Malnutrition
| Malnutrition | |
|---|---|
 | |
| Underfed child in Dolo Ado, Ethiopia, at an MSF treatment tent | |
| Specialty | Critical care medicine |
| Symptoms | Problems with physical or mental development; poor energy levels; hair loss; swollen legs and abdomen[1][2] |
| Causes | Eating a diet with too few or too many nutrients; malabsorption[3][4] |
| Risk factors | Lack of breastfeeding; gastroenteritis; pneumonia; malaria; measles; poverty; homelessness[5] |
| Prevention | Improving agricultural practices; reducing poverty; improving sanitation; education |
| Treatment | Improved nutrition; supplementation; ready-to-use therapeutic foods; treating the underlying cause[6][7][8] |
| Medication | Eating food with enough nutrients on a near daily basis |
| Frequency | 821 million undernourished / 11% of the population (2017)[9] |
| Deaths | 406,000 from nutritional deficiencies (2015)[10] |
Malnutrition occurs when an organism gets too few or too many nutrients, resulting in health problems.[11][12] Specifically, it is a deficiency, excess, or imbalance of energy, protein and other nutrients which adversely affects the body's tissues and form.[13]
Malnutrition is a category of diseases that includes undernutrition and overnutrition.[14] Undernutrition is a lack of nutrients, which can result in stunted growth, wasting, and underweight.[15] A surplus of nutrients causes overnutrition, which can result in obesity. In some developing countries, overnutrition in the form of obesity is beginning to appear within the same communities as undernutrition.[16]
Most clinical studies use the term 'malnutrition' to refer to undernutrition. However, the use of 'malnutrition' instead of 'undernutrition' makes it impossible to distinguish between undernutrition and overnutrition, a less acknowledged form of malnutrition.[13][17] Accordingly, a 2019 report by The Lancet Commission suggested expanding the definition of malnutrition to include "all its forms, including obesity, undernutrition, and other dietary risks."[18] The World Health Organization[19] and The Lancet Commission have also identified "[t]he double burden of malnutrition", which occurs from "the coexistence of overnutrition (overweight and obesity) alongside undernutrition (stunted growth and wasting)."[20][21]
Prevalence
[edit]
It is estimated that nearly one in three persons globally has at least one form of malnutrition: wasting, stunting, vitamin or mineral deficiency, overweight, obesity, or diet-related noncommunicable diseases.[22] Undernutrition is more common in developing countries.[23] Stunting is more prevalent in urban slums than in rural areas.[24] Studies on malnutrition have the population categorised into different groups including infants, under-five children, children, adolescents, pregnant women, adults and the elderly population. The use of different growth references in different studies leads to variances in the undernutrition prevalence reported in different studies. Some of the growth references used in studies include the National Center for Health Statistics (NCHS) growth charts, WHO reference 2007, Centers for Disease Control and Prevention (CDC) growth charts, National Health and Nutrition Examination Survey (NHANES), WHO reference 1995, Obesity Task Force (IOTF) criteria and Indian Academy of Pediatrics (IAP) growth charts.[25]
In children
[edit]The prevalence of undernutrition is highest among children under five.[24] In 2021, 148.1 million children under five years old were stunted, 45 million were wasted, and 37 million were overweight or obese.[26] The same year, an estimated 45% of deaths in children were linked to undernutrition.[26][5] As of 2020[update], the prevalence of wasting among children under five in South Asia was reported to be 16% moderately or severely wasted.[24] As of 2022[update], UNICEF reported this prevalence as having slightly improved, but still being at 14.8%.[27] In Asia, India has one of the highest burden of wasting with over 20% wasted children.[28] However, the burden of undernutrition among under-five children in African countries is much higher. A pooled analysis of the prevalence of chronic undernutrition among under-five children in East Africa was identified to be 33.3%. This prevalence of undernutrition among under-five children ranged from 21.9% in Kenya to 53% in Burundi.[29] In Tanzania, the prevalence of stunting, among children under five varied from 41% in lowland and 64.5% in highland areas. Undernutrition by underweight and wasting was 11.5% and 2.5% in lowland and 22.% and 1.4% in the highland areas of Tanzania respectively.[30] In South Sudan, the prevalence of undernutrition explained by stunting, underweight and wasting in under-five children were 23.8%, 4.8% and 2.3% respectively.[31] In 28 countries, at least 30% of children were still affected by stunting in 2022.[32]
Vitamin A deficiency affects one third of children under age 5 around the world,[33] leading to 670,000 deaths and 250,000–500,000 cases of blindness.[34] Vitamin A supplementation has been shown to reduce all-cause mortality by 12 to 24%.[35]
In adults
[edit]As of June 2021, 1.9 billion adults were overweight or obese, and 462 million adults were underweight.[26] Globally, two billion people had iodine deficiency in 2017.[36] In 2020, 900 million women and children had anemia, which is often caused by iron deficiency.[37] More than 3.1 billion people in the world – 42% – were unable to afford a healthy diet in 2021.[38]
Certain groups have higher rates of undernutrition, including elderly people and women (in particular while pregnant or breastfeeding children under five years of age). Undernutrition is an increasing health problem in people aged over 65 years, even in developed countries, especially among nursing home residents and in acute care hospitals.[39] In the elderly, undernutrition is more commonly due to physical, psychological, and social factors, not a lack of food.[40] Age-related reduced dietary intake due to chewing and swallowing problems, sensory decline, depression, imbalanced gut microbiome, poverty and loneliness are major contributors to undernutrition in the elderly population. Malnutrition is also attributed due to wrong diet plan adopted by people who aim to reduce their weight without medical practitioners or nutritionist advice.[41]
Increase in 2020
[edit]
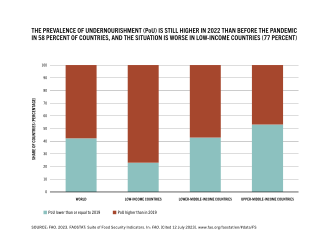
There has been a global increase in food insecurity and hunger between 2011 and 2020. In 2015, 795 million people (about one in ten people on earth) had undernutrition.[9][42] It is estimated that between 691 and 783 million people in the world faced hunger in 2022.[43] According to UNICEF, 2.4 billion people were moderately or severely food insecure in 2022, 391 million more than in 2019.[44]
These increases are partially related to the ongoing COVID-19 pandemic, which continues to highlight the weaknesses of current food and health systems. It has contributed to food insecurity, increasing hunger worldwide; meanwhile, lower physical activity during lockdowns has contributed to increases in overweight and obesity.[45] In 2020, experts estimated that by the end of the year, the pandemic could have double the number of people at risk of suffering acute hunger.[46] Similarly, experts estimated that the prevalence of moderate and severe wasting could increase by 14% due to COVID-19; coupled with reductions in nutrition and health services coverage, this could result in over 128,000 additional deaths among children under 5 in 2020 alone.[45] Although COVID-19 is less severe in children than in adults, the risk of severe disease increases with undernutrition.[47]
Other major causes of hunger include manmade conflicts, climate changes, and economic downturns.[48]
Type
[edit]| External videos | |
|---|---|
Undernutrition
[edit]
Undernutrition can occur either due to protein-energy wasting or as a result of micronutrient deficiencies.[2][49][26][1][3][50][51] It adversely affects physical and mental functioning, and causes changes in body composition and body cell mass.[52][53] Undernutrition is a major health problem, causing the highest mortality rate in children, particularly in those under 5 years, and is responsible for long-lasting physiologic effects.[54] It is a barrier to the complete physical and mental development of children.[51]
Undernutrition can manifest as stunting, wasting, and underweight. If undernutrition occurs during pregnancy, or before two years of age, it may result in permanent problems with physical and mental development.[1][50] Extreme undernutrition can cause starvation, chronic hunger, Severe Acute Malnutrition (SAM), and/or Moderate Acute Malnutrition (MAM).
The signs and symptoms of micronutrient deficiencies depend on which micronutrient is lacking.[2] However, undernourished people are often thin and short, with very poor energy levels; and swelling in the legs and abdomen is also common.[1][2][50] People who are undernourished often get infections and frequently feel cold.[2]
Micronutrient undernutrition
[edit]Micronutrient undernutrition results from insufficient intake of vitamins and minerals.[26] Worldwide, deficiencies in iodine, Vitamin A, and iron are the most common. Children and pregnant women in low-income countries are at especially high risk for micronutrient deficiencies.[26][50]
Anemia is most commonly caused by iron deficiency, but can also result from other micronutrient deficiencies and diseases. This condition can have major health consequences.[55]
It is possible to have overnutrition simultaneously with micronutrient deficiencies; this condition is termed the double burden of malnutrition.
Protein-energy malnutrition
[edit]'Undernutrition' sometimes refers specifically to protein–energy malnutrition (PEM).[2][56] This condition involves both micronutrient deficiencies and an imbalance of protein intake and energy expenditure.[49] It differs from calorie restriction in that calorie restriction may not result in negative health effects. Hypoalimentation (underfeeding) is one cause of undernutrition.[57]
Two forms of PEM are kwashiorkor and marasmus; both commonly coexist.[11]

Kwashiorkor is primarily caused by inadequate protein intake.[11] Its symptoms include edema, wasting, liver enlargement, hypoalbuminaemia, and steatosis; the condition may also cause depigmentation of skin and hair.[11] The disorder is further identified by a characteristic swelling of the belly, and extremities which disguises the patient's undernourished condition.[58] 'Kwashiorkor' means 'displaced child' and is derived from the Ga language of coastal Ghana in West Africa. It means "the sickness the baby gets when the next baby is born," as it often occurs when the older child is deprived of breastfeeding and weaned to a diet composed largely of carbohydrates.[59]
Marasmus (meaning 'to waste away') can result from a sustained diet that is deficient in both protein and energy. This causes their metabolism to adapt to prolong survival.[11] The primary symptoms are severe wasting, leaving little or no edema; minimal subcutaneous fat; and abnormal serum albumin levels.[11] It is traditionally seen in cases of famine, significant food restriction, or severe anorexia.[11] Conditions are characterized by extreme wasting of the muscles and a gaunt expression.[58]
Overnutrition
[edit]Excessive consumption of energy-dense foods and drinks and limited physical activity causes overnutrition.[60] It causes overweight, defined as a body mass index (BMI) of 25 or more, and can lead to obesity (a BMI of 30 or more).[26][2] Obesity has become a major health issue worldwide.[61] Overnutrition is linked to chronic non-communicable diseases like diabetes, certain cancers, and cardiovascular diseases. Hence identifying and addressing the immediate risk factors has become a major health priority.[62] The recent evidence on the impact of diet-induced obesity in fathers and mothers around the time of conception is identified to negatively program the health outcomes of multiple generations.[63]
According to UNICEF, at least 1 in every 10 children under five is overweight in 33 countries.[64]
Classifying malnutrition
[edit]Definition by Gomez and Galvan
[edit]In 1956, Gómez and Galvan studied factors associated with death in a group of undernourished children in a hospital in Mexico City, Mexico. They defined three categories of malnutrition: first, second, and third degree.[65] The degree of malnutrition is calculated based on a child's body size compared to the median weight for their age.[66] The risk of death increases with increasing degrees of malnutrition.[65]
An adaptation of Gomez's original classification is still used today. While it provides a way to compare malnutrition within and between populations, this classification system has been criticized for being "arbitrary" and for not considering overweight as a form of malnutrition. Also, height alone may not be the best indicator of malnutrition; children who are born prematurely may be considered short for their age even if they have good nutrition.[67]
| Degree of PEM | % of desired body weight for age and sex | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Normal | 90–100% | ||||||||||||||
| Mild: Grade I (1st degree) | 75–89% | ||||||||||||||
| Moderate: Grade II (2nd degree) | 60–74% | ||||||||||||||
| Severe: Grade III (3rd degree) | <60% | ||||||||||||||
| SOURCE:"Serum Total Protein and Albumin Levels in Different Grades of Protein Energy Malnutrition"[58] | |||||||||||||||
Definition by Waterlow
[edit]In the 1970s, John Conrad Waterlow established a new classification system for malnutrition.[68] Instead of using just weight for age measurements, Waterlow's system combines weight-for-height (indicating acute episodes of malnutrition) with height-for-age to show the stunting that results from chronic malnutrition.[69] One advantage of the Waterlow classification is that weight for height can be calculated even if a child's age is unknown.[68]
| Degree of PEM | Stunting (%) Height for age | Wasting (%) Weight for height | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Normal: Grade 0 | >95% | >90% | |||||||||||||
| Mild: Grade I | 87.5–95% | 80–90% | |||||||||||||
| Moderate: Grade II | 80–87.5% | 70–80% | |||||||||||||
| Severe: Grade III | <80% | <70% | |||||||||||||
| SOURCE: "Classification and definition of protein-calorie malnutrition." by Waterlow, 1972[68] | |||||||||||||||
The World Health Organization frequently uses these classifications of malnutrition, with some modifications.[66]
Effects
[edit]
Undernutrition weakens every part of the immune system.[70] Protein and energy undernutrition increases susceptibility to infection; so do deficiencies of specific micronutrients (including iron, zinc, and vitamins).[70] In communities or areas that lack access to safe drinking water, these additional health risks present a critical problem.[citation needed]
Undernutrition plays a major role in the onset of active tuberculosis.[71] It also raises the risk of HIV transmission from mother to child, and increases replication of the virus.[70] Undernutrition can cause vitamin-deficiency-related diseases like scurvy and rickets. As undernutrition worsens, those affected have less energy and experience impairment in brain functions. This can make it difficult (or impossible) for them to perform the tasks needed to acquire food, earn an income, or gain an education.[citation needed]
Undernutrition can also cause acute problems, like hypoglycemia (low blood sugar). This condition can cause lethargy, limpness, seizures, and loss of consciousness. Children are particularly at risk and can become hypoglycemic after 4 to 6 hours without food. Dehydration can also occur in malnourished people, and can be life-threatening, especially in babies and small children.[citation needed]
Signs
[edit]There are many different signs of dehydration in undernourished people. These can include sunken eyes; a very dry mouth; decreased urine output and/or dark urine; increased heart rate with decreasing blood pressure; and altered mental status.
| Site | Sign | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Face | Moon face (in kwashiorkor); shrunken, monkey-like face (in marasmus) | ||||||||||||||
| Eye | Dry eyes; pale conjunctiva; periorbital edema; Bitot's spots (in vitamin A deficiency) | ||||||||||||||
| Mouth | Angular stomatitis; cheilitis; glossitis; parotid enlargement; spongy, bleeding gums (in vitamin C and B12 deficiencies) | ||||||||||||||
| Teeth | Enamel mottling; delayed eruption | ||||||||||||||
| Hair | Dull, sparse, brittle hair, with thinning of the hair follicles; hypopigmentation; flag sign (alternating bands of light and normal color); broomstick eyelashes; alopecia | ||||||||||||||
| Skin | Dry skin; follicular hyperkeratosis; patchy hyper- and hypopigmentation; erosions; poor wound healing; loose and wrinkled skin (in marasmus); shiny and edematous skin (in kwashiorkor) | ||||||||||||||
| Nail | Koilonychia; thin and soft nail plates; fissures or ridges | ||||||||||||||
| Musculature | Muscle wasting, particularly in the buttocks and thighs | ||||||||||||||
| Skeletal | Deformities, usually resulting from deficiencies in calcium, vitamin D, or vitamin C | ||||||||||||||
| Abdomen | Distended; hepatomegaly with fatty liver; possible ascites | ||||||||||||||
| Cardiovascular | Bradycardia; hypotension; reduced cardiac output; small vessel vasculopathy | ||||||||||||||
| Neurologic | Global developmental delay; loss of knee and ankle reflexes; poor memory, often resulting from deficiencies in vitamin B12 and other B vitamins | ||||||||||||||
| Hematological | Pallor; petechiae; bleeding diathesis | ||||||||||||||
| Behavior | Lethargic; apathetic; anxious | ||||||||||||||
| Source: "Protein Energy Malnutrition"[66] | |||||||||||||||
Cognitive development
[edit]Protein-calorie malnutrition can cause cognitive impairments. This most commonly occurs in people who were malnourished during a "critical period ... from the final third of gestation to the first 2 years of life".[72] For example, in children under two years of age, iron deficiency anemia is likely to affect brain function acutely, and probably also chronically. Similarly, folate deficiency has been linked to neural tube defects.[73]
Iodine deficiency is "the most common preventable cause of mental impairment worldwide."[74][75] "Even moderate [iodine] deficiency, especially in pregnant women and infants, lowers intelligence by 10 to 15 I.Q. points, shaving incalculable potential off a nation's development."[74] Among those affected, very few people experience the most visible and severe effects: disabling goiters, cretinism and dwarfism. These effects occur most commonly in mountain villages. However, 16 percent of the world's people have at least mild goiter (a swollen thyroid gland in the neck)."[74][76]
Causes and risk factors
[edit]
Social and political
[edit]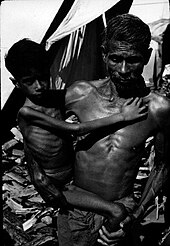
Social conditions have a significant influence on the health of people.[77] The social determinants of undernutrition mainly include poor education, poverty, disease burden and lack of women's empowerment.[78] Identifying and addressing these determinants can eliminate undernutrition in the long term.[78] Identification of the social conditions that causes malnutrition in children under five has received significant research attention as it is a major public health problem.[citation needed]
Undernutrition most commonly results from a lack of access to high-quality, nutritious food.[5] The household income is a socio-economic variable that influences the access to nutritious food and the probability of under and overnutrition in a community.[79] In the study by Ghattas et al. (2020), the probability of overnutrition is significantly higher in higher-income families than in disadvantaged families.[21] High food prices is a major factor preventing low income households from getting nutritious food[1][5] For example, Khan and Kraemer (2009) found that in Bangladesh, low socioeconomic status was associated with chronic malnutrition since it inhibited purchase of nutritious foods (like milk, meat, poultry, and fruits).[80] Food shortages may also contribute to malnutritions in countries which lack technology. However, in the developing world, eighty percent of malnourished children live in countries that produce food surpluses, according to estimates from the Food and Agriculture Organization (FAO).[81] The economist Amartya Sen observes that, in recent decades, famine has always been a problem of food distribution, purchasing power, and/or poverty, since there has always been enough food for everyone in the world.[82]
There are also sociopolitical causes of malnutrition. For example, the population of a community might be at increased risk for malnutrition if government is poor and the area lacks health-related services. On a smaller scale, certain households or individuals may be at an even higher risk due to differences in income levels, access to land, or levels of education.[83] Community plays a crucial role in addressing the social causes of malnutrition.[84] For example, communities with high social support and knowledge sharing about social protection programs can enable better public service demands.[85] Better public service demands and social protection programs minimise the risk of malnutrition in these communities.
It is argued that commodity speculators are increasing the cost of food. As the real-estate bubble in the United States was collapsing, it is said that trillions of dollars moved to invest in food and primary commodities, causing the 2007–2008 food price crisis.[86]
The use of biofuels as a replacement for traditional fuels raises the price of food.[87] The United Nations special rapporteur on the right to food, Jean Ziegler proposes that agricultural waste, such as corn cobs and banana leaves, should be used as fuel instead of crops.[88]
In some developing countries, overnutrition (in the form of obesity) is beginning to appear in the same communities where malnutrition occurs.[89] Overnutrition increases with urbanisation, food commercialisation and technological developments and increases physical inactivity.[90] Variations in the health status of individuals in the same society are associated with the societal structure and an individual's socioeconomic status which leads to income inequality, racism, educational differences and lack of opportunities.[91]
Diseases and conditions
[edit]Infectious diseases which increase nutrient requirements, such as gastroenteritis,[92] pneumonia, malaria, and measles, can cause malnutrition.[5] So can some chronic illnesses, especially HIV/AIDS.[93][94]
Malnutrition can also result from abnormal nutrient loss due to diarrhea or chronic small bowel illnesses, like Crohn's disease or untreated coeliac disease.[4][8][95] "Secondary malnutrition" can result from increased energy expenditure.[66][96]
In infants, a lack of breastfeeding may contribute to undernourishment.[66][96] Anorexia nervosa and bariatric surgery can also cause malnutrition.[97][98]
Dietary practices
[edit]Undernutrition
[edit]Undernutrition due to lack of adequate breastfeeding is associated with the deaths of an estimated one million children annually. Illegal advertising of breast-milk substitutes contributed to malnutrition and continued three decades after its 1981 prohibition under the WHO International Code of Marketing Breast Milk Substitutes.[99]
Maternal malnutrition can also factor into the poor health or death of a baby. Over 800,000 neonatal deaths have occurred because of deficient growth of the fetus in the mother's womb.[100]
Deriving too much of one's diet from a single source, such as eating almost exclusively potato, maize or rice, can cause malnutrition. This may either be from a lack of education about proper nutrition, only having access to a single food source, or from poor healthcare access and unhealthy environments.[101][102]
It is not just the total amount of calories that matters but specific nutritional deficiencies such as vitamin A deficiency, iron deficiency or zinc deficiency can also increase risk of death.[103]
Overnutrition
[edit]
Overnutrition caused by overeating is also a form of malnutrition. In the United States, more than half of all adults are now overweight—a condition that, like hunger, increases susceptibility to disease and disability, reduces worker productivity, and lowers life expectancy.[81] Overeating is much more common in the United States, since most people have adequate access to food. Many parts of the world have access to a surplus of non-nutritious food. Increased sedentary lifestyles also contribute to overnutrition. Yale University psychologist Kelly Brownell calls this a "toxic food environment", where fat- and sugar-laden foods have taken precedence over healthy nutritious foods.[81]
In these developed countries, overnutrition can be prevented by choosing the right kind of food. More fast food is consumed per capita in the United States than in any other country. This mass consumption of fast food results from its affordability and accessibility. Fast food, which is low in cost and nutrition, is high in calories. Due to increasing urbanization and automation, people are living more sedentary lifestyles. These factors combine to make weight gain difficult to avoid.[104]
Overnutrition also occurs in developing countries. It has appeared in parts of developing countries where income is on the rise.[81] It is also a problem in countries where hunger and poverty persist. Economic development, rapid urbanisation and shifting dietary patterns have increased the burden of overnutrition in the cities of low and middle-income countries.[105] In China, consumption of high-fat foods has increased, while consumption of rice and other goods has decreased.[81] Overeating leads to many diseases, such as heart disease and diabetes, that may be fatal.
Agricultural productivity
[edit]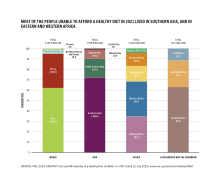
Local food shortages can be caused by a lack of arable land, adverse weather, and/or poorer farming skills (like inadequate crop rotation). They can also occur in areas which lack the technology or resources needed for the higher yields found in modern agriculture. These resources include fertilizers, pesticides, irrigation, machinery, and storage facilities. As a result of widespread poverty, farmers and governments cannot provide enough of these resources to improve local yields.[citation needed]
Additionally, the World Bank and some wealthy donor countries have pressured developing countries to use free market policies. Even as the United States and Europe extensively subsidized their own farmers, they urged developing countries to cut or eliminate subsidized agricultural inputs, like fertilizer.[106][107] Without subsidies, few (if any) farmers in developing countries can afford fertilizer at market prices. This leads to low agricultural production, low wages, and high, unaffordable food prices.[106] Fertilizer is also increasingly unavailable because Western environmental groups have fought to end its use due to environmental concerns. The Green Revolution pioneers Norman Borlaug and Keith Rosenberg cited as the obstacle to feeding Africa by .[108]
Future threats
[edit]In the future, variety of factors could potentially disrupt global food supply and cause widespread malnutrition. According to UNICEF's projections, it is projected that almost 600 million people will be chronically undernourished in 2030.[109]
Global warming is of importance to food security. Almost all malnourished people (95%) live in the tropics and subtropics, where the climate is relatively stable. According to the latest Intergovernmental Panel on Climate Change reports, temperature increases in these regions are "very likely."[110] Even small changes in temperatures can make extreme weather conditions occur more frequently.[110] Extreme weather events, like drought, have a major impact on agricultural production, and hence nutrition. For example, the 1998–2001 Central Asian drought killed about 80 percent of livestock in Iran and caused a 50% reduction in wheat and barley crops there.[111] Other central Asian nations experienced similar losses. An increase in extreme weather such as drought in regions such as Sub-Saharan Africa would have even greater consequences in terms of malnutrition. Even without an increase of extreme weather events, a simple increase in temperature reduces the productivity of many crop species, and decreases food security in these regions.[110][112]
Another threat is colony collapse disorder, a phenomenon where bees die in large numbers.[113] Since many agricultural crops worldwide are pollinated by bees, colony collapse disorder represents a threat to the global food supply.[114]
Prevention
[edit]
Reducing malnutrition is key part of the United Nations' Sustainable Development Goal 2 (SDG2), "Zero Hunger", which aims to reduce malnutrition, undernutrition, and stunted child growth.[115] Managing severe acute undernutrition in a community setting has received significant research attention.[78][51]
Food security
[edit]In the 1950s and 1960s, the Green Revolution aimed to bring modern Western agricultural techniques (like nitrogen fertilizers and pesticides) to Asia. Investments in agriculture, such as fund fertilizers and seeds, increased food harvests and thus food production. Consequently, food prices and malnutrition decreased (as they had earlier in Western nations).[106][116]
The Green Revolution was possible in Asia because of existing infrastructure and institutions, such as a system of roads and public seed companies that made seeds available.[117] These resources were in short supply in Africa, decreasing the Green Revolution's impact on the continent.
For example, almost five million of the 13 million people in Malawi used to need emergency food aid. However, in the early 2000s, the Malawian government changed its agricultural policies, and implemented subsidies for fertilizer and seed introduced against World Bank strictures. By 2007, farmers were producing record-breaking corn harvests. Corn production leaped to 3.4 million in 2007 compared to 1.2 million in 2005, making Malawi a major food exporter.[106] Consequently, food prices lowered and wages for farmworkers rose.[106] Such investments in agriculture are still needed in other African countries like the Democratic Republic of the Congo (DRC). Despite the country's great agricultural potential, the prevalence of malnutrition in the DRC is among the highest in the world.[118] Proponents for investing in agriculture include Jeffrey Sachs, who argues that wealthy countries should invest in fertilizer and seed for Africa's farmers.[106][119]
Imported Ready to Use Therapeutic Food (RUTF) has been used to treat malnutrition in northern Nigeria. Some Nigerians also use soy kunu, a locally sourced and prepared blend consisting of peanut, millet and soybeans.[120]
New technology in agricultural production has great potential to combat undernutrition. It makes farming easier, thus improving agricultural yields.[121] By increasing farmers' incomes, this could reduce poverty. It would also open up area which farmers could use to diversify crops for household use.
The World Bank claims to be part of the solution to malnutrition, asserting that countries can best break the cycle of poverty and malnutrition by building export-led economies, which give them the financial means to buy foodstuffs on the world market.
Economics
[edit]Many aid groups have found that giving cash assistance (or cash vouchers) is more effective than donating food. Particularly in areas where food is available but unaffordable, giving cash assistance is a cheaper, faster, and more efficient way to deliver help to the hungry.[122] In 2008, the UN's World Food Program, the biggest non-governmental distributor of food, announced that it would begin distributing cash and vouchers instead of food in some areas, which Josette Sheeran, the WFP's executive director, described as a "revolution" in food aid.[122][123] The aid agency Concern Worldwide piloted a method of giving cash assistance using a mobile phone operator, Safaricom, which runs a money transfer program that allows cash to be sent from one part of a country to another.[122]
However, during a drought, delivering food might be the most appropriate way to help people, especially those who live far from markets and thus have limited access to them.[122] Fred Cuny stated that "the chances of saving lives at the outset of a relief operation are greatly reduced when food is imported. By the time it arrives in the country and gets to people, many will have died."[124] U.S. law requires food aid to be purchased at home rather than in the countries where the hungry live; this is inefficient because approximately half of the money spent goes for transport.[125] Cuny further pointed out that "studies of every recent famine have shown that food was available in-country—though not always in the immediate food deficit area" and "even though by local standards the prices are too high for the poor to purchase it, it would usually be cheaper for a donor to buy the hoarded food at the inflated price than to import it from abroad."[126]

Food banks and soup kitchens address malnutrition in places where people lack money to buy food. A basic income has been proposed as a way to ensure that everyone has enough money to buy food and other basic needs. This is a form of social security in which all citizens or residents of a country regularly receive an unconditional sum of money, either from a government or some other public institution, in addition to any income received from elsewhere.[127]
Successful initiatives
[edit]Ethiopia pioneered a program that later became part of the World Bank's prescribed method for coping with a food crisis. Through the country's main food assistance program, the Productive Safety Net Program, Ethiopia provided rural residents who were chronically short of food a chance to work for food or cash. Foreign aid organizations like the World Food Program were then able to buy food locally from surplus areas to distribute in areas with a shortage of food.[128] Aid organizations now view the Ethiopian program as a model of how to best help hungry nations.[citation needed]
Successful initiatives also include Brazil's recycling program for organic waste, which benefits farmers, the urban poor, and the city in general. City residents separate organic waste from their garbage, bag it, and then exchange it for fresh fruit and vegetables from local farmers. This reduces the country's waste while giving the urban poor a steady supply of nutritious food.[104]
World population
[edit]Restricting population size is a proposed solution to malnutrition. Thomas Malthus argues that population growth can be controlled by natural disasters and by voluntary limits through "moral restraint."[129] Robert Chapman suggests that government policies are a necessary ingredient for curtailing global population growth.[130] The United Nations recognizes that poverty and malnutrition (as well as the environment) are interdependent and complementary with population growth.[131] According to the World Health Organization, "Family planning is key to slowing unsustainable population growth and the resulting negative impacts on the economy, environment, and national and regional development efforts".[132] However, more than 200 million women worldwide lack adequate access to family planning services.
There are different theories about what causes famine. Some theorists, like the Indian economist Amartya Sen, believe that the world has more than enough resources to sustain its population. In this view, malnutrition is caused by unequal distribution of resources and under- or unused arable land.[133][134] For example, Sen argues that "no matter how a famine is caused, methods of breaking it call for a large supply of food in the Public Distribution System. This applies not only to organizing rationing and control, but also to undertaking work programmes and other methods of increasing purchasing power for those hit by shifts in exchange entitlements in a general inflationary situation."[82]
Food sovereignty
[edit]Food sovereignty is one suggested policy framework to resolve access issues. In this framework, people (rather than international market forces) have the right to define their own food, agricultural, livestock, and fishery systems. Food First is one of the primary think tanks working to build support for food sovereignty. Neoliberals advocate for an increasing role of the free market.[citation needed]
Health facilities
[edit]Another possible long-term solution to malnutrition is to increase access to health facilities in rural parts of the world. These facilities could monitor undernourished children, act as supplemental food distribution centers, and provide education on dietary needs. Similar facilities have already proven very successful in countries such as Peru and Ghana.[135][136]
Breastfeeding
[edit]In 2016, estimates suggested that more widespread breastfeeding could prevent about 823,000 deaths annually of children under age 5.[137] In addition to reducing infant deaths, breast milk provides an important source of micronutrients - which are clinically proven to bolster children's immune systems – and provides long-term defenses against non-communicable and allergic diseases.[138] Breastfeeding may improve cognitive abilities in children, and correlates strongly with individual educational achievements.[138][139] As previously noted, lack of proper breastfeeding is a major factor in child mortality rates, and is a primary determinant of disease development for children. The medical community recommends exclusively breastfeeding infants for 6 months, with nutritional whole food supplementation and continued breastfeeding up to 2 years or older for overall optimal health outcomes.[139][140][141] Exclusive breastfeeding is defined as giving an infant only breast milk for six months as a source of food and nutrition.[139][141] This means no other liquids, including water or semi-solid foods.[141]
Barriers to breastfeeding
[edit]Breastfeeding is noted as one of the most cost-effective medical interventions benefiting child health.[140] While there are considerable differences among developed and developing countries, there are universal determinants of whether a mother breastfeeds or uses formula; these include income, employment, social norms, and access to healthcare.[139][140] Many newly made mothers face financial barriers; community-based healthcare workers have helped to alleviate these barriers, while also providing a viable alternative to traditional and expensive hospital-based medical care.[139] Recent studies, based upon surveys conducted from 1995 to 2010, show that exclusive breastfeeding rates have risen globally, from 33% to 39%.[141] Despite the growth rates, medical professionals acknowledge the need for improvement given the importance of exclusive breastfeeding.[141]
21st century global initiatives
[edit]Starting around 2009, there was renewed international media and political attention focused on malnutrition. This resulted in part from spikes in food prices and the 2008 financial crisis. Additionally, there was an emerging consensus that combating malnutrition is one of the most cost-effective ways to contribute to development. This led to the 2010 launch of the UN's Scaling up Nutrition movement (SUN).[142]
In April 2012, a number of countries signed the Food Assistance Convention, the world's first legally binding international agreement on food aid. The following month, the Copenhagen Consensus recommended that politicians and private sector philanthropists should prioritize interventions against hunger and malnutrition to maximize the effectiveness of aid spending. The Consensus recommended prioritizing these interventions ahead of any others, including the fights against malaria and AIDS.[143]
In June 2015, the European Union and the Bill & Melinda Gates Foundation launched a partnership to combat undernutrition, especially in children. The program was first implemented in Bangladesh, Burundi, Ethiopia, Kenya, Laos and Niger. It aimed to help these countries improve information and analysis about nutrition, enabling them to develop effective national nutrition policies.[144]
Also in 2015, the UN's Food and Agriculture Organization created a partnership aimed at ending hunger in Africa by 2025. The African Union's Comprehensive Africa Agriculture Development Programme (CAADP) provided the framework for the partnership. It includes a variety of interventions, including support for improved food production, a strengthening of social protection, and integration of the right to food into national legislation.[145]
The EndingHunger campaign is an online communication campaign whose goal is to raise awareness about hunger. The campaign has created viral videos depicting celebrities voicing their anger about the large number of hungry people in the world.[citation needed]
After the Millennium Development Goals expired in 2015, the Sustainable Development Goals became the main global policy focus to reduce hunger and poverty. In particular, Goal 2: Zero Hunger sets globally agreed-upon targets to wipe out hunger, end all forms of malnutrition, and make agriculture sustainable.[146] The partnership Compact2025 develops and disseminates evidence-based advice to politicians and other decision-makers, with the goal of ending hunger and undernutrition by 2025.[147][148][149] The International Food Policy Research Institute (IFPRI) led the partnership, with the involvement of UN organisations, non-governmental organizations (NGOs), and private foundations.
Treatment
[edit]

Improving nutrition
[edit]Efforts such as infant and young child feeding practices to improve nutrition are some of the common forms of development aid.[6][150] Interventions often promote breastfeeding to reduce rates of malnutrition and death in children.[1] Some of these interventions have been successful.[7] For example, interventions with commodities such as ready to use therapeutic foods, ready to use supplementary foods, micronutrient intervention and vitamin supplementation were identified to significantly improve nutrition, reduce stunting and prevent diseases in communities with severe acute malnutrition.[78] In young children, outcomes improve when children between six months and two years of age receive complementary food (in addition to breast milk).[7] There is also good evidence that supports giving supplemental micronutrients to pregnant women and young children in the developing world.[7]
The United Nations has reported on the importance of nutritional counselling and support, for example in the care of HIV-infected persons, especially in "resource-constrained settings where malnutrition and food insecurity are endemic".[151] UNICEF provides nutritional counselling services for malnourished children in Afghanistan.[152]
Sending food and money is a common form of development aid, aimed at feeding hungry people. Some strategies help people buy food within local markets.[6][153] Simply feeding students at school is insufficient.[6]
Longer-term measures include improving agricultural practices,[154] reducing poverty, and improving sanitation.
Identifying malnourishment
[edit]Measuring children is crucial to identifying malnourishment. In 2000, the United States Centers for Disease Control and Prevention (CDC) established the International Micronutrient Malnutrition Prevention and Control (IMMPaCt) program. It tested children for malnutrition by conducting a three-dimensional scan, using an iPad or a tablet. Its objective was to help doctors provide more efficient treatments.[155] There may be some chance of error when using this method.[155] The Screening Tool for the Assessment of Malnutrition in Paediatrics (STAMPa) is another method for the identification and evaluation of malnutrition in young children.[156] The assessment tool has fair to medium reliability in the identification of children at risk of malnutrition.[156]
A systematic review of 42 studies found that many approaches to mitigating acute malnutrition are equally effective; thus, intervention decisions can be based on cost-related factors. Overall, evidence for the effectiveness of acute malnutrition interventions is not robust. The limited evidence related to cost indicates that community and outpatient management of children with uncomplicated malnutrition may be the most cost-effective strategy.[157]
Regularly measuring and charting children's growth and including activities to promote health (an intervention called growth monitoring and promotion, also known as GPM) is often considered by policy makers and is recommended by the World Health Organization.[158] This program is often performed at the same time as a child has their regular immunizations.[159] Despite widespread use of this type of program, further studies are needed to understand the impact of these programs on overall child health and how to better address faltering growth in a child and improve practices related to feeding children in lower to middle income countries.[159]
Medical management
[edit]It is often possible to manage severe malnutrition within a person's home, using ready-to-use therapeutic foods.[7] In people with severe malnutrition complicated by other health problems, treatment in a hospital setting is recommended.[7] In-hospital treatment often involves managing low blood sugar, maintaining adequate body temperature, addressing dehydration, and gradual feeding.[7][160]
Routine antibiotics are usually recommended because malnutrition weakens the immune system, causing a high risk of infection.[160] Additionally, broad spectrum antibiotics are recommended in all severely undernourished children with diarrhea requiring admission to hospital.[161]
A severely malnourished child who appears to have dehydration, but has not had diarrhea, should be treated as if they have an infection.[161]
Among malnourished people who are hospitalized, nutritional support improves protein intake, calorie intake, and weight.[162]
Bangladeshi model
[edit]
In response to child malnutrition, the Bangladeshi government recommends ten steps for treating severe malnutrition:[163]
- Prevent or treat dehydration
- Prevent or treat low blood sugar
- Prevent or treat low body temperature
- Prevent or treat infection;
- Correct electrolyte imbalances
- Correct micronutrient deficiencies
- Start feeding cautiously
- Achieve catch-up growth
- Provide psychological support
- Prepare for discharge and follow-up after recovery
Therapeutic foods
[edit]Due in part to limited research on supplementary feeding, there is little evidence that this strategy is beneficial.[164] A 2015 systematic review of 32 studies found that there are limited benefits when children under 5 receive supplementary feeding, especially among younger, poorer, and more undernourished children.[165]
However, specially formulated foods do appear to be useful in treating moderate acute malnutrition in the developing world.[166] These foods may have additional benefits in humanitarian emergencies, since they can be stored for years, can be eaten directly from the packet, and do not have to be mixed with clean water or refrigerated.[167] In young children with severe acute malnutrition, it is unclear if ready-to-use therapeutic food differs from a normal diet.[168]
Severely malnourished individuals can experience refeeding syndrome if fed too quickly.[169] Refeeding syndrome can result regardless of whether food is taken orally, enterally or parenterally.[169] It can present several days after eating with potentially fatal heart failure, dysrhythmias, and confusion.[169][170]
Some manufacturers have fortified everyday foods with micronutrients before selling them to consumers. For example, flour has been fortified with iron, zinc, folic acid, and other B vitamins like thiamine, riboflavin, niacin and vitamin B12.[103] Baladi bread (Egyptian flatbread) is made with fortified wheat flour. Other fortified products include fish sauce in Vietnam and iodized salt.[167]
Micronutrient supplementation
[edit]According to the World Bank, treating malnutrition – mostly by fortifying foods with micronutrients – improves lives more quickly than other forms of aid, and at a lower cost.[171] After reviewing a variety of development proposals, The Copenhagen Consensus, a group of economists who reviewed a variety of development proposals, ranked micronutrient supplementation as its number-one treatment strategy.[172][125]
In malnourished people with diarrhea, zinc supplementation is recommended following an initial four-hour rehydration period. Daily zinc supplementation can help reduce the severity and duration of the diarrhea. Additionally, continuing daily zinc supplementation for ten to fourteen days makes diarrhea less likely to recur in the next two to three months.[173]
Malnourished children also need both potassium and magnesium.[163] Within two to three hours of starting rehydration, children should be encouraged to take food, particularly foods rich in potassium[163][173] like bananas, green coconut water, and unsweetened fresh fruit juice.[173] Along with continued eating, many homemade products can also help restore normal electrolyte levels. For example, early during the course of a child's diarrhea, it can be beneficial to provide cereal water (salted or unsalted) or vegetable broth (salted or unsalted).[173] If available, vitamin A, potassium, magnesium, and zinc supplements should be added, along with other vitamins and minerals.[163]
Giving base (as in Ringer's lactate) to treat acidosis without simultaneously supplementing potassium worsens low blood potassium.[173]
Treating diarrhea
[edit]Preventing dehydration
[edit]Food and drink can help prevent dehydration in malnourished people with diarrhea. Eating (or breastfeeding, among infants) should resume as soon as possible.[161] Sugary beverages like soft drinks, fruit juices, and sweetened teas are not recommended as they may worsen diarrhea.[174]
Malnourished people with diarrhea (especially children) should be encouraged to drink fluids; the best choices are fluids with modest amounts of sugar and salt, like vegetable broth or salted rice water. If clean water is available, they should be encouraged to drink that too. Malnourished people should be allowed to drink as much as they want, unless signs of swelling emerge.
Babies can be given small amounts of fluids via an eyedropper or a syringe without the needle. Children under two should receive a teaspoon of fluid every one to two minutes; older children and adults should take frequent sips of fluids directly from a cup.[173] After the first two hours, fluids and foods should be alternated, rehydration should be continued at the same rate or more slowly, depending on how much fluid the child wants and whether they are having ongoing diarrhea.[163]
If vomiting occurs, fluids can be paused for 5–10 minutes and then restarted more slowly. Vomiting rarely prevents rehydration, since fluids are still absorbed and vomiting is usually short-term.[174]
Oral rehydration therapy
[edit]If prevention has failed and dehydration develops, the preferred treatment is rehydration through oral rehydration therapy (ORT). In severely undernourished children with diarrhea, rehydration should be done slowly, according to the World Health Organization.
Oral rehydration solutions consist of clean water mixed with small amounts of sugars and salts. These solutions help restore normal electrolyte levels, provide a source of carbohydrates, and help with fluid replacement.[175]
Reduced-osmolarity ORS is the current standard of care for oral rehydration therapy, with reasonably wide availability.[176][177] Introduced in 2003 by WHO and UNICEF, reduced-osmolarity solutions contain lower concentrations of sodium and glucose than original ORS preparations. Reduced-osmolarity ORS has the added benefit of reducing stool volume and vomiting while simultaneously preventing dehydration. Packets of reduced-osmolarity ORS include glucose, table salt, potassium chloride, and trisodium citrate. For general use, each packet should be mixed with a liter of water. However, for malnourished children, experts recommend adding a packet of ORS to two liters of water, along with an extra 50 grams of sucrose and some stock potassium solution.[178]
People who have no access to commercially available ORS can make a homemade version using water, sugar, and table salt. Experts agree that homemade ORS preparations should include one liter (34 oz.) of clean water and 6 teaspoons of sugar; however, they disagree about whether they should contain half a teaspoon of table salt or a full teaspoon. Most sources recommend using half a teaspoon of salt per liter of water.[173][179][180][181] However, people with malnutrition have an excess of body sodium.[163] To avoid worsening this symptom, ORS for people with severe undernutrition should contain half the usual amount of sodium and more potassium.
Patients who do not drink may require fluids by nasogastric tube. Intravenous fluids are recommended only in those who have significant dehydration due to their potential complications, including congestive heart failure.[161]

Low blood sugar
[edit]Hypoglycemia, whether known or suspected, can be treated with a mixture of sugar and water. If the patient is conscious, the initial dose of sugar and water can be given by mouth.[182] Otherwise, they should receive glucose by intravenous or nasogastric tube. If seizures occur (and continue after glucose is given), rectal diazepam may be helpful. Blood sugar levels should be re-checked on two-hour intervals.[163]
Hypothermia
[edit]Hypothermia (dangerously low core body temperature) can occur in malnutrition, particularly in children. Mild hypothermia causes confusion, trembling, and clumsiness; more severe cases can be fatal. Keeping malnourished children warm can prevent or treat hypothermia. Covering the child (including their head) in blankets is one method. Another method is to warm the child through direct skin-to-skin contact with their mother or father, then covering both parent and child.
Warming methods are usually most important at night.[163] Prolonged bathing or prolonged medical exams can further lower body temperature and are not recommended for malnourished children at high risk of hypothermia.
Epidemiology
[edit]

| no data <200 200–400 400–600 600–800 800–1000 1000–1200 | 1200–1400 1400–1600 1600–1800 1800–2000 2000–2200 >2200 |
The figures provided in this section on epidemiology all refer to undernutrition even if the term malnutrition is used which, by definition, could also apply to too much nutrition.
The Global Hunger Index (GHI) is a multidimensional statistical tool used to describe the state of countries' hunger situation. The GHI measures progress and failures in the global fight against hunger.[184] The GHI is updated once a year. The data from the 2015 report shows that Hunger levels have dropped 27% since 2000. Fifty two countries remain at serious or alarming levels. In addition to the latest statistics on Hunger and Food Security, the GHI also features different special topics each year. The 2015 report include an article on conflict and food security.[185]
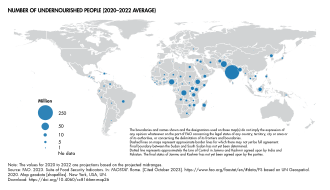
People affected
[edit]The United Nations estimated that there were 821 million undernourished people in the world in 2017. This is using the UN's definition of 'undernourishment', where it refers to insufficient consumption of raw calories, and so does not necessarily include people who lack micro nutrients.[9] The undernourishment occurred despite the world's farmers producing enough food to feed around 12 billion people—almost double the current world population.[186]
Malnutrition, as of 2010, was the cause of 1.4% of all disability adjusted life years.[187]
| Year | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|---|---|
| Number in millions | 793.4 | 746.5 | 691.0 | 663.1 | 661.8 | 597.8 | 578.3 | 580.0 | 572.3 |
| Percentage (%) | 12.1% | 11.2% | 10.3% | 9.7% | 9.6% | 8.6% | 8.2% | 8.1% | 7.9% |
| Year | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 |
| Number in millions | 563.9 | 588.9 | 586.4 | 571.8 | 586.8 | 612.8 | 701.4 | 738.9 | 735.1 |
| Percentage (%) | 7.7% | 7.9% | 7.8% | 7.5% | 7.6% | 7.9% | 8.9% | 9.3% | 9.2% |
| Year | 1970 | 1980 | 1991 | 1996 | 2002 | 2004 | 2006 | 2011 |
|---|---|---|---|---|---|---|---|---|
| Number in millions | 875 | 841 | 820 | 790 | 825 | 848 | 927 | 805 |
| Percentage (%) | 37% | 28% | 20% | 18% | 17% | 16% | 17% | 14% |

In 2010 protein-energy malnutrition resulted in 600,000 deaths down from 883,000 deaths in 1990.[192] Other nutritional deficiencies, which include iodine deficiency and iron deficiency anemia, result in another 84,000 deaths.[192] In 2010 malnutrition caused about 1.5 million deaths in women and children.[193]
According to the World Health Organization, malnutrition is the biggest contributor to child mortality, present in half of all cases.[194] Six million children die of hunger every year.[195] Underweight births and intrauterine growth restrictions cause 2.2 million child deaths a year. Poor or non-existent breastfeeding causes another 1.4 million. Other deficiencies, such as lack of vitamin A or zinc, for example, account for 1 million. Malnutrition in the first two years is irreversible. Malnourished children grow up with worse health and lower education achievement. Their own children tend to be smaller. Malnutrition was previously[when?] seen as something that exacerbates the problems of diseases such as measles, pneumonia and diarrhea, but malnutrition actually causes diseases, and can be fatal in its own right.[194]
History
[edit]Hunger has been a perennial human problem. However, until the early 20th century, there was relatively little awareness of the qualitative aspects of malnutrition.
Throughout history, various peoples have known the importance of eating certain foods to prevent symptoms now associated with malnutrition. Yet such knowledge appears to have been repeatedly lost and then re-discovered. For example, the ancient Egyptians reportedly knew the symptoms of scurvy. Much later, in the 14th century, Crusaders sometimes used anti-scurvy measures – for example, ensuring that citrus fruits were planted on Mediterranean islands, for use on sea journeys. However, for several centuries, Europeans appear to have forgotten the importance of these measures. They rediscovered this knowledge in the 18th century, and by the early 19th century, the Royal Navy was issuing frequent rations of lemon juice to every crewman on their ships. This massively reduced scurvy deaths among British sailors, which in turn gave the British a significant advantage in the Napoleonic Wars. Later on in the 19th century, the Royal Navy replaced lemons with limes (unaware at the time that lemons are far more effective at preventing scurvy).[196][197]
According to historian Michael Worboys, malnutrition was essentially discovered, and the science of nutrition established, between World War I and World War II. Advances built on prior works like Casimir Funk's 1912 formulisation of the concept of vitamins. Scientific study of malnutrition increased in the 1920s and 1930s, and grew even more common after World War II.
Non-governmental organizations and United Nations agencies began to devote considerable energy to alleviating malnutrition around the world. The exact methods and priorities for doing this tended to fluctuate over the years, with varying levels of focus on different types of malnutrition like Kwashiorkor or Marasmus; varying levels of concern on protein deficiency compared to vitamins, minerals and lack of raw calories; and varying priorities given to the problem of malnutrition in general compared to other health and development concerns. The green Revolution of the 1950s and 1960s saw considerable improvement in capability to prevent malnutrition.[197][196][198]
One of the first official global documents addressing Food security and global malnutrition was the 1948 Universal Declaration of Human Rights(UDHR). Within this document it stated that access to food was part of an adequate right to a standard of living.[199] The Right to food was asserted in the International Covenant on Economic, Social and Cultural Rights, a treaty adopted by the United Nations General Assembly on December 16, 1966. The Right to food is a human right for people to feed themselves in dignity, be free from hunger, food insecurity, and malnutrition.[200] As of 2018, the treaty has been signed by 166 countries, by signing states agreed to take steps to the maximum of their available resources to achieve the right to adequate food.
However, after the 1966 International Covenant the global concern for the access to sufficient food only became more present, leading to the first ever World Food Conference that was held in 1974 in Rome, Italy. The Universal Declaration on the Eradication of Hunger and Malnutrition was a UN resolution adopted November 16, 1974 by all 135 countries that attended the 1974 World Food Conference.[201] This non-legally binding document set forth certain aspirations for countries to follow to sufficiently take action on the global food problem. Ultimately this document outline and provided guidance as to how the international community as one could work towards fighting and solving the growing global issue of malnutrition and hunger.
Adoption of the right to food was included in the Additional Protocol to the American Convention on Human Rights in the area of Economic, Social, and Cultural Rights, this 1978 document was adopted by many countries in the Americas, the purpose of the document is, "to consolidate in this hemisphere, within the framework of democratic institutions, a system of personal liberty and social justice based on respect for the essential rights of man."[202]
A later document in the timeline of global initiatives for malnutrition was the 1996 Rome Declaration on World Food Security, organized by the Food and Agriculture Organization. This document reaffirmed the right to have access to safe and nutritious food by everyone, also considering that everyone gets sufficient food, and set the goals for all nations to improve their commitment to food security by halving their number of undernourished people by 2015.[203] In 2004 the Food and Agriculture Organization adopted the Right to Food Guidelines, which offered states a framework of how to increase the right to food on a national basis.
Special populations
[edit]Undernutrition is an important determinant of maternal and child health, accounting for more than a third of child deaths and more than 10 percent of the total global disease burden according to 2008 studies.[204]
Children
[edit]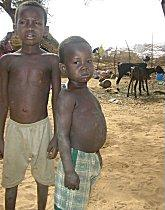
Undernutrition adversely affects the cognitive development of children, contributing to poor earning capacity and poverty in adulthood.[205] The development of childhood undernutrition coincides with the introduction of complementary weaning foods which are usually nutrient deficient.[206] The World Health Organization estimates that malnutrition accounts for 54 percent of child mortality worldwide,[56] about 1 million children.[207] There is a strong association between undernutrition and child mortality.[208] Another estimate also by WHO states that childhood underweight is the cause for about 35% of all deaths of children under the age of five years worldwide.[209] Over 90% of the stunted children below five years of age live in sub-Saharan Africa and South Central Asia.[78] Although access to adequate food and improving nutritional intake is an obvious solution to tackling undernutrition in children, the progress in reducing children undernutrition is disappointing.[210]
Women
[edit]

In 2022, more than 1 billion adolescent girls and women suffered from undernutrition, according to UNICEF's 2023 report "Undernourished and Overlooked: A Global Nutrition Crisis in Adolescent Girls and Women".[211] The gender gap in food insecurity more than doubled between 2019 (49 million) and 2021 (126 million). The report shows that globally, 30% of women aged 15–49 years are living with anaemia while 10 per cent of women aged 20–49 years suffer from underweight. South Asia, West and Central Africa and Eastern and Southern Africa are home to 60% of women with anaemia and 65% of women being underweight. In contrast, overweight is affecting more than 35% of women aged 20–49 years, of which 13% are living with obesity.[211] Middle East and North Africa has the highest prevalence of overweight with 61% affected. North America closely follows at 60%.[211] Fewer than 1 in 3 adolescent girls and women have diets meeting the minimum dietary diversity in the Sudan (10%), Burundi (12%), Burkina Faso (17%) and Afghanistan (26%).[211] In Niger, the percentage of women accessing a minimally diverse diet fell from 53% to 37% between 2020 and 2022.[211]
Researchers from the Centre for World Food Studies in 2003 found that the gap between levels of undernutrition in men and women is generally small, but that the gap varies from region to region and from country to country.[212] These small-scale studies showed that female undernutrition prevalence rates exceeded male undernutrition prevalence rates in South/Southeast Asia and Latin America and were lower in Sub-Saharan Africa.[212] Datasets for Ethiopia and Zimbabwe reported undernutrition rates between 1.5 and 2 times higher in men than in women; however, in India and Pakistan, datasets rates of undernutrition were 1.5–2 times higher in women than in men. Intra-country variation also occurs, with frequent high gaps between regional undernutrition rates.[212] Gender inequality in nutrition in some countries such as India is present in all stages of life.[213]
Studies on nutrition concerning gender bias within households look at patterns of food allocation, and one study from 2003 suggested that women often receive a lower share of food requirements than men.[212] Gender discrimination, gender roles, and social norms affecting women can lead to early marriage and childbearing, close birth spacing, and undernutrition, all of which contribute to malnourished mothers.[80]
Within the household, there may be differences in levels of malnutrition between men and women, and these differences have been shown to vary significantly from one region to another, with problem areas showing relative deprivation of women.[212] Samples of 1000 women in India in 2008 demonstrated that malnutrition in women is associated with poverty, lack of development and awareness, and illiteracy.[213] The same study showed that gender discrimination in households can prevent a woman's access to sufficient food and healthcare.[213] How socialization affects the health of women in Bangladesh, Najma Rivzi explains in an article about a research program on this topic.[214] In some cases, such as in parts of Kenya in 2006, rates of malnutrition in pregnant women were even higher than rates in children.[215]
Women in some societies are traditionally given less food than men since men are perceived to have heavier workloads.[216] Household chores and agricultural tasks can in fact be very arduous and require additional energy and nutrients; however, physical activity, which largely determines energy requirements, is difficult to estimate.[212]
Physiology
[edit]Women have unique nutritional requirements, and in some cases need more nutrients than men; for example, women need twice as much calcium as men.[216]
Pregnancy and breastfeeding
[edit]During pregnancy and breastfeeding, women must ingest enough nutrients for themselves and their child, so they need significantly more protein and calories during these periods, as well as more vitamins and minerals (especially iron, iodine, calcium, folic acid, and vitamins A, C, and K).[216] In 2001 the FAO of the UN reported that iron deficiency affected 43 percent of women in developing countries and increased the risk of death during childbirth.[216] A 2008 review of interventions estimated that universal supplementation with calcium, iron, and folic acid during pregnancy could prevent 105,000 maternal deaths (23.6 percent of all maternal deaths).[217] Malnutrition has been found to affect three-quarters of UK women aged 16–49 indicated by them having less folic acid than the WHO recommended levels.[218]
Frequent pregnancies with short intervals between them and long periods of breastfeeding add an additional nutritional burden.[212]
Educating children
[edit]"Action for Healthy Kids" has created several methods to teach children about nutrition. They introduce 2 different topics, self-awareness which teaches children about taking care of their own health and social awareness, which is how culinary arts vary from culture to culture. As well as its importance when it comes to nutrition. They include eBooks, tips, cooking clubs. including facts about vegetables and fruits.[219]
Team Nutrition has created "MyPlate eBooks" this includes 8 different eBooks to download for free. These eBooks contain drawings to color, audio narration, and a large number of characters to make nutrition lessons entertaining for children.[220]
According to the FAO, women are often responsible for preparing food and have the chance to educate their children about beneficial food and health habits, giving mothers another chance to improve the nutrition of their children.[216]
Elderly
[edit]
Malnutrition and being underweight are more common in the elderly than in adults of other ages.[221] If elderly people are healthy and active, the aging process alone does not usually cause malnutrition.[222] However, changes in body composition, organ functions, adequate energy intake and ability to eat or access food are associated with aging, and may contribute to malnutrition.[223] Sadness or depression can play a role, causing changes in appetite, digestion, energy level, weight, and well-being.[222] A study on the relationship between malnutrition and other conditions in the elderly found that malnutrition in the elderly can result from gastrointestinal and endocrine system disorders, loss of taste and smell, decreased appetite and inadequate dietary intake.[223] Poor dental health, ill-fitting dentures, or chewing and swallowing problems can make eating difficult.[222] As a result of these factors, malnutrition is seen to develop more easily in the elderly.[224]
Rates of malnutrition tend to increase with age with less than 10 percent of the "young" elderly (up to age 75) malnourished, while 30 to 65 percent of the elderly in home care, long-term care facilities, or acute hospitals are malnourished.[225] Many elderly people require assistance in eating, which may contribute to malnutrition.[224] However, the mortality rate due to undernourishment may be reduced.[226] Because of this, one of the main requirements of elderly care is to provide an adequate diet and all essential nutrients.[227] Providing the different nutrients such as protein and energy keeps even small but consistent weight gain.[226] Hospital admissions for malnutrition in the United Kingdom have been related to insufficient social care, where vulnerable people at home or in care homes are not helped to eat.[228]
In Australia malnutrition or risk of malnutrition occurs in 80 percent of elderly people presented to hospitals for admission.[229] Malnutrition and weight loss can contribute to sarcopenia with loss of lean body mass and muscle function.[221] Abdominal obesity or weight loss coupled with sarcopenia lead to immobility, skeletal disorders, insulin resistance, hypertension, atherosclerosis, and metabolic disorders.[223] A paper from the Journal of the American Dietetic Association noted that routine nutrition screenings represent one way to detect and therefore decrease the prevalence of malnutrition in the elderly.[222]
See also
[edit]- Action Against Hunger
- A Place at the Table
- Agrobiodiversity
- Child health and nutrition in Africa
- Childhood obesity
- Community Therapeutic Care
- Deficiency (medicine)
- Eating disorder
- Economic issues
- Famine scales
- Fome Zero (Zero Hunger)
- Food Donation Connection
- Homelessness
- Hunger in the United Kingdom
- Hunger in the United States
- Hunger marches
- The Hunger Project
- Income inequality
- Integrated Food Security Phase Classification
- List of global issues
- Malnutrition in India
- Malnutrition in South Africa
- Malnutrition in Peru
- Malnutrition in Zimbabwe
- NutritionDay
- Nutrition and Education International
- Muselmann
- National Security Study Memorandum 200 (1974)
- Oxfam
- Poverty trap
- Project Open Hand
- Social programs
- Starvation response
- Sustainable fishery
- United Nations Millennium Declaration
- Vitamin deficiency
References
[edit]- ^ a b c d e f Facts for life (PDF) (4th ed.). New York: United Nations Children's Fund. 2010. pp. 61 and 75. ISBN 978-92-806-4466-1. Archived from the original (PDF) on December 12, 2018. Retrieved March 19, 2012.
- ^ a b c d e f g Young EM (2012). Food and development. Abingdon, Oxon: Routledge. pp. 36–38. ISBN 978-1-135-99941-4.
- ^ a b "malnutrition" at Dorland's Medical Dictionary
- ^ a b Papadia C, Di Sabatino A, Corazza GR, Forbes A (February 2014). "Diagnosing small bowel malabsorption: a review". Internal and Emergency Medicine (Review). 9 (1): 3–8. doi:10.1007/s11739-012-0877-7. PMID 23179329. S2CID 33775071.
- ^ a b c d e "Maternal, newborn, child and adolescent health". WHO. Archived from the original on March 10, 2012. Retrieved July 4, 2014.
- ^ a b c d "An update of 'The Neglected Crisis of Undernutrition: Evidence for Action'" (PDF). www.gov.uk. Department for International Development. October 2012. Retrieved July 5, 2014.
- ^ a b c d e f g Bhutta ZA, Das JK, Rizvi A, Gaffey MF, Walker N, Horton S, et al. (August 2013). "Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost?". Lancet. 382 (9890): 452–477. doi:10.1016/s0140-6736(13)60996-4. PMID 23746776. S2CID 11748341.
- ^ a b Kastin DA, Buchman AL (November 2002). "Malnutrition and gastrointestinal disease". Current Opinion in Clinical Nutrition and Metabolic Care (Review). 5 (6): 699–706. doi:10.1097/00075197-200211000-00014. PMID 12394647.
- ^ a b c The State of Food Insecurity in the World 2018. Food and Agricultural Organization of the United Nations. 2020. doi:10.4060/CA9692EN. ISBN 978-92-5-132901-6. S2CID 239729231. Retrieved January 11, 2019.
- ^ Wang, Haidong; Naghavi, Mohsen; Allen, Christine; Barber, Ryan M.; et al. (GBD 2015 Mortality and Causes of Death Collaborators) (October 8, 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- ^ a b c d e f g Katsilambros N (2011). Clinical Nutrition in Practice. John Wiley & Sons. p. 37. ISBN 978-1-4443-4777-7.
- ^ "Malnutrition". www.who.int. Retrieved May 3, 2024.
- ^ a b Hickson, Mary; Smith, Sara, eds. (2018). Advanced nutrition and dietetics in nutrition support. Hoboken, NJ. p. 3. ISBN 978-1-118-99386-6. OCLC 1004376424.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ "WHO, nutrition experts take action on malnutrition". World Health Organization. Archived from the original on April 14, 2011. Retrieved February 10, 2012.
- ^ Lenters, Lindsey; Wazny, Kerri; Bhutta, Zulfiqar A. (2016), Black, Robert E.; Laxminarayan, Ramanan; Temmerman, Marleen; Walker, Neff (eds.), "Management of Severe and Moderate Acute Malnutrition in Children", Reproductive, Maternal, Newborn, and Child Health: Disease Control Priorities, Third Edition (Volume 2), Washington (DC): The International Bank for Reconstruction and Development / The World Bank, doi:10.1596/978-1-4648-0348-2_ch11, ISBN 978-1-4648-0348-2, PMID 27227221, retrieved May 3, 2024
- ^ "Progress For Children: A Report Card On Nutrition" (PDF). UNICEF. Archived from the original (PDF) on January 12, 2021. Retrieved March 19, 2012.
- ^ Ngaruiya, C., Hayward, A., Post, L. and Mowafi, H., 2017. "Obesity as a form of malnutrition: over-nutrition on the Uganda 'malnutrition' agenda". Pan African Medical Journal, 28, p. 49.
- ^ Swinburn, B., Kraak, V., Allender, S., et al., 2019. "The Global Syndemic of Obesity, Undernutrition, and Climate Change: The Lancet Commission report." The Lancet, 393(10173), pp. 791–846.
- ^ References Min, J., Zhao, Y., Slivka, L. and Wang, Y., 2017. "Double burden of diseases worldwide: coexistence of undernutrition and overnutrition-related non-communicable chronic diseases". Obesity Reviews, 19(1), pp. 49–61.
- ^ "The Double Burden of Malnutrition". The Lancet Commission. December 16, 2019. Retrieved January 17, 2022.
- ^ a b Ghattas, H., Acharya, Y., Jamaluddine, Z., Assi, M., El Asmar, K. and Jones, A., 2020. The child-level double burden of malnutrition in the MENA and LAC regions: Prevalence and social determinants. Maternal & Child Nutrition, 16(2).
- ^ WHO. The double burden of malnutrition. Policy brief. Geneva: World Health Organization; 2017.
- ^ Liz Young (2002). World Hunger Routledge Introductions to Development. Routledge. p. 20. ISBN 978-1-134-77494-4.
- ^ a b c Murarkar, S., Gothankar, J., Doke, P., Pore, P., Lalwani, S., Dhumale, G., Quraishi, S., Patil, R., Waghachavare, V., Dhobale, R., Rasote, K., Palkar, S. and Malshe, N., 2020. Prevalence and determinants of undernutrition among under-five children residing in urban slums and rural area, Maharashtra, India: a community-based cross-sectional study. BMC Public Health, 20(1).
- ^ Estecha Querol, S., Al-Khudairy, L., Iqbal, R., Johnson, S. and Gill, P., 2021. Adolescent undernutrition in South Asia: a scoping review protocol. BMJ Open, 10(1), p.e031955.
- ^ a b c d e f g "The State of Food Security and Nutrition 2023". UNICEF Data. July 12, 2023. Retrieved October 25, 2023.
- ^ "Child Malnutrition". UNICEF. May 2023.
- ^ Gautam, S., Verma, M., Barman, S. and Arya, A., 2018. Nutritional status and its corelates in under five slum children of Kanpur Nagar, India. International Journal of Contemporary Pediatrics, 5(2), p.584.
- ^ Tesema, G., Yeshaw, Y., Worku, M., Tessema, Z. and Teshale, A., 2021. Pooled prevalence and associated factors of chronic undernutrition among under-five children in East Africa: A multilevel analysis. PLOS ONE, 16(3), p.e0248637.
- ^ Mrema, J., Elisaria, E., Mwanri, A. and Nyaruhucha, C., 2021. Prevalence and Determinants of Undernutrition among 6- to 59-Months-Old Children in Lowland and Highland Areas in Kilosa District, Tanzania: A Cross-Sectional Study. Journal of Nutrition and Metabolism, 2021, pp.1–9.
- ^ Kiarie, J., Karanja, S., Busiri, J., Mukami, D. and Kiilu, C., 2021. The prevalence and associated factors of undernutrition among under-five children in South Sudan using the standardized monitoring and assessment of relief and transitions (SMART) methodology. BMC Nutrition, 7(1).
- ^ "Malnutrition in Children". UNICEF DATA. Retrieved November 7, 2023.
- ^ World Health Organization, Global prevalence of vitamin A deficiency in populations at risk 1995–2005, World Health Organization global database on vitamin A deficiency.
- ^ Black RE et al., Maternal and child undernutrition: global and regional exposures and health consequences, The Lancet, 2008, 371(9608), p. 253.
- ^ "Vitamin A Deficiency in Children". UNICEF DATA. Retrieved October 31, 2023.
- ^ Biban BG, Lichiardopol C (2017). "Iodine Deficiency, Still a Global Problem?". Current Health Sciences Journal. 43 (2): 103–111. doi:10.12865/CHSJ.43.02.01. PMC 6284174. PMID 30595864.
- ^ "WHO guidance helps detect iron deficiency and protect brain development". www.who.int. Retrieved November 19, 2021.
- ^ Moumen, Hana (July 12, 2023). "State of Food Security and Nutrition in the World (SOFI) 2023". UNICEF DATA. Retrieved November 8, 2023.
- ^ van Zwienen-Pot, J., Visser, M., Kuijpers, M., Grimmerink, M. and Kruizenga, H., 2017. Undernutrition in nursing home rehabilitation patients. Clinical Nutrition, 36(3), pp. 755–759.
- ^ Rosenthal RA, Zenilman ME, Katlic MR, eds. (2011). Principles and practice of geriatric surgery (2nd ed.). Berlin: Springer. p. 78. ISBN 978-1-4419-6999-6.
- ^ McMinn, J., Steel, C. and Bowman, A., 2011. Investigation and management of unintentional weight loss in older adults. BMJ, 342(mar29 1), p. d1732.
- ^ "Global hunger declining, but still unacceptably high International hunger targets difficult to reach" (PDF). Food and Agriculture Organization of the United Nations. September 2010. Retrieved July 1, 2014.
- ^ Moumen, Hana (July 12, 2023). "State of Food Security and Nutrition in the World (SOFI) 2023". UNICEF DATA. Retrieved October 31, 2023.
- ^ Moumen, Hana (July 12, 2023). "State of Food Security and Nutrition in the World (SOFI) 2023". UNICEF DATA. Retrieved October 31, 2023.
- ^ a b Mark HE, Dias da Costa G, Pagliari C, Unger SA (December 2020). "Malnutrition: the silent pandemic". BMJ. 371: m4593. doi:10.1136/bmj.m4593. PMC 7705612. PMID 33262147.
- ^ "Goal 2020: Zero Hunger-United Nations". April 20, 2020.
- ^ Kulkarni, R., Rajput, U., Dawre, R., Sonkawade, N., Pawar, S., & Sonteke, S. et al. (2020). Severe Malnutrition and Anemia Are Associated with Severe COVID in Infants. Journal Of Tropical Pediatrics, 67(1). doi: 10.1093/tropej/fmaa084
- ^ "2020 Global crisis on Food crises". April 20, 2020.
- ^ a b Essentials of International Health. Jones & Bartlett Publishers. 2011. p. 194. ISBN 978-1-4496-6771-9.
- ^ a b c d World Health Organization (2013). Essential Nutrition Actions: Improving Maternal, Newborn, Infant and Young Child Health and Nutrition (PDF). Geneva: World Health Organization. pp. vi-94. ISBN 978-92-4-1505550.
- ^ a b c Morley, J., 2012. Undernutrition in older adults. Family Practice, 29(suppl 1), pp.i89-i93.
- ^ Cederholm, T., Bosaeus, I., Barazzoni, R., Bauer, J., Van Gossum, A., Klek, S., Muscaritoli, M., Nyulasi, I., Ockenga, J., Schneider, S., de van der Schueren, M. and Singer, P., 2015. Diagnostic criteria for malnutrition – An ESPEN Consensus Statement. Clinical Nutrition, 34(3), pp. 335–340.
- ^ Sobotka, L., 2012. Basics in clinical nutrition. 4th ed. Prague: Galen.
- ^ Martins, V., Toledo Florêncio, T., Grillo, L., Do Carmo P. Franco, M., Martins, P., Clemente, A., Santos, C., Vieira, M. and Sawaya, A., 2011. Long-Lasting Effects of Undernutrition. International Journal of Environmental Research and Public Health, 8(6), pp. 1817–1846.
- ^ Safiri S, Kolahi AA, Noori M, Nejadghaderi SA, Karamzad N, Bragazzi NL, et al. (November 2021). "Burden of anemia and its underlying causes in 204 countries and territories, 1990–2019: results from the Global Burden of Disease Study 2019". Journal of Hematology & Oncology. 14 (1): 185. doi:10.1186/s13045-021-01202-2. PMC 8567696. PMID 34736513.
- ^ a b Duggan C, Watkins JB, Walker WA, eds. (2008). Nutrition in pediatrics: basic science, clinical application. Hamilton: BC Decker. pp. 127–141. ISBN 978-1-55009-361-2.
- ^ "hypoalimentation" at Dorland's Medical Dictionary
- ^ a b c Chowdhury MS, Akhter N, Haque M, Aziz R, Nahar N (2009). "Serum Total Protein and Albumin Levels in Different Grades of Protein Energy Malnutrition". Journal of Bangladesh Society of Physiologist. 3: 58–60. doi:10.3329/jbsp.v3i0.1799.
- ^ Stanton J (2001). "Listening to the Ga: Cicely Williams' Discovery of Kwashiorkor on the Gold Coast". Women and Modern Medicine. Clio Medica. Vol. 61. pp. 149–171. doi:10.1163/9789004333390_008. ISBN 9789004333390. PMID 11603151. S2CID 34931635.
- ^ "Fact sheets – Malnutrition". World Health Organization. 2021. Retrieved January 27, 2022.
- ^ The GBD. 2015 Obesity Collaborators. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N. Engl J Med. 2017;377:13–27.
- ^ Nicolaidis S. Environment and obesity. Metabolism. 2019;100s:153942.
- ^ Billah, M., Khatiwada, S., Morris, M., & Maloney, C. (2022). Effects of paternal overnutrition and interventions on future generations. International Journal Of Obesity, 46(5), 901–917. doi: 10.1038/s41366-021-01042-7
- ^ "Diets". UNICEF DATA. Retrieved November 8, 2023.
- ^ a b Stevenson RD, Conaway MR (August 2011). "Weight and mortality rates: "Gómez classification" for children with cerebral palsy?". Pediatrics. 128 (2): e436–e437. doi:10.1542/peds.2011-1472. PMID 21768321. S2CID 1708728.
- ^ a b c d e Grover Z, Ee LC (October 2009). "Protein energy malnutrition". Pediatric Clinics of North America. 56 (5): 1055–1068. doi:10.1016/j.pcl.2009.07.001. PMID 19931063.
- ^ Gueri M, Gurney JM, Jutsum P (1980). "The Gomez classification. Time for a change?" (PDF). Bulletin of the World Health Organization. 58 (5): 773–777. PMC 2395976. PMID 6975186. Archived from the original (PDF) on January 27, 2005.
- ^ a b c Waterlow JC (September 1972). "Classification and definition of protein-calorie malnutrition". British Medical Journal. 3 (5826): 566–569. doi:10.1136/bmj.3.5826.566. PMC 1785878. PMID 4627051.
- ^ Watts G (December 2010). "John Conrad Waterlow". The Lancet. 376 (9757): 1982. doi:10.1016/S0140-6736(10)62252-0. S2CID 54424049.
- ^ a b c Stillwaggon E (2008). "Race, Sex, and the Neglected Risks for Women and Girls in Sub-Saharan Africa". Feminist Economics. 14 (4): 67–86. doi:10.1080/13545700802262923. S2CID 154082747.
- ^ Schaible UE, Kaufmann SH (May 2007). "Malnutrition and infection: complex mechanisms and global impacts". PLOS Medicine. 4 (5): e115. doi:10.1371/journal.pmed.0040115. PMC 1858706. PMID 17472433.
- ^ Laus MF, Vales LD, Costa TM, Almeida SS (February 2011). "Early postnatal protein-calorie malnutrition and cognition: a review of human and animal studies". International Journal of Environmental Research and Public Health. 8 (2): 590–612. doi:10.3390/ijerph8020590. PMC 3084481. PMID 21556206.
- ^ Kenton R. Holden (2007). "Malnutrition and Brain Development: A Review". Neurologic Consequences of Malnutrition (PDF). New York, NY: Demos Medical Publishing. ISBN 978-1-933864-03-7. Archived from the original (PDF) on May 10, 2013. Retrieved March 3, 2014.
- ^ a b c McNeil Jr DG (December 16, 2006). "In raising the world's IQ the secret is in salt". New York Times.
- ^ Kapil U (December 2007). "Health consequences of iodine deficiency". Sultan Qaboos University Medical Journal. 7 (3): 267–272. PMC 3074887. PMID 21748117.
- ^ "Bệnh suy dinh dưỡng trẻ em: Tổng hợp năm 2021". Y Khoa Blog (in Vietnamese). August 27, 2021. Retrieved October 4, 2021.
- ^ Hossain, A., Niroula, B., Duwal, S., Ahmed, S. and Kibria, M., 2020. Maternal profiles and social determinants of severe acute malnutrition among children under-five years of age: A case-control study in Nepal. Heliyon, 6(5), p.e03849.
- ^ a b c d e Bhutta, Z., Ahmed, T., Black, R., Cousens, S., Dewey, K., Giugliani, E., Haider, B., Kirkwood, B., Morris, S., Sachdev, H. and Shekar, M., 2008. What works? Interventions for maternal and child undernutrition and survival. The Lancet, 371(9610), pp.417–440.
- ^ Aheto JM, Keegan TJ, Taylor BM, Diggle PJ. Childhood Malnutrition and Its Determinants among Under-Five Children in Ghana. Paediatr Perinat Epidemiol. 2015;29(6):552–61.
- ^ a b Khan MM, Kraemer A (August 2009). "Factors associated with being underweight, overweight and obese among ever-married non-pregnant urban women in Bangladesh". Singapore Medical Journal. 50 (8): 804–813. PMID 19710981.
- ^ a b c d e Gardner G, Halweil B (2000). "Escaping Hunger, Escaping Excess". World Watch. 13 (4): 24. Archived from the original on January 12, 2012. Retrieved September 25, 2011.
- ^ a b Sen AK (1981). Poverty and famines: An essay on entitlement and deprivation. Oxford University Press. ISBN 978-0-19-828463-5.
- ^ Fotso JC, Kuate-Defo B (2005). "Measuring socioeconomic status in health research in developing countries: Should we be focusing on households, communities or both?". Social Indicators Research. 72 (2): 189–237. doi:10.1007/s11205-004-5579-8. S2CID 144596985.
- ^ Alvear-Vega, S. and Vargas-Garrido, H., 2022. Social determinants of malnutrition in Chilean children aged up to five. BMC Public Health, 22(1).
- ^ Tasnim, T., 2018. Determinants of Malnutrition in Children Under Five Years in Developing Countries: A Systematic Review. Indian Journal of Public Health Research & Development, 9(6), p.333.
- ^ "The role of speculators in the global food crisis". Spiegel Online.
- ^ "Biofuel use increasing poverty". BBC News. June 25, 2008.
- ^ Ferrett G (October 27, 2007). "Biofuels 'crime against humanity'". BBC News.
- ^ "Progress For Children: A Report Card On Nutrition" (PDF). UNICEF. Archived from the original (PDF) on January 12, 2021. Retrieved March 19, 2012.
- ^ Tremblay, M., Gray, C., Akinroye, K., Harrington, D., Katzmarzyk, P., Lambert, E., Liukkonen, J., Maddison, R., Ocansey, R., Onywera, V., Prista, A., Reilly, J., Martínez, M., Duenas, O., Standage, M. and Tomkinson, G., 2014. Physical Activity of Children: A Global Matrix of Grades Comparing 15 Countries. Journal of Physical Activity and Health, 11(s1), pp.S113-S125.
- ^ Gabriele, A. and Schettino, F., 2008. Child Malnutrition and Mortality in Developing Countries: Evidence from a Cross-Country Analysis. Analyses of Social Issues and Public Policy, 8(1), pp. 53–81.
- ^ Mandell GL, Bennett JE, Dolin R, Douglas RG, eds. (2010). Mandell, Douglas, and Bennett's principles and practice of infectious diseases (7th ed.). Philadelphia: Churchill Livingstone/Elsevier. pp. Chp 93. ISBN 978-0-443-06839-3.
- ^ Malnutrition at eMedicine
- ^ Baro M, Deubel TF (2006). "Persistent Hunger: Perspectives on Vulnerability, Famine, and Food Security in Sub-Saharan Africa". Annual Review of Anthropology. 35: 521–538. doi:10.1146/annurev.anthro.35.081705.123224.
- ^ Newnham ED (March 2017). "Coeliac disease in the 21st century: paradigm shifts in the modern age". Journal of Gastroenterology and Hepatology (Review). 32 (Suppl 1): 82–85. doi:10.1111/jgh.13704. PMID 28244672.
The epidemiology of coeliac disease (CD) is changing. Presentation of CD with malabsorptive symptoms or malnutrition is now the exception rather than the rule

- ^ a b World Health Organization (2001). "Water-related diseases: Malnutrition". Archived from the original on December 11, 2003.
- ^ Caballero B, Lindsay A, Prentice A, eds. (2005). Encyclopedia of human nutrition (2nd ed.). Amsterdam: Elsevier/Academic Press. p. 68. ISBN 978-0-08-045428-3.
- ^ Stoelting's anesthesia and co-existing disease (6th ed.). Philadelphia: Saunders/Elsevier. 2012. p. 324. ISBN 978-1-4557-3812-0.
- ^ Brady JP (June 2012). "Marketing breast milk substitutes: problems and perils throughout the world". Archives of Disease in Childhood. 97 (6): 529–532. doi:10.1136/archdischild-2011-301299. PMC 3371222. PMID 22419779.
- ^ "Malnutrition Kills Over 3 Million Children Annually Worldwide". Medical News Today. Retrieved February 20, 2018.
- ^ Burchi F, Fanzo J, Frison E (February 2011). "The role of food and nutrition system approaches in tackling hidden hunger". International Journal of Environmental Research and Public Health. 8 (2): 358–373. doi:10.3390/ijerph8020358. PMC 3084466. PMID 21556191.
- ^ "Causes and Impacts of Undernutrition over the Life Course" (PDF).
- ^ a b UNICEF (2013). Improving Child Nutrition – The achievable imperative for global progress. UNICEF
- ^ a b Gardner G, Halweil B (2000). "Escaping Hunger, Escaping Excess". World Watch. 13 (4): 5. Archived from the original on January 12, 2012. Retrieved September 25, 2011.
- ^ Ofori-Asenso, R., Agyeman, A., Laar, A. and Boateng, D., 2016. Overweight and obesity epidemic in Ghana – a systematic review and meta-analysis. BMC Public Health, 16(1).
- ^ a b c d e f Dugger CW (December 2, 2007). "Ending Famine, Simply by Ignoring the Experts". New York Times.
- ^ Biles P (February 6, 2006). "Zambia: fertile but hungry". BBC News.
- ^ "Forgotten benefactor of humanity". The Atlantic.
- ^ Moumen, Hana (July 12, 2023). "State of Food Security and Nutrition in the World (SOFI) 2023". UNICEF DATA. Retrieved November 8, 2023.
- ^ a b c "Climate Change 2007: Synthesis Report" (PDF). Intergovernmental Panel on Climate Change. November 12–17, 2007. Retrieved January 27, 2010.
- ^ Battisti, David S. "Climate Change in Developing Countries." University of Washington. Seattle. October 27, 2008.[verification needed]
- ^ Black, Richard (August 9, 2010). "Rice yields falling under global warming". BBC News; Science & Environment.
- ^ Honey Bee Die-Off Alarms Beekeepers, Crop growers and researchers
- ^ Wells M (March 11, 2007). "Vanishing bees threaten US crops". BBC News.
- ^ "Goal2: Zero Hunger – United Nations".
- ^ Barclay, Eliza (June 18, 2008). "How a Kenyan village tripled its corn harvest". Christian Science Monitor.
- ^ Dugger CW (October 10, 2007). "In Africa, prosperity from seeds falls short". New York Times.
- ^ John Ulimwengu; et al. (March 2013). "Need in a land of planty". dandc.eu.
- ^ Baker P, Dugger CW (July 9, 2009). "Obama enlists major powers to aid poor farmers with $15 billion". The New York Times.
- ^ Chinedu O (October 12, 2018). "Severe Malnutrition, A Disturbance in Nigerian Health Sector". Public Health Nigeria. Archived from the original on October 18, 2018. Retrieved October 17, 2018.
- ^ Li, Jiming, Yeyun Xin and Longping Yuan. (2010). Pushing the Yield Frontier: Hybrid rice in China. In MillionsFed: Proved Success in Agriculture Development. Washington, DC: International Policy Research Institute
- ^ a b c d "UN aid debate: give cash not food?". Christian Science Monitor. June 4, 2008.
- ^ "Cash roll-out to help hunger hot spots". World Food Programme. December 8, 2008. Archived from the original on February 12, 2009.
- ^ Andrew S. Natsios (Administrator U.S. Agency for International Development)
- ^ a b "Let them eat micronutrients". Newsweek.
- ^ Memorandum to former Representative Steve Solarz (United States, Democratic Party, New York), July 1994
- ^ "Improving Social Security in Canada Guaranteed Annual Income: A Supplementary Paper". Government of Canada. 1994. Retrieved November 30, 2013.
- ^ "A model of African food aid is now in trouble". Christian Science Monitor. May 6, 2008.
- ^ Malthus TR, Appleman P (1976). An essay on the principle of population: text, sources and background, criticism. Norton. ISBN 978-0-393-09202-8.
- ^ Chapman R (1999). "No room at the inn, or why population problems are not all economic". Population and Environment. 21: 81–97. doi:10.1007/BF02436122. S2CID 154975902.
- ^ "Environment – United Nations Population Division | Department of Economic and Social Affairs". www.un.org. Retrieved September 21, 2018.
- ^ "Family planning/Contraception". World Health Organization. Retrieved September 21, 2018.
- ^ Ohlin, G. (1967). Population control and economic development. Paris: Dev Centers, OECD.
- ^ Nielson, K. (1992). Global Justice, Capitalism and the Third World. (R.A. Wilkons, Ed.)
- ^ Waters HR, Penny ME, Creed-Kanashiro HM, Robert RC, Narro R, Willis J, et al. (July 2006). "The cost-effectiveness of a child nutrition education programme in Peru". Health Policy and Planning. 21 (4): 257–264. doi:10.1093/heapol/czl010. PMID 16672293.
- ^ Nyonator, Frank, J Koku Awooner-Williams, James Phillips, Tanya Jones, Robert Miller. (2003). The Ghana Community-based Health Planning and Services Initiative: Fostering Evidence-based Organizational Change and Development in a Resource-constrained Setting. In Policy Research Division Working Papers 180. New York: Population Council. Nyonator FK, Phillips JF, Awoonor-Williams JK, Jones TC, Miller JR. "PE Initiative: Fostering Evidence-based Organizational Change and Development in a Resource- constrained Setting" (PDF). Archived from the original (PDF) on March 11, 2012. Retrieved March 15, 2012.
- ^ Victora CG, Bahl R, Barros AJ, França GV, Horton S, Krasevec J, et al. (January 2016). "Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect". Lancet. 387 (10017): 475–490. doi:10.1016/S0140-6736(15)01024-7. hdl:10072/413175. PMID 26869575.
- ^ a b Lessen R, Kavanagh K (March 2015). "Position of the academy of nutrition and dietetics: promoting and supporting breastfeeding". Journal of the Academy of Nutrition and Dietetics. 115 (3): 444–449. doi:10.1016/j.jand.2014.12.014. PMID 25721389.
- ^ a b c d e Balogun OO, Dagvadorj A, Anigo KM, Ota E, Sasaki S (October 2015). "Factors influencing breastfeeding exclusivity during the first 6 months of life in developing countries: a quantitative and qualitative systematic review". Maternal & Child Nutrition. 11 (4): 433–451. doi:10.1111/mcn.12180. PMC 6860250. PMID 25857205.
- ^ a b c Pugh LC, Milligan RA, Frick KD, Spatz D, Bronner Y (June 2002). "Breastfeeding duration, costs, and benefits of a support program for low-income breastfeeding women". Birth. 29 (2): 95–100. doi:10.1046/j.1523-536X.2002.00169.x. PMID 12000411. S2CID 13510698.
- ^ a b c d e Cai X, Wardlaw T, Brown DW (September 2012). "Global trends in exclusive breastfeeding". International Breastfeeding Journal. 7 (1): 12. doi:10.1186/1746-4358-7-12. PMC 3512504. PMID 23020813.
- ^ "The history of the SUN Movement". United Nations. 2015. Archived from the original on October 2, 2018. Retrieved January 12, 2019.
- ^ "Outcome | Copenhagen Consensus Center". www.copenhagenconsensus.com.
- ^ European Commission Press release. June 2015. EU launches new partnership to combat Undernutrition with Bill & Melinda Gates Foundation. Accessed on November 1, 2015
- ^ FAO. 2015. Africa's Renewed Partnership to End Hunger by 2025 Archived January 28, 2020, at the Wayback Machine. Accessed on November 1, 2015.
- ^ "Goal 2: Zero Hunger".
- ^ Compact2025: Ending hunger and undernutrition. 2015. Project Paper. IFPRI: Washington, DC.
- ^ "Leadership Council". www.compact2025.org.
- ^ "Goal 2: Zero hunger". UNDP. Retrieved April 13, 2017.
- ^ "Infant and Young Child Feeding". Retrieved February 14, 2023.
- ^ United Nations, Nutrition plays key role in HIV/AIDS care, UN reports, published 25 February 2003, accessed 20 September 2023
- ^ UNICEF UK, Child Matters, Summer 2023, p. 9
- ^ "World Food Programme, Cash and Vouchers for Food" (PDF). WFP.org. April 2012. Retrieved July 5, 2014.
- ^ Foley JA, Ramankutty N, Brauman KA, Cassidy ES, Gerber JS, Johnston M, et al. (October 2011). "Solutions for a cultivated planet". Nature. 478 (7369): 337–342. Bibcode:2011Natur.478..337F. doi:10.1038/nature10452. PMID 21993620. S2CID 4346486.
- ^ a b "Division of Nutrition, Physical Activity, and Obesity, National Center for Chronic Disease Prevention and Health Promotion". June 18, 2020.
- ^ a b McCarthy, H. et al. (2012) "The development and evaluation of the screening tool for the assessment of malnutrition in Paediatrics (Stamp©) for use by Healthcare staff," Journal of Human Nutrition and Dietetics, 25(4), pp. 311–318. Available at: https://doi.org/10.1111/j.1365-277x.2012.01234.x.
- ^ Das JK, Salam RA, Saeed M, Kazmi FA, Bhutta ZA (2020). "Effectiveness of interventions to manage acute malnutrition in children under 5 years of age in low- and middle-income countries: A systematic review". Campbell Systematic Reviews. 16 (2): e1082. doi:10.1002/cl2.1082. PMC 8356333. PMID 37131422. S2CID 242985650.
- ^ "Child growth". www.who.int. Retrieved October 17, 2023.
- ^ a b Taylor, Melissa; Tapkigen, Janet; Ali, Israa; Liu, Qin; Long, Qian; Nabwera, Helen (October 12, 2023). Cochrane Developmental, Psychosocial and Learning Problems Group (ed.). "The impact of growth monitoring and promotion on health indicators in children under five years of age in low- and middle-income countries". Cochrane Database of Systematic Reviews. 2023 (10): CD014785. doi:10.1002/14651858.CD014785.pub2. PMC 10568659. PMID 37823471.
- ^ a b Ann Ashworth (2003). Guidelines for the inpatient treatment of severely malnourished children. Geneva: World Health Organization. ISBN 978-92-4-154609-6.
- ^ a b c d "8. Management of diarrhoea with severe malnutrition" (PDF). The Treatment of diarrhoea: a manual for physicians and other senior health workers (4 ed.). Geneva: World Health Organization. 2005. pp. 22–24. ISBN 978-92-4-159318-2.
- ^ Bally MR, Blaser Yildirim PZ, Bounoure L, Gloy VL, Mueller B, Briel M, Schuetz P (January 2016). "Nutritional Support and Outcomes in Malnourished Medical Inpatients: A Systematic Review and Meta-analysis". JAMA Internal Medicine. 176 (1): 43–53. doi:10.1001/jamainternmed.2015.6587. PMID 26720894.
- ^ a b c d e f g h National Guidelines for the Management of Severely Malnourished Children in Bangladesh Archived October 19, 2011, at the Wayback Machine, Institute of Public Health Nutrition, Directorate General of Health Services, Ministry of Health and Family Welfare, Government of the People's Republic of Bangladesh, May 2008, page 18 (19 in PDF) and following pages.
- ^ Sguassero Y, de Onis M, Bonotti AM, Carroli G (June 2012). "Community-based supplementary feeding for promoting the growth of children under five years of age in low and middle income countries". The Cochrane Database of Systematic Reviews. 2012 (6): CD005039. doi:10.1002/14651858.CD005039.pub3. PMC 8078353. PMID 22696347.
- ^ Kristjansson E, Francis DK, Liberato S, Benkhalti Jandu M, Welch V, Batal M, et al. (March 2015). "Food supplementation for improving the physical and psychosocial health of socio-economically disadvantaged children aged three months to five years". The Cochrane Database of Systematic Reviews. 11 (3): CD009924. doi:10.4073/csr.2015.11. PMC 6885042. PMID 25739460.
- ^ Lazzerini M, Rubert L, Pani P (June 2013). "Specially formulated foods for treating children with moderate acute malnutrition in low- and middle-income countries". The Cochrane Database of Systematic Reviews (6): CD009584. doi:10.1002/14651858.CD009584.pub2. PMID 23794237.
- ^ a b Anderson T (June 24, 2009). "Firms target nutrition for the poor". BBC News.
- ^ Schoonees A, Lombard MJ, Musekiwa A, Nel E, Volmink J (May 2019). "Ready-to-use therapeutic food (RUTF) for home-based nutritional rehabilitation of severe acute malnutrition in children from six months to five years of age". The Cochrane Database of Systematic Reviews. 2019 (5): CD009000. doi:10.1002/14651858.CD009000.pub3. PMC 6537457. PMID 31090070.
- ^ a b c Viana L, Burgos MG, Silva R (January–March 2012). "Refeeding syndrome: clinical and nutritional relevance". Arquivos Brasileiros de Cirurgia Digestiva. 25 (1): 56–59. doi:10.1590/s0102-67202012000100013. PMID 22569981.
- ^ Boateng AA, Sriram K, Meguid MM, Crook M (February 2010). "Refeeding syndrome: treatment considerations based on collective analysis of literature case reports". Nutrition. 26 (2): 156–167. doi:10.1016/j.nut.2009.11.017. PMID 20122539.
- ^ Kristof ND (December 4, 2008). "Raising the world's IQ". The New York Times.
- ^ a b c d e f g The Treatment of Diarrhoea: A manual for physicians and other senior health workers, World Health Organization, 2005. See especially Ch. 4 "Management of Acute Diarrhoea (Without Blood)" and Ch. 8 "Management of Diarrhoea With Severe Malnutrition."
- ^ a b "4. Management of acute diarrhoea without blood" (PDF). The Treatment of diarrhoea : a manual for physicians and other senior health workers (4 ed.). Geneva: World Health Organization. 2005. pp. 8–16. ISBN 978-92-4-159318-2.
- ^ Victora CG, Bryce J, Fontaine O, Monasch R (January 2000). "Reducing deaths from diarrhoea through oral rehydration therapy". Bulletin of the World Health Organization. 78 (10): 1246–1255. hdl:10665/268000. PMC 2560623. PMID 11100619.
- ^ "WHO Drug Information Vol. 16, No. 2, 2002: Current Topics: New formula oral rehydration salts". September 23, 2012. Archived from the original on September 23, 2012.
- ^ Low-osmolarity oral rehydration solution (ORS), Rehydrate Project, updated: April 23, 2014.
- ^ The Treatment of Diarrhoea: A manual for physicians and other senior health workers, WHO, 2005. Specifically, 45 milliliters of potassium chloride solution from a stock solution containing 100g KCl per liter, along with one packet of ORS, two liters of water, and 50 grams of sucrose. And please remember, sucrose has approximately twice the molecular weight of glucose, with one mole of glucose weighing 180 g and one mole of sucrose weighing 342 g.
- ^ "Guidelines for the control of shigellosis, including epidemics due to Shigella dysenteriae type 1". World Health Organization, 2005, Annex 12 – Preparation of Home Made Oral Rehydration Solution, p. 51 (57 in PDF): "Ingredients: Half a teaspoon of salt (2.5 grams), six level teaspoons of sugar (30 grams) and one litre of safe drinking water".
- ^ "Dehydration, treatments and drugs." Mayo Clinic January 7, 2011. "In an emergency situation where a pre-formulated solution is unavailable, you can make your own oral rehydration solution by mixing half teaspoon salt, six level teaspoons of sugar and one litre (about 1 quart) of safe drinking water."
- ^ Family Practice Notebook, Oral Rehydration Solution, Scott Moses, MD, February 1, 2014.
- ^ National Guidelines for the Management of Severely Malnourished Children in Bangladesh Archived October 19, 2011, at the Wayback Machine recommends, for initial hypoglycemia, a 50 milliliter bolus of 10% glucose or sucrose. This can also be achieved by added 1 rounded teaspoon of sugar to 10.5 teaspoons of water (which is 3.5 tablespoons of water).
- ^ "Mortality and Burden of Disease Estimates for WHO Member States in 2002" (xls). World Health Organization. 2002.
- ^ "Global hunger worsening, warns UN". BBC (Europe). October 14, 2009. Retrieved August 22, 2010.
- ^ K. von Grebmer, J. Bernstein, A. de Waal, N. Prasai, S. Yin, Y. Yohannes: 2015 Global Hunger Index – Armed Conflict and the Challenge of Hunger. Bonn, Washington DC, Dublin: Welthungerhilfe, IFPRI, and Concern Worldwide. October 2015.
- ^ Jean Ziegler. "Promotion And Protection Of All Human Rights, Civil, Political, Economic, Social And Cultural Rights, Including The Right To Development: Report of the Special Rapporteur on the right to food, Jean Ziegler". Human Rights Council of the United Nations, January 10, 2008."According to the Food and Agriculture Organization of the United Nations (FAO), the world already produces enough food to feed every child, woman and man and could feed 12 billion people, or double the current world population."
- ^ Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. (December 2012). "Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2197–2223. doi:10.1016/S0140-6736(12)61689-4. PMID 23245608. S2CID 205967479.
- ^ "Putting a number on hunger". Putting a number on hunger. Retrieved September 4, 2024.
- ^ "The State of Food Insecurity in the World 2006". Food and Agricultural Organization of the United Nations. Retrieved April 6, 2019.
- ^ "The State of Food Insecurity in the World 2008". Food and Agricultural Organization of the United Nations. Retrieved April 6, 2019.
- ^ "The State of Food Insecurity in the World 2015" (PDF). Food and Agricultural Organization of the United Nations. Retrieved April 6, 2019.
- ^ a b Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. (December 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2095–2128. doi:10.1016/S0140-6736(12)61728-0. hdl:10536/DRO/DU:30050819. PMC 10790329. PMID 23245604. S2CID 1541253.
- ^ Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. (December 2012). "A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2224–2260. doi:10.1016/S0140-6736(12)61766-8. PMC 4156511. PMID 23245609.
- ^ a b "Malnutrition The Starvelings". The Economist. January 24, 2008.
- ^ "U.N. chief: Hunger kills 17,000 kids daily". CNN. November 17, 2009.
- ^ a b Joshua Ruxin (1996). "Hunger, Science, and Politics: FAO, WHO, and Unicef Nutrition Policies, 1945–1978" (PDF). University College London. Retrieved January 12, 2019.
- ^ a b James Vernon (2007). Hunger: A Modern History. Harvard University Press. pp. 81–140, passim. ISBN 978-0-674-02678-0.
- ^ Grigg D (1981). "The historiography of hunger: changing views on the world food problem, 1945–1980". Transactions. NS. 6 (3): 279–292. Bibcode:1981TrIBG...6..279G. doi:10.2307/622288. JSTOR 622288. PMID 12265450.
Before 1945 very little academic or political notice was taken of the problem of world hunger, since 1945 there has been a vast literature on the subject.
- ^ "Universal Declaration of Human Rights". www.un.org. October 6, 2015. Retrieved February 24, 2018.
- ^ "What is the Right to Food? | Right to food". www.righttofood.org. Retrieved February 24, 2018.
- ^ "Universal Declaration on the Eradication of Hunger and Malnutrition". Archived from the original on October 8, 2018. Retrieved February 24, 2018.
- ^ "American Convention on Human Rights". www.hrcr.org. Retrieved March 17, 2018.
- ^ "Rome Declaration and Plan of Action". www.fao.org. Retrieved March 17, 2018.
- ^ Black RE, Allen LH, Bhutta ZA, Caulfield LE, de Onis M, Ezzati M, et al. (January 2008). "Maternal and child undernutrition: global and regional exposures and health consequences". Lancet. 371 (9608): 243–260. doi:10.1016/S0140-6736(07)61690-0. PMID 18207566. S2CID 3910132.
- ^ Tomkins, A., 2014. Tackling undernutrition in children – new opportunities for innovation and action. Paediatrics and International Child Health, 34(4), pp.235–238.
- ^ Mupunga, I., Mngqawa, P. and Katerere, D., 2017. Peanuts, Aflatoxins and Undernutrition in Children in Sub-Saharan Africa. Nutrients, 9(12), p.1287.
- ^ Trehan I, Goldbach HS, LaGrone LN, Meuli GJ, Wang RJ, Maleta KM, Manary MJ (January 2013). "Antibiotics as part of the management of severe acute malnutrition". The New England Journal of Medicine. 368 (5): 425–435. doi:10.1056/NEJMoa1202851. PMC 3654668. PMID 23363496.
The addition of antibiotics to therapeutic regimens for uncomplicated severe acute malnutrition was associated with a significant improvement in recovery and mortality rates.
- ^ Caulfield, L., de Onis, M., Blössner, M. and Black, R., 2004. Undernutrition as an underlying cause of child deaths associated with diarrhea, pneumonia, malaria, and measles. The American Journal of Clinical Nutrition, 80(1), pp.193–198.
- ^ Prüss-Üstün, A., Bos, R., Gore, F., Bartram, J. (2008). Safer water, better health – Costs, benefits and sustainability of interventions to protect and promote health. World Health Organization (WHO), Geneva, Switzerland
- ^ Collins, S., Sadler, K., Bahwere, P. and Hallam, A., 2007. Management of severe acute malnutrition in children – Authors' reply. The Lancet, 369(9563), p.741.
- ^ a b c d e Moumen, Hana (February 24, 2023). "Undernourished and Overlooked". UNICEF DATA. Retrieved November 8, 2023.
- ^ a b c d e f g Nubé M, Van Den Boom GJ (2003). "Gender and adult undernutrition in developing countries". Annals of Human Biology. 30 (5): 520–537. doi:10.1080/0301446031000119601. PMID 12959894. S2CID 25229403.
- ^ a b c Dewan M (2008). "Malnutrition in Women" (PDF). Studies on Home and Community Science. 2 (1): 7–10. doi:10.1080/09737189.2008.11885247. S2CID 39557892. Retrieved March 3, 2014.
- ^ Najma Rizvi (March 2013). "Enduring misery". dandc.eu.
- ^ Carter RB. "Survey Reveals High Malnutrition Rates Among Pregnant Women in Kenya". UNICEF. Archived from the original on March 28, 2014. Retrieved March 3, 2014.
- ^ a b c d e "Gender and Nutrition 2001". Food and Agriculture of the United Nations. July 2001. Retrieved August 22, 2016.
- ^ Bhutta ZA, Ahmed T, Black RE, Cousens S, Dewey K, Giugliani E, et al. (February 2008). "What works? Interventions for maternal and child undernutrition and survival". Lancet. 371 (9610): 417–440. doi:10.1016/S0140-6736(07)61693-6. PMID 18206226. S2CID 18345055.
- ^ Denis Campbell (October 14, 2014). "Folic acid to be added to UK flour in effort to reduce birth defects". The Guardian. Retrieved October 15, 2018.
- ^ "Nutrition Education". Action for Healthy Kids.
- ^ "Team Nutrition MyPlate eBooks".
- ^ a b Kvamme JM, Olsen JA, Florholmen J, Jacobsen BK (May 2011). "Risk of malnutrition and health-related quality of life in community-living elderly men and women: the Tromsø study". Quality of Life Research. 20 (4): 575–582. doi:10.1007/s11136-010-9788-0. PMC 3075394. PMID 21076942.
- ^ a b c d Wellman NS, Weddle DO, Kranz S, Brain CT (October 1997). "Elder insecurities: poverty, hunger, and malnutrition". Journal of the American Dietetic Association. 97 (10 Suppl 2): S120–S122. doi:10.1016/S0002-8223(97)00744-X. PMID 9336570.
- ^ a b c Saka B, Kaya O, Ozturk GB, Erten N, Karan MA (December 2010). "Malnutrition in the elderly and its relationship with other geriatric syndromes". Clinical Nutrition. 29 (6): 745–748. doi:10.1016/j.clnu.2010.04.006. PMID 20627486.
- ^ a b Volkert D (2002). "Malnutrition in the elderly – prevalence, causes and corrective strategies". Clinical Nutrition. 21: 110–112. doi:10.1016/S0261-5614(02)80014-0.
- ^ Volkert D (2002). "Malnutrition in the elderly – prevalence, causes and corrective strategies". Clinical Nutrition. 21: 110–112. doi:10.1016/S0261-5614(02)80014-0.
- ^ a b Milne AC, Potter J, Vivanti A, Avenell A (April 2009). "Protein and energy supplementation in elderly people at risk from malnutrition". The Cochrane Database of Systematic Reviews. 2009 (2): CD003288. doi:10.1002/14651858.CD003288.pub3. PMC 7144819. PMID 19370584.
- ^ Mamhidir AG, Kihlgren M, Soerlie V (June 2010). "Malnutrition in elder care: qualitative analysis of ethical perceptions of politicians and civil servants". BMC Medical Ethics. 11: 11. doi:10.1186/1472-6939-11-11. PMC 2927875. PMID 20553607.
- ^ "Care crisis triggers rise in malnutrition, charities claim". Home care Insight. August 19, 2019. Retrieved October 1, 2019.
- ^ Bolin T, Bare M, Caplan G, Daniells S, Holyday M (2010). "Malabsorption may contribute to malnutrition in the elderly". Nutrition. 26 (7–8): 852–853. doi:10.1016/j.nut.2009.11.016. PMID 20097534.
