". www.who.int. Retrieved March 24, 2022.
- ^ Umeh, Chukwuemeka A.; Feeley, Frank G. (June 27, 2017). "Inequitable Access to Health Care by the Poor in Community-Based Health Insurance Programs: A Review of Studies From Low- and Middle-Income Countries". Global Health: Science and Practice. 5 (2): 299–314. doi:10.9745/GHSP-D-16-00286. ISSN 2169-575X. PMC 5487091. PMID 28655804.
- ^ Gray, M.; Pitini, E.; Kelley, T.; Bacon, N. (2017). "Managing population healthcare". Journal of the Royal Society of Medicine. 110 (11): 434–439. doi:10.1177/0141076817721099. PMC 5728616. PMID 29148874.
- ^ National Audit Office (February 1, 2003). "International health comparisons: a compendium of published information on healthcare systems, the provision of health care and health achievement in 10 countries". London: National Audit Office. Retrieved November 7, 2007.
- ^ Grosse-Tebbe, Susanne; Figueras, Josep (2004). "Snapshots of health systems: the state of affairs in 16 countries in summer 2004" (PDF). Copenhagen: World Health Organization on behalf of the European Observatory on Health Systems and Policies. Archived from the original (PDF) on September 26, 2007. Retrieved November 7, 2007.
- ^ "Tracking Universal Health Coverage: 2023 Global Monitoring Report". Tracking Universal Health Coverage. September 18, 2023. doi:10.1596/40348.
- ^ “World Health Organization; World Bank. 2023. Tracking Universal Health Coverage: 2023 Global Monitoring Report. © Washington, DC: World Bank. http://hdl.handle.net/10986/40348 License: CC BY-NC-SA 3.0 IGO.”
- ^ Galvani, Alison P; Parpia, Alyssa S; Foster, Eric M; Singer, Burton H; Fitzpatrick, Meagan C (February 13, 2020). "Improving the prognosis of health care in the USA". The Lancet. 395 (10223): 524–533. doi:10.1016/S0140-6736(19)33019-3. PMC 8572548. PMID 32061298. S2CID 211105345.
- ^ Galvani, Alison P.; Parpia, Alyssa S.; et al. (2022). "Universal healthcare as pandemic preparedness: The lives and costs that could have been saved during the COVID-19 pandemic". PNAS. 119 (25): e2200536119. Bibcode:2022PNAS..11900536G. doi:10.1073/pnas.2200536119. PMC 9231482. PMID 35696578. S2CID 249645274.
External links
[edit] Media related to Universal healthcare at Wikimedia Commons
Media related to Universal healthcare at Wikimedia Commons- WHO fact sheet on universal health coverage
- Achieving Universal Health Care (July 2011). MEDICC Review: International Journal of Cuban Health and Medicine 13 (3). Theme issue: authors from 19 countries on dimensions of the challenges of providing universal access to health care.
- Catalyzing Change: The System Reform Costs of Universal Health Coverage (November 15, 2010). New York: The Rockefeller Foundation. Report on the feasibility of establishing the systems and institutions needed to pursue UHC.
- Physicians for a National Health Program Chicago: PNHP. A group of physicians and health professionals who support single-payer reform.
- Primary health care, World Health Organization
- UHC Forward Washington, D.C.: Results for Development Institute. Portal on universal health coverage.
- Percentage of population covered under national health programs , selected countries , 1955 and 1970
- Information on health coverage in various countries in the 1970s and in the 1980s
- "Unmet health care needs statistics", - Statistics Explained eurostat
- "Health at a Glance: Europe 2018: State of Health in the EU Cycle", OECD
- Countries with social security programs in operation, January 1, 1955, by type of program and date of legislation
