Q fever
| Q fever | |
|---|---|
| Other names | Query fever, coxiellosis[1][2] |
 | |
| Immunohistochemical detection of C. burnetii in resected cardiac valve of a 60-year-old man with Q fever endocarditis, Cayenne, French Guiana: Monoclonal antibodies against C. burnetii and hematoxylin were used for staining; original magnification is ×50. | |
| Specialty | Infectious diseases |
| Types | acute, chronic[1] |
| Risk factors | Contact with livestock[2] |
| Differential diagnosis | pneumonia, influenza, brucellosis, leptospirosis, meningitis, viral hepatitis, dengue fever, malaria, other rickettsial infections[2] |
Q fever or query fever is a disease caused by infection with Coxiella burnetii,[1][3][4] a bacterium that affects humans and other animals. This organism is uncommon, but may be found in cattle, sheep, goats, and other domestic mammals, including cats and dogs. The infection results from inhalation of a spore-like small-cell variant, and from contact with the milk, urine, feces, vaginal mucus, or semen of infected animals. Rarely, the disease is tick-borne.[5] The incubation period can range from 9 to 40 days. Humans are vulnerable to Q fever, and infection can result from even a few organisms.[5] The bacterium is an obligate intracellular pathogenic parasite.
Signs and symptoms
[edit]The incubation period is usually two to three weeks.[6] The most common manifestation is flu-like symptoms: abrupt onset of fever, malaise, profuse perspiration, severe headache, muscle pain, joint pain, loss of appetite, upper respiratory problems, dry cough, pleuritic pain, chills, confusion, and gastrointestinal symptoms, such as nausea, vomiting, and diarrhea. About half of infected individuals exhibit no symptoms.[6]
During its course, the disease can progress to an atypical pneumonia, which can result in a life-threatening acute respiratory distress syndrome, usually occurring during the first four to five days of infection.[7]
Less often, Q fever causes (granulomatous) hepatitis, which may be asymptomatic or become symptomatic with malaise, fever, liver enlargement, and pain in the right upper quadrant of the abdomen. This hepatitis often results in the elevation of transaminase values, although jaundice is uncommon. Q fever can also rarely result in retinal vasculitis.[8]
The chronic form of Q fever is virtually identical to endocarditis (i.e. inflammation of the inner lining of the heart),[9] which can occur months or decades following the infection. It is usually fatal if untreated. However, with appropriate treatment, the mortality falls to around 10%.[citation needed]
A minority of Q fever survivors develops Q fever fatigue syndrome after acute infection, one of the more well-studied post-acute infection syndromes. Q fever fatigue syndrome is characterised by post-exertional malaise and debilitating fatigue. People with Q fever fatigue syndrome frequently meet the diagnostic criteria for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Symptoms often persist years after the initial infection.[10]
Diagnosis
[edit]
Diagnosis is usually based on serology[11][12] (looking for an antibody response) rather than looking for the organism itself. Serology allows the detection of chronic infection by the appearance of high levels of the antibody against the virulent form of the bacterium. Molecular detection of bacterial DNA is increasingly used. Contrary to most obligate intracellular parasites, Coxiella burnetii can be grown in an axenic culture, but its culture is technically difficult and not routinely available in most microbiology laboratories.[13]
Q fever can cause endocarditis (infection of the heart valves) which may require transoesophageal echocardiography to diagnose. Q fever hepatitis manifests as an elevation of alanine transaminase and aspartate transaminase, but a definitive diagnosis is only possible on liver biopsy, which shows the characteristic fibrin ring granulomas.[14]
Prevention
[edit]Research done in the 1960s–1970s by French Canadian-American microbiologist and virologist Paul Fiset was instrumental in the development of the first successful Q fever vaccine.[15]
Protection is offered by Q-Vax, a whole-cell, inactivated vaccine developed by an Australian vaccine manufacturing company, CSL Limited.[16] The intradermal vaccination is composed of killed C. burnetii organisms. Skin and blood tests should be done before vaccination to identify pre-existing immunity, because vaccinating people who already have immunity can result in a severe local reaction. After a single dose of vaccine, protective immunity lasts for many years. Revaccination is not generally required. Annual screening is typically recommended.[17]
In 2001, Australia introduced a national Q fever vaccination program for people working in "at risk" occupations. Vaccinated or previously exposed people may have their status recorded on the Australian Q Fever Register,[18] which may be a condition of employment in the meat processing industry or in veterinary research.[19] An earlier killed vaccine had been developed in the Soviet Union, but its side effects prevented its licensing abroad.[citation needed]
Preliminary results suggest vaccination of animals may be a method of control. Published trials proved that use of a registered phase vaccine (Coxevac) on infected farms is a tool of major interest to manage or prevent early or late abortion, repeat breeding, anoestrus, silent oestrus, metritis, and decreases in milk yield when C. burnetii is the major cause of these problems.[20][21]
Treatment
[edit]Treatment of acute Q fever with antibiotics is very effective.[7] Commonly used antibiotics include doxycycline, tetracycline, chloramphenicol, ciprofloxacin, and ofloxacin; the antimalarial drug hydroxychloroquine is also used.[7] Chronic Q fever is more difficult to treat and can require up to four years of treatment with doxycycline and quinolones or doxycycline with hydroxychloroquine.[7] If a person has chronic Q fever, doxycycline and hydroxychloroquine will be prescribed for at least 18 months. Q fever in pregnancy is especially difficult to treat because doxycycline and ciprofloxacin are contraindicated in pregnancy. The preferred treatment for pregnancy and children under the age of eight is co-trimoxazole.[22][23]
Epidemiology
[edit]
Q fever is a globally distributed zoonotic disease caused by a highly sustainable and virulent bacterium. The pathogenic agent is found worldwide, with the exception of New Zealand[24] and Antarctica.[25] Understanding the transmission and risk factors of Q fever is crucial for public health due to its potential to cause widespread infection.
Transmission and occupational risks
[edit]Transmission primarily occurs through the inhalation of contaminated dust, contact with contaminated milk, meat, or wool, and particularly birthing products. Ticks can transfer the pathogenic agent to other animals. While human-to-human transmission is rare, often associated with the transmission of birth products, sexual contact, and blood transfusion,[25] certain occupations pose higher risks for Q fever:[26]
- Veterinary personnel
- Stockyard workers
- Farmers
- Sheep shearers
- Animal transporters
- Laboratory workers handling potentially infected veterinary samples or visiting abattoirs
- People who cull and process kangaroos
- Hide (tannery) workers
It is important to note that anyone who has contact with animals infected with Q fever bacteria, especially people who work on farms or with animals, is at an increased risk of contracting the disease.[27] Understanding these occupational risks is crucial for public health.
Prevalence and risk factors
[edit]Studies indicate a higher prevalence of Q fever in men than in women,[28][29] potentially linked to occupational exposure rates.[30] Other contributing risk factors include geography, age, and occupational exposure. Diagnosis relies on blood compatibility testing, with treatment varying for acute and chronic cases. Acute disease often responds to doxycycline, while chronic cases may require a combination of doxycycline and hydroxychloroquine.[31] It is worth noting that Q fever was officially reported in the United States as a notifiable disease in 1999 due to its potential biowarfare agent status.[32]
Q fever exhibits global epidemiological patterns, with higher incidence rates reported in certain countries. In Africa, wild animals in rainforests primarily transmit the disease, making it endemic.[25] Unique patterns are observed in Latin America, but reporting is sporadic and inconsistent between and among countries, making it difficult to track and address.[33]
Recent outbreaks in European countries, including the Netherlands and France, have been linked to urbanized goat farming, raising concerns about the safety of intensive livestock farming practices and the potential risks of zoonotic diseases. Similarly, in the United States, Q fever is more common in livestock farming regions, especially in the West and the Great Plains. California, Texas, and Iowa account for almost 40% of reported cases, with a higher incidence during the spring and early summer when livestock are breeding, regardless of whether the infection is acute or chronic.[27]
These outbreaks have affected a significant number of people, with immunocompromised individuals being more severely impacted.[32] The global nature of Q fever and its association with livestock farming highlight the importance of implementing measures to prevent and control the spread of the disease, particularly in high-risk regions.
Age and occupational exposure
[edit]Older men in the West and Great Plains regions, involved in close contact with livestock management, are at a higher risk of contracting chronic Q fever.[30] This risk may be further increased for those with a history of cardiac problems.[30] The disease can manifest years after the initial infection, presenting symptoms such as non-specific fatigue, fever, weight loss, and endocarditis.[25][30] Additionally, certain populations have been found to be more vulnerable to Q fever, including children living in farming communities, who may experience similar symptoms as adults.[34] There have also been reported cases of Q fever among United States military service members,[35] particularly those deployed to Iraq or Afghanistan, which further highlights the importance of understanding and addressing the occupational risks associated with Q fever.[36]
Prevention and public health education
[edit]Proper public health education is crucial in reducing the number of Q fever cases. Raising awareness about transmission routes, occupational risks, and preventive measures,[32] such as eliminating unpasteurized milk products from the diet, can help prevent the spread of disease.[37]
Interdisciplinary collaboration between medical personnel and farmers is critical when developing strategies for control and prevention in a community.[38] Awareness campaigns should particularly target occupations that work with livestock, focusing on risk-reduction procedures such as herd monitoring, implementing sanitation practices and personal protective equipment, and vaccinating animals.[38] Locating livestock farms at least 500 meters away from residential areas can also help reduce animal-to-human transmission.[38]
History
[edit]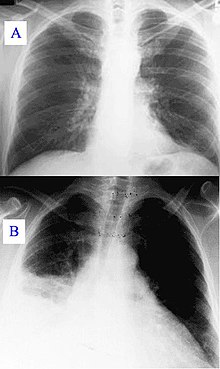
Q fever was first described in 1935 by Edward Holbrook Derrick[39] in slaughterhouse workers in Brisbane, Queensland. The "Q" stands for "query" and was applied at a time when the causative agent was unknown; it was chosen over suggestions of abattoir fever and Queensland rickettsial fever, to avoid directing negative connotations at either the cattle industry or the state of Queensland.[40]
The pathogen of Q fever was discovered in 1937, when Frank Macfarlane Burnet and Mavis Freeman isolated the bacterium from one of Derrick's patients.[41] It was originally identified as a species of Rickettsia. H.R. Cox and Gordon Davis elucidated the transmission when they isolated it from ticks found in the US state of Montana in 1938.[42] It is a zoonotic disease whose most common animal reservoirs are cattle, sheep, and goats. Coxiella burnetii – named for Cox and Burnet – is no longer regarded as closely related to the Rickettsiae, but as similar to Legionella and Francisella, and is a Gammaproteobacterium.[citation needed]
Society and culture
[edit]An early mention of Q fever was important in one of the early Dr. Kildare films (1939, Calling Dr. Kildare). Kildare's mentor Dr. Gillespie (Lionel Barrymore) tires of his protégé working fruitlessly on "exotic diagnoses" ("I think it's Q fever!") and sends him to work in a neighborhood clinic, instead.[43][44]
Biological warfare
[edit]C. burnetii has been used to develop biological weapons.[45]
The United States investigated it as a potential biological warfare agent in the 1950s, with eventual standardization as agent OU. At Fort Detrick and Dugway Proving Ground, human trials were conducted on Whitecoat volunteers to determine the median infective dose (18 MICLD50/person i.h.) and course of infection. The Deseret Test Center dispensed biological Agent OU with ships and aircraft, during Project 112 and Project SHAD.[46] As a standardized biological, it was manufactured in large quantities at Pine Bluff Arsenal, with 5,098 gallons in the arsenal in bulk at the time of demilitarization in 1970.[citation needed]
C. burnetii is currently ranked as a "category B" bioterrorism agent by the CDC.[47] It can be contagious, and is very stable in aerosols in a wide range of temperatures. Q fever microorganisms may survive on surfaces up to 60 days. It is considered a good agent in part because its ID50 (number of bacilli needed to infect 50% of individuals) is considered to be one, making it the lowest known.[dubious – discuss]
In animals
[edit]Q fever can affect many species of domestic and wild animals, including ruminants (cattle, sheep, goats, bison,[48] deer species[49][50]...), carnivores (dogs, cats,[51] seals[52]...), rodents,[53] reptiles and birds. However, ruminants (cattle, goats, and sheep) are the most frequently affected animals, and can serve as a reservoir for the bacteria.[54]
Clinical signs
[edit]In contrast to humans, though a respiratory and cardiac infection could be experimentally reproduced in cattle,[55] the clinical signs mainly affect the reproductive system. Q fever in ruminants is, therefore, mainly responsible for abortions, metritis, retained placenta, and infertility.
The clinical signs vary between species. In small ruminants (sheep and goats), it is dominated by abortions, premature births, stillbirths, and the birth of weak lambs or kids. One of the characteristics of abortions in goats is that they are very frequent and clustered in the first year or two after contamination of the farm. This is known as an abortion storm.[56]
In cattle, although abortions also occur, they are less frequent and more sporadic. The clinical picture is rather dominated by nonspecific signs such as placental retentions, metritis, and consequent fertility disorders.[57][58][59]
Epidemiology
[edit]With the exception of New Zealand, which is currently free of Q fever, the disease is present throughout the world. Numerous epidemiological surveys have been carried out. They have shown that about one in three cattle farms and one in four sheep or goat farms are infected,[60] but wide variations are seen between studies and countries. In China, Iran, Great Britain, Germany, Hungary, the Netherlands, Spain, the US, Belgium, Denmark, Croatia, Slovakia, the Czech Republic, Serbia, Slovenia, and Jordan, for example, more than 50% of cattle herds were infected with Q fever.[61][62][63][64][65][66][67]
Infected animals shed the bacteria by three routes - genital discharge, faeces, and milk.[68] Excretion is greatest at the time of parturition or abortion, and placentas and aborted fetuses are the main sources of bacteria, particularly in goats.
As C. burnetii is small and resistant in the environment, it is easily airborne and can be transmitted from one farm to another, even if several kilometres away.[69]
Control
[edit]Biosecurity measures
[edit]Based on the epidemiological data, biosecurity measures can be derived:[70]
- The spread of manure from infected farm should be avoided in windy conditions
- The level of hygiene must be very high during parturition and fetal annexes, and fetuses must be collected and destroyed as soon as possible
Medical measures
[edit]A vaccine for cattle, goats and sheep exists. It reduces clinical expression such as abortions and decreases excretion of the bacteria by the animals leading to control of Q fever in herds.[71]
In addition, vaccination of herds against Q fever has been shown to reduce the risk of human infection.[72]
References
[edit]- ^ a b c "Epidemiology and Statistics | Q Fever | CDC". www.cdc.gov. 2019-09-16. Archived from the original on 2020-05-29. Retrieved 2020-05-27.
- ^ a b c National Organization for Rare Disorders (2003). "Q Fever". NORD Guide to Rare Disorders. Lippincott Williams & Wilkins. p. 293. ISBN 978-0-7817-3063-1.
- ^ Beare PA, Samuel JE, Howe D, Virtaneva K, Porcella SF, Heinzen RA (April 2006). "Genetic diversity of the Q fever agent, Coxiella burnetii, assessed by microarray-based whole-genome comparisons". Journal of Bacteriology. 188 (7): 2309–2324. doi:10.1128/JB.188.7.2309-2324.2006. PMC 1428397. PMID 16547017.
- ^ "Q fever | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". Genetic and Rare Diseases Information Center. Archived from the original on 2018-04-18. Retrieved 2018-04-17.
- ^ a b "Q Fever | CDC". Centers for Disease Control and Prevention. 2017-12-27. Archived from the original on 2018-04-18. Retrieved 2018-04-17.
- ^ a b Anderson A (2011). "Q Fever". In Brunette GW, McQuiston J, et al. (eds.). CDC Health Information for International Travel: The Yellow Book. Oxford University Press. p. 270. ISBN 978-0-19-976901-8.
- ^ a b c d "Coxiella/Q Fever". The Lecturio Medical Concept Library. Archived from the original on 2021-05-15. Retrieved 7 July 2021.
- ^ Kuhne F, Morlat P, Riss I, Dominguez M, Hostyn P, Carniel N, et al. (1992). "[Is A29, B12 vasculitis caused by the Q fever agent? (Coxiella burnetii)]" [Is A29, B12 vasculitis caused by the Q fever agent? (Coxiella burnetii)]. Journal Français d'Ophtalmologie (in French). 15 (5): 315–321. OCLC 116712679. PMID 1430809.
- ^ Karakousis PC, Trucksis M, Dumler JS (June 2006). "Chronic Q fever in the United States". Journal of Clinical Microbiology. 44 (6): 2283–2287. doi:10.1128/JCM.02365-05. PMC 1489455. PMID 16757641.
- ^ Choutka J, Jansari V, Hornig M, Iwasaki A (May 2022). "Unexplained post-acute infection syndromes". Nature Medicine. 28 (5): 911–923. doi:10.1038/s41591-022-01810-6. PMID 35585196. S2CID 248889597.
- ^ Maurin M, Raoult D (October 1999). "Q fever". Clinical Microbiology Reviews. 12 (4): 518–553. doi:10.1128/CMR.12.4.518. PMC 88923. PMID 10515901.
- ^ Scola BL (October 2002). "Current laboratory diagnosis of Q fever". Seminars in Pediatric Infectious Diseases. 13 (4): 257–262. doi:10.1053/spid.2002.127199. PMID 12491231.
- ^ Omsland A, Cockrell DC, Howe D, Fischer ER, Virtaneva K, Sturdevant DE, et al. (March 2009). "Host cell-free growth of the Q fever bacterium Coxiella burnetii". Proceedings of the National Academy of Sciences of the United States of America. 106 (11): 4430–4434. Bibcode:2009PNAS..106.4430O. doi:10.1073/pnas.0812074106. PMC 2657411. PMID 19246385.
- ^ van de Veerdonk FL, Schneeberger PM (May 2006). "Patient with fever and diarrhea". Clinical Infectious Diseases. 42 (7): 1051–2. doi:10.1086/501027.
- ^ Saxon W (March 8, 2001). "Dr. Paul Fiset, 78, Microbiologist And Developer of Q Fever Vaccine". The New York Times. p. C-17. Archived from the original on 2015-05-27. Retrieved 2022-01-28.
- ^ "Q fever Vaccine" (PDF). CSL Limited. 17 January 2014. Archived from the original (PDF) on 9 March 2017. Retrieved 11 July 2015.
- ^ "USCF communicable disease prevention program animal exposure surveillance program" (PDF). Archived from the original (PDF) on 2007-07-01. Retrieved 2007-05-08.
- ^ "Australian Q Fever Register". AusVet. Archived from the original on 2016-02-16. Retrieved 12 February 2016.
- ^ "Q-Fever Vaccinations". Faculty of Veterinary and Agricultural Sciences | The University of Melbourne. 2019-11-20. Archived from the original on 2019-06-25. Retrieved 2020-07-11.
- ^ Camuset P, Remmy D (2008). Q Fever (Coxiella burnetii) Eradication in a Dairy Herd by Using Vaccination with a Phase 1 Vaccine. XXV World Buiatrics Congress. Budapest.
- ^ Hogerwerf L, van den Brom R, Roest HI, Bouma A, Vellema P, Pieterse M, et al. (March 2011). "Reduction of Coxiella burnetii prevalence by vaccination of goats and sheep, The Netherlands". Emerging Infectious Diseases. 17 (3): 379–386. doi:10.3201/eid1703.101157. PMC 3166012. PMID 21392427.
- ^ Carcopino X, Raoult D, Bretelle F, Boubli L, Stein A (September 2007). "Managing Q fever during pregnancy: the benefits of long-term cotrimoxazole therapy". Clinical Infectious Diseases. 45 (5): 548–555. doi:10.1086/520661. PMID 17682987.
- ^ "Query Fever - MARI REF". Misdiagnosis Association and Research Institute. 20 July 2021. Archived from the original on 2021-08-27. Retrieved 2021-08-27.
- ^ Cutler SJ, Bouzid M, Cutler RR (April 2007). "Q fever". The Journal of Infection. 54 (4): 313–318. doi:10.1016/j.jinf.2006.10.048. PMID 17147957.
- ^ a b c d Salifu SP, Bukari AR, Frangoulidis D, Wheelhouse N (2019-05-01). "Current perspectives on the transmission of Q fever: Highlighting the need for a systematic molecular approach for a neglected disease in Africa". Acta Tropica. 193: 99–105. doi:10.1016/j.actatropica.2019.02.032. ISSN 0001-706X. PMID 30831112. S2CID 73461378.
- ^ "Q fever: MedlinePlus Medical Encyclopedia". MedlinePlus. Archived from the original on 2016-07-28. Retrieved 2018-04-17.
- ^ a b CDC (2021-08-06). "Q fever epidemiology and statistics | CDC". Centers for Disease Control and Prevention. Retrieved 2023-11-21.
- ^ Domingo P, Muñoz C, Franquet T, Gurguí M, Sancho F, Vazquez G (October 1999). "Acute Q fever in adult patients: report on 63 sporadic cases in an urban area". Clinical Infectious Diseases. 29 (4): 874–879. doi:10.1086/520452. PMID 10589906.
- ^ Dupuis G, Petite J, Péter O, Vouilloz M (June 1987). "An important outbreak of human Q fever in a Swiss Alpine valley". International Journal of Epidemiology. 16 (2): 282–287. doi:10.1093/ije/16.2.282. PMID 3301708.
- ^ a b c d "Epidemiology and Statistics | Q Fever | CDC". www.cdc.gov. 2019-09-16. Archived from the original on 2020-05-29. Retrieved 2020-05-27.
- ^ Hartzell JD, Wood-Morris RN, Martinez LJ, Trotta RF (May 2008). "Q Fever: Epidemiology, Diagnosis, and Treatment". Mayo Clinic Proceedings. 83 (5): 574–579. doi:10.4065/83.5.574. ISSN 0025-6196. PMID 18452690.
- ^ a b c Patil SM, Regunath H (2023), "Q Fever", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 32310555, retrieved 2023-11-21
- ^ Fernandes J, Sampaio de Lemos ER (2023-04-01). "The multifaceted Q fever epidemiology: a call to implement One Health approach in Latin America". The Lancet Regional Health - Americas. 20: 100463. doi:10.1016/j.lana.2023.100463. ISSN 2667-193X. PMC 10006848. PMID 36915670.
- ^ Bwatota SF, Cook EA, de Clare Bronsvoort BM, Wheelhouse N, Hernandez-Castor LE, Shirima GM (2022-11-17). "Epidemiology of Q-fever in domestic ruminants and humans in Africa. A systematic review". CABI One Health. doi:10.1079/cabionehealth.2022.0008. hdl:20.500.11820/8b572652-80f8-4983-a0f0-c2586c7d1b9e. ISSN 2791-223X. S2CID 253662234.
- ^ Anderson AD, Smoak B, Shuping E, Ockenhouse C, Petruccelli B. "Q Fever and the US Military - Volume 11, Number 8—August 2005 - Emerging Infectious Diseases journal - CDC". doi:10.3201/eid1108.050314.
- ^ Hartzell J (May 2008). "Q Fever: Epidemiology, Diagnosis, and Treatment". Concise Review for Physicians. 83 (5): 574–579. doi:10.4065/83.5.574. PMID 18452690.
- ^ CDC (2019-01-15). "Prevention of Q fever | CDC". Centers for Disease Control and Prevention. Retrieved 2023-12-12.
- ^ a b c Ullah Q, Jamil T, Saqib M, Iqbal M, Neubauer H (2022-07-28). "Q Fever—A Neglected Zoonosis". Microorganisms. 10 (8): 1530. doi:10.3390/microorganisms10081530. ISSN 2076-2607. PMC 9416428. PMID 36013948.
- ^ Derrick EH (August 1937). "'Q' Fever a new fever entity: clinical features. diagnosis, and laboratory investigation". Medical Journal of Australia. 2 (8): 281–299. doi:10.5694/j.1326-5377.1937.tb43743.x.
- ^ McDade JE (1990). "Historical aspects of Q Fever". Q Fever: The Disease. Vol. I. CRC Press. p. 8. ISBN 978-0-8493-5984-2.
- ^ Burnet FM, Freeman M (1 July 1983). "Experimental studies on the virus of "Q" fever". Reviews of Infectious Diseases. 5 (4): 800–808. doi:10.1093/clinids/5.4.800. PMID 6194551.
- ^ "Public Health Weekly Reports for DECEMBER 30, 1938". Public Health Reports. 53 (52): 2259–2309. December 1938. doi:10.2307/4582746. JSTOR 4582746. PMC 2110862. PMID 19315693.
- ^ "Calling Dr. Kildare". Movie Mirrors Index. Archived from the original on 2012-02-04. Retrieved 30 April 2013.
- ^ Kalisch PA, Kalisch BJ (September 1985). "When Americans called for Dr. Kildare: images of physicians and nurses in the Dr. Kildare and Dr. Gillespie movies, 1937-1947" (PDF). Medical Heritage. 1 (5): 348–363. PMID 11616027. Archived (PDF) from the original on 2010-11-30.
- ^ Madariaga MG, Rezai K, Trenholme GM, Weinstein RA (November 2003). "Q fever: a biological weapon in your backyard". The Lancet. Infectious Diseases. 3 (11): 709–721. doi:10.1016/S1473-3099(03)00804-1. PMID 14592601.
- ^ "Deseret Test Center, Project SHAD, Shady Grove revised fact sheet".
- ^ Seshadri R, Paulsen IT, Eisen JA, Read TD, Nelson KE, Nelson WC, et al. (April 2003). "Complete genome sequence of the Q-fever pathogen Coxiella burnetii". Proceedings of the National Academy of Sciences of the United States of America. 100 (9): 5455–5460. Bibcode:2003PNAS..100.5455S. doi:10.1073/pnas.0931379100. PMC 154366. PMID 12704232.
- ^ Didkowska A, Klich D, Hapanowicz A, Orłowska B, Gałązka M, Rzewuska M, et al. (November 2021). "Pathogens with potential impact on reproduction in captive and free-ranging European bison (Bison bonasus) in Poland - a serological survey". BMC Veterinary Research. 17 (1): 345. doi:10.1186/s12917-021-03057-8. PMC 8567710. PMID 34736464.
- ^ Rijks JM, Roest HI, van Tulden PW, Kik MJ, IJzer J, Gröne A (December 2011). "Coxiella burnetii infection in roe deer during Q fever epidemic, the Netherlands". Emerging Infectious Diseases. 17 (12): 2369–2371. doi:10.3201/eid1712.110580. PMC 3311195. PMID 22172398.
- ^ Kirchgessner MS, Dubovi EJ, Whipps CM (November 2012). "Seroepidemiology of Coxiella burnetii in wild white-tailed deer (Odocoileus virginianus) in New York, United States". Vector Borne and Zoonotic Diseases. 12 (11): 942–947. doi:10.1089/vbz.2011.0952. PMID 22989183.
- ^ Cyr J, Turcotte MÈ, Desrosiers A, Bélanger D, Harel J, Tremblay D, et al. (February 2021). "Prevalence of Coxiella burnetii seropositivity and shedding in farm, pet and feral cats and associated risk factors in farm cats in Quebec, Canada". Epidemiology and Infection. 149: e57. doi:10.1017/s0950268821000364. PMC 8060820. PMID 33583452.
- ^ Conway R, Duncan C, Foster RA, Kersh GJ, Raverty S, Gelatt T, Frank C (April 2022). "Histologic lesions in placentas of northern fur seals (callorhinus ursinus) from a population with high placental prevalence of coxiella burnetii". Journal of Wildlife Diseases. 58 (2): 333–340. doi:10.7589/jwd-d-21-00037. PMC 11290099. PMID 35245373. S2CID 247236730.
- ^ Pascucci I, Di Domenico M, Dall'Acqua F, Sozio G, Cammà C (July 2015). "Detection of Lyme Disease and Q Fever Agents in Wild Rodents in Central Italy". Vector Borne and Zoonotic Diseases. 15 (7): 404–411. doi:10.1089/vbz.2015.1807. PMC 4507354. PMID 26134933.
- ^ Arricau-Bouvery N, Rodolakis A (May 2005). "Is Q Fever an emerging or re-emerging zoonosis?". Veterinary Research. 36 (3): 327–349. doi:10.1051/vetres:2005010. ISSN 0928-4249. PMID 15845229.
- ^ Plommet M, Capponi M, Gestin J, Renoux G, Marly J, Sahuc D, Petit A (1973). "FIÈVRE Q EXPÉRIMENTALE DES BOVINS". Annales de Recherches Vétérinaires (in French). 4 (2): 325–346. OCLC 862686843.
- ^ Arricau-Bouvery N, Rodolakis A (May 2005). "Is Q fever an emerging or re-emerging zoonosis?". Veterinary Research. 36 (3): 327–349. doi:10.1051/vetres:2005010. PMID 15845229.
- ^ De Biase D, Costagliola A, Del Piero F, Di Palo R, Coronati D, Galiero G, et al. (July 2018). "Coxiella burnetii in Infertile Dairy Cattle With Chronic Endometritis". Veterinary Pathology. 55 (4): 539–542. doi:10.1177/0300985818760376. PMID 29566608. S2CID 4268347.
- ^ Valla G. "Prevalenza di Coxiella burnetii nel latte di massa in allevamenti di bovine da latte italiani e possibile correlazione con problemi riproduttivi" (PDF).
- ^ Ordronneau S. Impact de la vaccination et de l'antibiothérapie sur l'incidence des troubles de la reproduction et sur la fertilité dans des troupeaux bovins laitiers infectés par Coxiella Burnetii. OCLC 836117348.
- ^ Guatteo R, Seegers H, Taurel AF, Joly A, Beaudeau F (April 2011). "Prevalence of Coxiella burnetii infection in domestic ruminants: a critical review". Veterinary Microbiology. 149 (1–2): 1–16. doi:10.1016/j.vetmic.2010.10.007. PMID 21115308.
- ^ Pexara A, Solomakos N, Govaris A (December 2018). "Q fever and seroprevalence of Coxiella burnetii in domestic ruminants". Veterinaria Italiana. 54 (4): 265–279. doi:10.12834/VetIt.1113.6046.3. PMID 30681125.
- ^ Pexara A, Solomakos N, Govaris A (2018-01-01). "Q fever and prevalence of Coxiella burnetii in milk". Trends in Food Science & Technology. 71: 65–72. doi:10.1016/j.tifs.2017.11.004. ISSN 0924-2244.
- ^ Dobos A, Gábor G, Wehmann E, Dénes B, Póth-Szebenyi B, Kovács ÁB, Gyuranecz M (September 2020). "Serological screening for Coxiella burnetii in the context of early pregnancy loss in dairy cows". Acta Veterinaria Hungarica. 68 (3): 305–309. doi:10.1556/004.2020.00035. PMID 33156002. S2CID 226269478.
- ^ Dobos A, Fodor I (October 2021). "Prevalence of Coxiella burnetii in bovine placentas in Hungary and Slovakia: Detection of a novel sequence type - Short communication". Acta Veterinaria Hungarica. 69 (4): 303–307. doi:10.1556/004.2021.00047. PMID 34735368. S2CID 243762186.
- ^ Obaidat MM, Kersh GJ (April 2017). "Prevalence and Risk Factors of Coxiella burnetii Antibodies in Bulk Milk from Cattle, Sheep, and Goats in Jordan". Journal of Food Protection. 80 (4): 561–566. doi:10.4315/0362-028X.JFP-16-377. PMC 6489127. PMID 28272921.
- ^ Espí A, Del Cerro A, Oleaga Á, Rodríguez-Pérez M, López CM, Hurtado A, et al. (May 2021). "One Health Approach: An Overview of Q Fever in Livestock, Wildlife and Humans in Asturias (Northwestern Spain)". Animals. 11 (5): 1395. doi:10.3390/ani11051395. PMC 8153578. PMID 34068431.
- ^ Agger JF, Paul S (July 2014). "Increasing prevalence of Coxiella burnetii seropositive Danish dairy cattle herds". Acta Veterinaria Scandinavica. 56 (1): 46. doi:10.1186/s13028-014-0046-2. PMC 4115160. PMID 25056416.
- ^ Guatteo R, Beaudeau F, Joly A, Seegers H (November 2007). "Coxiella burnetii shedding by dairy cows". Veterinary Research. 38 (6): 849–860. doi:10.1051/vetres:2007038. PMID 17903418.
- ^ Hawker JI, Ayres JG, Blair I, Evans MR, Smith DL, Smith EG, et al. (September 1998). "A large outbreak of Q fever in the West Midlands: windborne spread into a metropolitan area?". Communicable Disease and Public Health. 1 (3): 180–187. PMID 9782633.
- ^ Plummer PJ, McClure J, Menzies P, Morley PS, Van den Brom R, Van Metre DC (September 2018). "Management of Coxiella burnetii infection in livestock populations and the associated zoonotic risk: A consensus statement". Journal of Veterinary Internal Medicine. 32 (5): 1481–1494. doi:10.1111/jvim.15229. PMC 6189356. PMID 30084178.
- ^ "Coxevac | European Medicines Agency". 17 September 2018.
- ^ Roest HI, Tilburg JJ, van der Hoek W, Vellema P, van Zijderveld FG, Klaassen CH, Raoult D (January 2011). "The Q fever epidemic in The Netherlands: history, onset, response and reflection". Epidemiology and Infection. 139 (1): 1–12. doi:10.1017/S0950268810002268. PMID 20920383. S2CID 29026616.
