Leishmaniasis
| Leishmaniasis | |
|---|---|
| Other names | Leishmaniosis |
 | |
| Cutaneous leishmaniasis in the hand of a Central American adult | |
| Pronunciation |
|
| Specialty | Infectious disease |
| Symptoms | Skin ulcers, fever, low red blood cells, enlarged liver[2][3] |
| Causes | Leishmania parasites spread by sandflies[2] |
| Prevention | Bug nets, insecticide[2] |
| Frequency | 4–12 million[4][5] |
| Deaths | 24,200 (2015)[6] |
Leishmaniasis is a wide array of clinical manifestations caused by protozoal parasites of the Trypanosomatida genus Leishmania.[7] It is generally spread through the bite of phlebotomine sandflies, Phlebotomus and Lutzomyia, and occurs most frequently in the tropics and sub-tropics of Africa, Asia, the Americas, and southern Europe.[2][8] The disease can present in three main ways: cutaneous, mucocutaneous, or visceral.[2] The cutaneous form presents with skin ulcers, while the mucocutaneous form presents with ulcers of the skin, mouth, and nose. The visceral form starts with skin ulcers and later presents with fever, low red blood cell count, and enlarged spleen and liver.[2][3]
Infections in humans are caused by more than 20 species of Leishmania.[8][2] Risk factors include poverty, malnutrition, deforestation, and urbanization.[2] All three types can be diagnosed by seeing the parasites under microscopy.[2] Additionally, visceral disease can be diagnosed by blood tests.[3]
Leishmaniasis can be partly prevented by sleeping under nets treated with insecticide.[2] Other measures include spraying insecticides to kill sandflies and treating people with the disease early to prevent further spread.[2] The treatment needed is determined by where the disease is acquired, the species of Leishmania, and the type of infection.[2] Some possible medications used for visceral disease include liposomal amphotericin B,[9] a combination of pentavalent antimonials and paromomycin,[9] and miltefosine.[10] For cutaneous disease, paromomycin, fluconazole, or pentamidine may be effective.[11]
About 4 to 12 million people are currently infected[4][5] in some 98 countries.[3] About 2 million new cases[3] and between 20 and 50 thousand deaths occur each year.[2][12] About 200 million people in Asia, Africa, South and Central America, and southern Europe live in areas where the disease is common.[3][13] The World Health Organization has obtained discounts on some medications to treat the disease.[3] It is classified as a neglected tropical disease.[14] The disease may occur in a number of other animals, including dogs and rodents.[2]
Signs and symptoms
[edit]
The symptoms of leishmaniasis are skin sores which erupt weeks to months after the person is bitten by infected sand flies.
Leishmaniasis may be divided into the following types:[15]
- Cutaneous leishmaniasis is the most common form, which causes an open sore at each bite site, which heals in a few months to a year and half, leaving an unpleasant-looking scar.[2][3]
- Mucocutaneous leishmaniasis causes both skin and mucosal ulcers with damage primarily of the nose and mouth.[2][3]
- Visceral leishmaniasis or kala-azar ('black fever') is the most serious form, and is generally fatal if untreated.[2] Other consequences, which can occur a few months to years after infection, include fever, damage to the spleen and liver, and anemia.[2]
Leishmaniasis is considered one of the classic causes of a markedly enlarged (and therefore palpable) spleen; the organ, which is not normally felt during examination of the abdomen, may even become larger than the liver in severe cases.[citation needed]
Cause
[edit]
Leishmaniasis is transmitted by the bite of infected female phlebotomine sandflies[2] which can transmit the protozoa Leishmania.[2] The sandflies inject the infective stage, metacyclic promastigotes, during blood meals. Metacyclic promastigotes in the puncture wound are phagocytized by macrophages, and transform into amastigotes. Amastigotes multiply in infected cells and affect different tissues, depending in part on the host, and in part on which Leishmania species is involved. These differing tissue specificities cause the differing clinical manifestations of the various forms of leishmaniasis. Sandflies become infected during blood meals on infected hosts when they ingest macrophages infected with amastigotes. In the sandfly's midgut, the parasites differentiate into promastigotes, which multiply, differentiate into metacyclic promastigotes, and migrate to the proboscis.
The genomes of three Leishmania species (L. major, L. infantum, and L. braziliensis) have been sequenced, and this has provided much information about the biology of the parasite. For example, in Leishmania, protein-coding genes are understood to be organized as large polycistronic units in a head-to-head or tail-to-tail manner; RNA polymerase II transcribes long polycistronic messages in the absence of defined RNA pol II promoters, and Leishmania has unique features with respect to the regulation of gene expression in response to changes in the environment. The new knowledge from these studies may help identify new targets for urgently needed drugs and aid the development of vaccines.[16]
Vector
[edit]Although most of the literature mentions only one genus transmitting Leishmania to humans (Lutzomyia) in the New World, a 2003 study by Galati suggested a new classification for New World sand flies, elevating several subgenera to the genus level. Elsewhere in the world, the genus Phlebotomus is considered the vector of leishmaniasis.[16]
Possible non-human reservoirs
[edit]Some cases of infection of non-human animals of human-infecting species of Leishmania have been observed. In one study, L. major was identified in twelve out of ninety-one wild western lowland gorilla fecal samples[17] and in a study of fifty-two captive non-human primates under zoo captivity in a leishmaniasis endemic area, eight (all three chimpanzees, three golden lion tamarins, a tufted capuchin, and an Angolan talapoin), were found to be infected with L. infantum and capable of infecting Lutzomyia longipalpis sand flies, although "parasite loads in infected sand flies observed in this study were considered low".[18]
Organisms
[edit]Visceral disease is usually caused by Leishmania donovani, L. infantum, or L. chagasi,[3] but occasionally these species may cause other forms of disease.[3] The cutaneous form of the disease is caused by more than 15 species of Leishmania.[3]
Risk factors
[edit]Risk factors include malnutrition, deforestation, lack of sanitation, suppressed immune system and urbanization.[2]
Diagnosis
[edit]
Leishmaniasis is diagnosed in the hematology laboratory by direct visualization of the amastigotes (Leishman–Donovan bodies). Buffy-coat preparations of peripheral blood or aspirates from marrow, spleen, lymph nodes, or skin lesions should be spread on a slide to make a thin smear and stained with Leishman stain or Giemsa stain (pH 7.2) for 20 minutes. Amastigotes are seen within blood and spleen monocytes or, less commonly, in circulating neutrophils and in aspirated tissue macrophages. They are small, round bodies 2–4 μm in diameter with indistinct cytoplasm, a nucleus, and a small, rod-shaped kinetoplast. Occasionally, amastigotes may be seen lying free between cells.[19] However, the retrieval of tissue samples is often painful for the patient and identification of the infected cells can be difficult. So, other indirect immunological methods of diagnosis are developed, including enzyme-linked immunosorbent assay, antigen-coated dipsticks, and direct agglutination test. Although these tests are readily available, they are not the standard diagnostic tests due to their insufficient sensitivity and specificity[citation needed].
Several different polymerase chain reaction (PCR) tests are available for the detection of Leishmania DNA.[3] With this assay, a specific and sensitive diagnostic procedure is finally possible. The most sensitive PCR tests use minicircle kinetoplast DNA found in the parasite. Kinetoplast DNA contains sequences for mitochondrial proteins in its maxicircles(~25–50 per parasite), and guide RNA in its minicircles(~10'000 per parasite) of the kinetoplast. With this specific method, one can still detect Leishmania even with a very low parasite load. When needing to diagnose a specific species of Leishmania, as opposed to only detection, other PCR methods have been superior.[20]
Most forms of the disease are transmitted only from nonhuman animals, but some can be spread between humans. Infections in humans are caused by about 21 of 30 species that infect mammals;[21] the different species look the same, but they can be differentiated by isoenzyme analysis, DNA sequence analysis, or monoclonal antibodies.
Prevention
[edit]- Using insect repellent to exposed skin and under the ends of sleeves and pant legs. Follow the instructions on the label of the repellent. The most effective repellents generally are those that contain the chemical DEET (N,N-diethylmetatoluamide)[22]
- Leishmaniasis can be partly prevented by using nets treated with insecticide or insect repellent while sleeping.[2] To provide good protection against sandflies, fine mesh sizes of 0.6 mm or less are required, but a mosquito net with 1.2mm mesh will provide a limited reduction in the number of sandfly bites.[23] Finer mesh sizes have the downside of higher cost and reduced air circulation which can cause overheating. Many Phlebotomine sandfly attacks occur at sunset rather than at night, so it may also be useful to put nets over doors and windows or to use insect repellents.[22]
- Use of insecticide-impregnated dog collars and treatment or culling of infected dogs.[citation needed]
- Spraying houses and animal shelters with insecticides.[23]
Treatment
[edit]
The treatment is determined by where the disease is acquired, the species of Leishmania, and the type of infection.[2] For visceral leishmaniasis in India, South America, and the Mediterranean, liposomal amphotericin B is the recommended treatment and is often used as a single dose.[3][9] Rates of cure with a single dose of amphotericin have been reported as 95%.[3] In India, almost all infections are resistant to pentavalent antimonials.[3] In Africa, a combination of pentavalent antimonials and paromomycin is recommended.[9] These, however, can have significant side effects.[3] Miltefosine, an oral medication, is effective against both visceral and cutaneous leishmaniasis.[10] Side effects are generally mild, though it can cause birth defects if taken within three months of getting pregnant.[3][10] It does not appear to work for L. major or L. braziliensis.[11] Trifluralin, a herbicide, is shown to be effective treatment as ointment, without hemolytic or cell-toxic side-effects.[24]
The evidence around the treatment of cutaneous leishmaniasis is poor.[3] A number of topical treatments may be used for cutaneous leishmaniasis. Which treatments are effective depends on the strain, with topical paromomycin effective for L. major, L. tropica, L. mexicana, L. panamensis, and L. braziliensis.[11] Pentamidine is effective for L. guyanensis.[11] Oral fluconazole or itraconazole appears effective in L. major and L. tropica.[3][11] There is limited evidence to support the use of heat therapy in cutaneous leishmaniasis as of 2015.[25]
There are no studies determining the effect of oral nutritional supplements on visceral leishmaniasis being treated with anti-leishmanial drug therapy.[26]
Epidemiology
[edit]

Out of 200 countries and territories reporting to WHO, 97 countries and territories are endemic for leishmaniasis.[28] The settings in which leishmaniasis is found range from rainforests in Central and South America to deserts in western Asia and the Middle East. It affects as many as 12 million people worldwide, with 1.5–2.0 million new cases each year.[29] The visceral form of leishmaniasis has an estimated incidence of 500,000 new cases.[30] In 2014, more than 90% of new cases reported to WHO occurred in six countries: Brazil, Ethiopia, India, Somalia, South Sudan and Sudan.[31] As of 2010,[update] it caused about 52,000 deaths, down from 87,000 in 1990.[12] Different types of the disease occur in different regions of the world.[2] Cutaneous disease is most common in Afghanistan, Algeria, Brazil, Colombia, and Iran, while mucocutaneous disease is most common in Bolivia, Brazil, and Peru, and visceral disease is most common in Bangladesh, Brazil, Ethiopia, India, and Sudan.[2]
Leishmaniasis is found through much of the Americas from northern Argentina to South Texas, though not in Uruguay or Chile, and has recently been shown to be spreading to North Texas and Oklahoma,[32][33] and further expansion to the north may be facilitated by climate change as more habitat becomes suitable for vector and reservoir species for leishmaniasis.[34] Leishmaniasis is also known as papalomoyo, papa lo moyo, úlcera de los chicleros, and chiclera in Latin America.[35] During 2004, an estimated 3,400 troops from the Colombian army, operating in the jungles near the south of the country (in particular around the Meta and Guaviare departments), were infected with leishmaniasis. Allegedly, a contributing factor was that many of the affected soldiers did not use the officially provided insect repellent because of its disturbing odor. Nearly 13,000 cases of the disease were recorded in all of Colombia throughout 2004, and about 360 new instances of the disease among soldiers had been reported in February 2005.[36]
The disease is found across much of Asia, and in the Middle East. Within Afghanistan, leishmaniasis occurs commonly in Kabul, partly due to bad sanitation and waste left uncollected in streets, allowing parasite-spreading sand flies an environment they find favorable.[37][38] In Kabul, the number of people infected was estimated to be at least 200,000, and in three other towns (Herat, Kandahar, and Mazar-i-Sharif) about 70,000 more occurred, according to WHO figures from 2002.[39][40] Kabul is estimated as the largest center of cutaneous leishmaniasis in the world, with around 67,500 cases as of 2004.[41] Africa, in particular the East and North,[27] is also home to cases of leishmaniasis. Leishmaniasis is considered endemic also in some parts of southern parts of western Europe and spreading towards north in recent years.[42] For example, an outbreak of cutaneous and visceral leishmaniasis was reported from Madrid, Spain, between 2010 and 2012.[43]
Leishmaniasis is mostly a disease of the developing world, and is rarely known in the developed world outside a small number of cases, mostly in instances where troops are stationed away from their home countries. Leishmaniasis has been reported by U.S. troops stationed in Saudi Arabia and Iraq since the Gulf War of 1990, including visceral leishmaniasis.[44][45][46] In September 2005, the disease was contracted by at least four Dutch marines who were stationed in Mazar-i-Sharif, Afghanistan, and subsequently repatriated for treatment.[47][48]
History
[edit]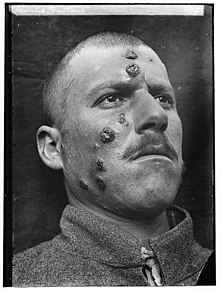
Descriptions of conspicuous lesions similar to cutaneous leishmaniasis appear on tablets from King Ashurbanipal from the seventh century BCE, some of which may have derived from even earlier texts from 1500 to 2500 BCE. Persian physicians, including Avicenna in the 10th century CE, gave detailed descriptions of what was called balkh sore.[49] In 1756, Alexander Russell, after examining a Turkish patient, gave one of the most detailed clinical descriptions of the disease. Physicians in the Indian subcontinent would describe it as kala-azar (pronounced kālā āzār, the Urdu, Hindi, and Hindustani phrase for "black fever", kālā meaning black and āzār meaning fever or disease). In the Americas, evidence of the cutaneous form of the disease in Ecuador and Peru appears in pre-Inca pottery depicting skin lesions and deformed faces dating back to the first century CE. Some 15th- and 16th-century texts from the Inca period and from Spanish colonials mention "valley sickness", "Andean sickness", or "white leprosy", which are likely to be the cutaneous form.[50]
It remains unclear who first discovered the organism. David Douglas Cunningham, Surgeon Major of the British Indian army, may have seen it in 1885 without being able to relate it to the disease.[51][52] Peter Borovsky, a Russian military surgeon working in Tashkent, conducted research into the etiology of "oriental sore", locally known as sart sore, and in 1898 published the first accurate description of the causative agent, correctly described the parasite's relation to host tissues and correctly referred it to the protozoa. However, because his results were published in Russian in a journal with low circulation, his results were not internationally acknowledged during his lifetime.[53] In 1901, William Boog Leishman identified certain organisms in smears taken from the spleen of a patient who had died from "dum-dum fever" (Dum Dum is an area close to Calcutta) and proposed them to be trypanosomes, found for the first time in India.[54] A few months later, Captain Charles Donovan (1863–1951) confirmed the finding of what became known as Leishman-Donovan bodies in smears taken from people in Madras in southern India.[55] But it was Ronald Ross who proposed that Leishman-Donovan bodies were the intracellular stages of a new parasite, which he named Leishmania donovani.[56] The link with the disease kala-azar was first suggested by Charles Donovan, and was conclusively demonstrated by Charles Bentley's discovery of L. donovani in patients with kala-azar.[57] Transmission by the sandfly was hypothesized by Lionel Napier and Ernest Struthers at the School of Tropical Medicine at Calcutta and later proven by his colleagues.[58][59] The disease became a major problem for Allied troops fighting in Sicily during the Second World War; research by Leonard Goodwin then showed pentostam was an effective treatment.[60]
Society and culture
[edit]The Institute for OneWorld Health has reintroduced the drug paromomycin for treatment of leishmaniasis, results with which led to its approval as an orphan drug. The Drugs for Neglected Diseases Initiative is also actively facilitating the search for novel therapeutics. A treatment with paromomycin will cost about US$10. The drug had originally been identified in the 1950s, but had been abandoned because it would not be profitable, as the disease mostly affects poor people.[61] The Indian government approved paromomycin for sale in August 2006.[62]
By 2012 the World Health Organization had successfully negotiated with the manufacturers to achieve a reduced cost for liposomal amphotericin B, to US$18 a vial, but a number of vials are needed for treatment and it must be kept at a stable, cool temperature.[3]
Research
[edit]
As of 2017, no leishmaniasis vaccine for humans was available.[63][64] Research to produce a human vaccine is ongoing.[64]
Currently some effective leishmaniasis vaccines for dogs exist.[65] There is also consideration that public health practices can control or eliminate leishmaniasis without a vaccine.[64] Pyrimidine–based drugs are being explored as anti-leishmanial compounds.[66]
See also
[edit]References
[edit]- ^ "Leishmaniasis definition and meaning | Collins English Dictionary". Archived from the original on 24 December 2013. Retrieved 23 December 2013.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y "Leishmaniasis Fact sheet N°375". World Health Organization. January 2014. Archived from the original on 21 February 2014. Retrieved 17 February 2014.
- ^ a b c d e f g h i j k l m n o p q r s t u v Barrett MP, Croft SL (2012). "Management of trypanosomiasis and leishmaniasis". British Medical Bulletin. 104 (1): 175–96. doi:10.1093/bmb/lds031. PMC 3530408. PMID 23137768.
- ^ a b "Leishmaniasis Magnitude of the problem". World Health Organization. Archived from the original on 26 October 2013. Retrieved 17 February 2014.
- ^ a b Vos T, Allen C, Arora M, Barber RM, Bhutta ZA, Brown A, et al. (GBD 2015 Disease Injury Incidence Prevalence Collaborators) (October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
- ^ Wang H, Naghavi M, Allen C, Barber RM, Bhutta ZA, Carter A, et al. (GBD 2015 Mortality Causes of Death Collaborators) (October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- ^ Roy M, Rawat A, Kaushik S, Jyoti A, Srivastava VK (1 August 2022). "Endogenous cysteine protease inhibitors in upmost pathogenic parasitic protozoa". Microbiological Research. 261: 127061. doi:10.1016/j.micres.2022.127061. ISSN 0944-5013. PMID 35605309. S2CID 248741177.
- ^ a b Rawat A, Roy M, Jyoti A, Kaushik S, Verma K, Srivastava VK (August 2021). "Cysteine proteases: Battling pathogenic parasitic protozoans with omnipresent enzymes". Microbiological Research. 249: 126784. doi:10.1016/j.micres.2021.126784. PMID 33989978. S2CID 234597200.
- ^ a b c d Sundar S, Chakravarty J (January 2013). "Leishmaniasis: an update of current pharmacotherapy". Expert Opinion on Pharmacotherapy. 14 (1): 53–63. doi:10.1517/14656566.2013.755515. PMID 23256501. S2CID 207479873.
- ^ a b c Dorlo TP, Balasegaram M, Beijnen JH, de Vries PJ (November 2012). "Miltefosine: a review of its pharmacology and therapeutic efficacy in the treatment of leishmaniasis". The Journal of Antimicrobial Chemotherapy. 67 (11): 2576–97. doi:10.1093/jac/dks275. PMID 22833634.
- ^ a b c d e Minodier P, Parola P (May 2007). "Cutaneous leishmaniasis treatment". Travel Medicine and Infectious Disease. 5 (3): 150–8. doi:10.1016/j.tmaid.2006.09.004. PMID 17448941.
- ^ a b Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. (December 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2095–128. doi:10.1016/S0140-6736(12)61728-0. hdl:10536/DRO/DU:30050819. PMC 10790329. PMID 23245604. S2CID 1541253.
- ^ Ejazi SA, Ali N (January 2013). "Developments in diagnosis and treatment of visceral leishmaniasis during the last decade and future prospects". Expert Review of Anti-Infective Therapy. 11 (1): 79–98. doi:10.1586/eri.12.148. PMID 23428104. S2CID 20508342.
- ^ "Neglected Tropical Diseases". cdc.gov. 6 June 2011. Archived from the original on 4 December 2014. Retrieved 28 November 2014.
- ^ James WD, Berger TG, Elston DM (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. pp. 422–428. ISBN 978-0-7216-2921-6.
- ^ a b Myler PJ, Fasel N (2008). Leishmania: After The Genome. Caister Academic Press. ISBN 978-1-904455-28-8. Archived from the original on 23 April 2008.[page needed]
- ^ Hamad I, Forestier CL, Peeters M, Delaporte E, Raoult D, Bittar F (15 January 2015). "Wild Gorillas as a Potential Reservoir of Leishmania major". J. Infect. Dis. 211 (2): 267–273. doi:10.1093/infdis/jiu380. PMC 4342692. PMID 25001460.
- ^ Ayisa Rodrigues de Oliveira, Guilherme Rafael Gomide Pinheiro, Herlandes P. Tinoco, Maria Elvira Loyola, Carlyle Mendes Coelho, Edelberto Santos Dias, Érika Michalsky Monteiro, Fabiana de Oliveira Lara e Silva, Angela Tinoco Pessanha, Andreza Geisiane Maia Souza, Nathália Cristina Lima Pereira, Nelder F. Gontijo, Ricardo T. Fujiwara, Tatiane Alves da Paixão, Renato Lima Santos (17 April 2019). "Competence of non-human primates to transmit Leishmania infantum to the invertebrate vector Lutzomyia longipalpis". PLOS Neglected Tropical Diseases. 13 (4): e0007313. doi:10.1371/journal.pntd.0007313. PMC 6488095. PMID 30995227.
- ^ Dacie JV, Bain BJ, Bates I (2006). Dacie and Lewis practical hematology. Philadelphia: Churchill Livingstone/Elsevier. ISBN 978-0-443-06660-3.[page needed]
- ^ Bensoussan E, Nasereddin A, Jonas F, Schnur LF, Jaffe CL (April 2006). "Comparison of PCR assays for diagnosis of cutaneous leishmaniasis". Journal of Clinical Microbiology. 44 (4): 1435–9. doi:10.1128/JCM.44.4.1435-1439.2006. PMC 1448629. PMID 16597873.
- ^ "Parasites – Leishmaniasis". Centers for Disease Control and Prevention. January 2013.
- ^ a b Prevention CC (19 February 2020). "CDC – Leishmaniasis – Prevention & Control". cdc.gov. Retrieved 26 June 2021.
- ^ a b * Alexander B, Maroli M (March 2003). "Control of phlebotomine sandflies". Medical and Veterinary Entomology. 17 (1): 1–18. doi:10.1046/j.1365-2915.2003.00420.x. PMID 12680919. S2CID 31387956.
- ^ Esteves MA, Fragiadaki I, Lopes R, Scoulica E, Cruz ME (1 January 2010). "Synthesis and biological evaluation of trifluralin analogues as antileishmanial agents". Bioorganic & Medicinal Chemistry. 18 (1): 274–281. doi:10.1016/j.bmc.2009.10.059.
- ^ Von Stebut E (March 2015). "Leishmaniasis". Journal of the German Society of Dermatology. 13 (3): 191–200, quiz 201. doi:10.1111/ddg.12595. PMID 25721626. S2CID 221649492.
- ^ Custodio E, López-Alcalde J, Herrero M, Bouza C, Jimenez C, Storcksdieck Genannt Bonsmann S, Mouratidou T, López-Cuadrado T, Benito A, Alvar J, et al. (Cochrane Infectious Diseases Group) (March 2018). "Nutritional supplements for patients being treated for active visceral leishmaniasis". The Cochrane Database of Systematic Reviews. 2018 (3): CD012261. doi:10.1002/14651858.CD012261.pub2. PMC 6494195. PMID 29578237.
- ^ a b Aoun K, Bouratbine A (2014). "Cutaneous leishmaniasis in North Africa: a review". Parasite. 21: 14. doi:10.1051/parasite/2014014. PMC 3952656. PMID 24626301.

- ^ "Leishmaniasis: Situation and trends". WHO Global Health Observatory. Retrieved 30 May 2018.
- ^ "Leishmaniasis: Magnitude of the problem". World Health Organization. Archived from the original on 26 October 2013.
- ^ "Hope for tropical disease vaccine". BBC News. 23 April 2006. Archived from the original on 27 April 2006.
- ^ "Epidemiological situation: Epidemiology". World Health Organization. Archived from the original on 30 June 2004. Retrieved 30 May 2018.
- ^ "Dallas News: Rare, non-fatal skin disease found in N. Texans". Archived from the original on 27 December 2009. Retrieved 2 June 2015.
- ^ Clarke CF, Bradley KK, Wright JH, Glowicz J (January 2013). "Case report: Emergence of autochthonous cutaneous leishmaniasis in northeastern Texas and southeastern Oklahoma". The American Journal of Tropical Medicine and Hygiene. 88 (1): 157–61. doi:10.4269/ajtmh.2012.11-0717. PMC 3541728. PMID 23185078.
- ^ González C, Wang O, Strutz SE, González-Salazar C, Sánchez-Cordero V, Sarkar S (January 2010). Galvani AP (ed.). "Climate change and risk of leishmaniasis in north america: predictions from ecological niche models of vector and reservoir species". PLOS Neglected Tropical Diseases. 4 (1): e585. doi:10.1371/journal.pntd.0000585. PMC 2799657. PMID 20098495.
- ^ "Papalomoyo" (PDF). Archived from the original (PDF) on 23 July 2011. Retrieved 16 August 2010.
- ^ "Informes – Informe de Fronteras Febrero 2005". Servicio Jesuita a Refugiados. Archived from the original on 10 November 2005.
- ^ "CENTRAL/S. ASIA – Kabul: A city in intensive care". Al Jazeera English. Archived from the original on 18 June 2007.
- ^ Birsel R (7 May 2007). "Disfiguring skin disease plagues Afghanistan". e-Ariana. Reuters. Archived from the original on 10 December 2015. Retrieved 8 December 2015.
- ^ Birsel R (28 June 2002). "Disfiguring epidemic hits 270,000 Afghans". e-Ariana. Reuters. Archived from the original on 10 December 2015. Retrieved 8 December 2015.
- ^ "WHO Seeking Funds to Prevent Leishmaniasis Outbreak in Afghanistan". voanews. October 2009.
- ^ "World Health Organization action in Afghanistan aims to control debilitating leishmaniasis". Archived from the original on 26 October 2010.
- ^ Medlock JM, Hansford KM, Van Bortel W, Zeller H, Alten B (June 2014). "A summary of the evidence for the change in European distribution of phlebotomine sand flies (Diptera: Psychodidae) of public health importance". Journal of Vector Ecology. 39 (1): 72–7. doi:10.1111/j.1948-7134.2014.12072.x. PMID 24820558. S2CID 20645170.
- ^ Aguado M, Espinosa P, Romero-Maté A, Tardío JC, Córdoba S, Borbujo J (May 2013). "Outbreak of cutaneous leishmaniasis in Fuenlabrada, Madrid". Actas Dermo-Sifiliograficas. 104 (4): 334–42. doi:10.1016/j.adengl.2013.03.005. PMID 23567452.
- ^ Kennedy K (30 March 2010). "VCS Advocacy in the News: VA May Designate 9 Infectious Diseases as Related to Gulf War". Veterans for Common Sense. Archived from the original on 13 February 2011. Retrieved 10 February 2011.
- ^ "Business: Company's mesh will help troops beat 'Baghdad boils'". Archived from the original on 16 March 2005.
- ^ "Archived copy" (PDF). Archived from the original (PDF) on 12 October 2007. Retrieved 17 September 2007.
{{cite web}}: CS1 maint: archived copy as title (link) - ^ Bhatia S, Goli D (2016). Leishmaniasis: Biology, Control and New Approaches for Its Treatment. CRC Press. ISBN 9781315341897.
- ^ van Thiel PP, Leenstra T, de Vries HJ, van der Sluis A, van Gool T, Krull AC, van Vugt M, de Vries PJ, Zeegelaar JE, Bart A, van der Meide WF, Schallig HD, Faber WR, Kager PA (December 2010). "Cutaneous leishmaniasis (Leishmania major infection) in Dutch troops deployed in northern Afghanistan: epidemiology, clinical aspects, and treatment". The American Journal of Tropical Medicine and Hygiene. 83 (6): 1295–300. doi:10.4269/ajtmh.2010.10-0143. PMC 2990047. PMID 21118937.
- ^ Cox FE (October 2002). "History of human parasitology". Clinical Microbiology Reviews. 15 (4). The Wellcome Trust: 595–612. doi:10.1128/CMR.15.4.595-612.2002. ISBN 978-1-869835-86-6. OCLC 35161690. PMC 126866. PMID 12364371.
- ^ "WHO: Leishmaniasis background information – a brief history of the disease". Archived from the original on 15 March 2014.
- ^ Cunningham DD (1885). On the presence of peculiar parasitic organisms in the tissue of a specimen of Delhi boil. Scientific memoirs officers Medical Sanitary Departments Government India. Calcutta: Printed by the superintendent of government printing, India. pp. 21–31. OCLC 11826455.
- ^ Cox FE (October 2002). "History of human parasitology". Clinical Microbiology Reviews. 15 (4): 595–612. doi:10.1128/CMR.15.4.595-612.2002. PMC 126866. PMID 12364371.
- ^ Hoare CA (1938). "Early discoveries regarding the parasite of oriental sore". Transactions of the Royal Society of Tropical Medicine and Hygiene. 32 (1): 67–92. doi:10.1016/S0035-9203(38)90097-5.
- ^ Leishman WB (1903). "On the possibility of the occurrence of trypanomiasis in India". The British Medical Journal. 1 (2213): 1252–1254. doi:10.1136/bmj.1.2213.1252. PMC 2514706.
- ^ Donovan C (1903). "Memoranda: On the possibility of the occurrence of trypanomiasis in India". The British Medical Journal.
- ^ Ross R (November 1903). "Further Notes on Leishman's Bodies". British Medical Journal. 2 (2239): 1401. doi:10.1136/bmj.2.2239.1401. PMC 2514909. PMID 20761210.
- ^ Bentley CA (24 December 1903). "Telegram to R. Ross". Ross Archives: 47/157.
- ^ "Dr. L. Everard Napier". The Indian Medical Gazette. 78 (5): 252. May 1943. PMC 5158438. PMID 29012190.
- ^ Gewurtz MS (1 January 2017). "Transnationalism in Missionary Medicine: The Case of Kala-azar in China and India, 1909–1946". Social Sciences and Missions. 30 (1–2): 30–43. doi:10.1163/18748945-03001001. ISSN 1874-8945.
- ^ "Leonard Goodwin – Telegraph". The Daily Telegraph. 14 January 2009. Archived from the original on 20 April 2009. Retrieved 18 January 2009.
- ^ "A Small Charity Takes the Reins in Fighting a Neglected Disease". New York Times. 31 July 2006. Archived from the original on 20 December 2016.
- ^ "Drug Program – Clinical Trial of Paromomycin". Institute for OneWorld Health. Archived from the original on 6 June 2010. Retrieved 10 February 2011.
- ^ Srivastava S, Shankar P, Mishra J, Singh S (May 2016). "Possibilities and challenges for developing a successful vaccine for leishmaniasis". Parasites & Vectors. 9 (1): 277. doi:10.1186/s13071-016-1553-y. PMC 4866332. PMID 27175732.
- ^ a b c Ghorbani M, Farhoudi R (2018). "Leishmaniasis in humans: drug or vaccine therapy?". Drug Design, Development and Therapy. 12: 25–40. doi:10.2147/DDDT.S146521. PMC 5743117. PMID 29317800.
- ^ Moafi M, Rezvan H, Sherkat R, Taleban R (2019). "Leishmania Vaccines Entered in Clinical Trials: A Review of Literature". International Journal of Preventive Medicine. 10: 95. doi:10.4103/ijpvm.IJPVM_116_18. PMC 6592111. PMID 31360342.
- ^ Ramesh D, Sarkar D, Joji A, Singh M, Mohanty AK, G Vijayakumar B, Chatterjee M, Sriram D, Muthuvel SK, Kannan T (April 2022). "First-in-class pyrido[2,3- d ]pyrimidine-2,4(1 H ,3 H )-diones against leishmaniasis and tuberculosis: Rationale, in vitro, ex vivo studies and mechanistic insights". Archiv der Pharmazie. 355 (4): 2100440. doi:10.1002/ardp.202100440. ISSN 0365-6233. PMID 35106845. S2CID 246474821.
