Epidermolysis bullosa
Parts of this article (those related to treatment with genetically modified skin grafts) need to be updated. (November 2020) |
| Epidermolysis bullosa | |
|---|---|
| Other names | Butterfly children[1] |
 | |
| A five-year-old boy displaying characteristic blisters of epidermolysis bullosa | |
| Specialty | Dermatology |
| Symptoms | Painful skin blisters[2][3] |
| Complications | Esophageal narrowing, squamous cell skin cancer, amputations[4][5] |
| Usual onset | At birth[5] |
| Duration | Often lifelong[5] |
| Types | Epidermolysis bullosa simplex, dystrophic epidermolysis bullosa, junctional epidermolysis bullosa, Kindler syndrome[2] |
| Causes | Genetic[2] |
| Diagnostic method | Skin biopsy, genetic testing[6] |
| Differential diagnosis | Bullous pemphigoid, pemphigus vulgaris, friction blisters, insect bites[5] |
| Treatment | Wound care, pain control, controlling infections, nutritional support[2] |
| Prognosis | Death usually occurs during early adulthood |
| Frequency | around 1 in 500,000[5] |
Epidermolysis bullosa (EB) is a group of rare medical conditions that result in easy blistering of the skin and mucous membranes. Blisters occur with minor trauma or friction and are painful. Its severity can range from mild to fatal.[7] Inherited EB is a rare disease with a prevalence in the United States of 8.2 per million live births.[8] Those with mild cases may not develop symptoms until they start to crawl or walk. Complications may include esophageal narrowing, squamous cell skin cancer, and the need for amputations.[medical citation needed]
EB is due to a mutation in at least one of 16 different genes. Some types are autosomal dominant while others are autosomal recessive.[2] The underlying mechanism is a defect in attachment between or within the layers of the skin. Loss or diminished function of type VII collagen leads to weakness in the structural architecture of the dermal–epidermal junction (DEJ) and mucosal membranes.[9] There are four main types: epidermolysis bullosa simplex (EBS), dystrophic epidermolysis bullosa (DEB), junctional epidermolysis bullosa (JEB), and Kindler syndrome. The diagnosis is suspected based on symptoms and confirmed by skin biopsy or genetic testing.
There is no cure for the condition. Management involves wound care, pain control, controlling infections, nutritional support, and prevention and treatment of complications.[7] About half a million people are affected globally.[5] It occurs equally commonly in males and females.[10]
Classification
[edit]Epidermolysis bullosa refers to a group of disorders that involve the formation of blisters following trivial trauma. Over 300 mutations have been identified in this condition.[11] They have been classified into the following types:[12][13]: 596
Epidermolysis bullosa simplex
[edit]Epidermolysis bullosa simplex (EBS) is a form of EB that causes blisters at the site of rubbing. It typically affects the hands and feet, and is typically inherited in an autosomal dominant manner, affecting the keratin genes KRT5 and KRT14. Therefore, there is a failure in keratinization, which affects the integrity and the ability of the skin to resist mechanical stresses.[citation needed]
Junctional epidermolysis bullosa
[edit]Junctional epidermolysis bullosa (JEB) is an inherited disease affecting laminin and collagen. This disease is characterized by blister formation within the lamina lucida of the basement membrane zone[13]: 599 and is inherited in an autosomal recessive manner. It also presents with blisters at the site of friction, especially on the hands and feet, and has variants that can occur in children and adults. Less than one person per million people is estimated to have this form of EB.[14]
Dystrophic epidermolysis bullosa
[edit]Dystrophic epidermolysis bullosa (DEB) is an inherited variant affecting the skin and other organs. DEB is caused by genetic defects (or mutations) within the human COL7A1 gene encoding the protein type VII collagen (collagen VII).[15] DEB-causing mutations can be either autosomal dominant or autosomal recessive. Epidermolysis bullosa pruriginosa and albopapuloid epidermolysis bullosa (Pasini disease) are rare subtypes of this disease.[16]
Other genetic variants
[edit]| OMIM | Name | Locus | Gene |
|---|---|---|---|
| 609638 | epidermolysis bullosa, lethal acantholytic | 6p24 | DSP |
Epidermolysis bullosa acquisita
[edit]Acral peeling
[edit]Pathophysiology
[edit]The human skin consists of two layers: an outermost layer called the epidermis and a layer underneath called the dermis. In individuals with healthy skin, there are protein anchors between these two layers (Dermo epidermal junction) that prevent them from moving independently from one another (shearing). In people born with EB, the two skin layers lack the protein anchors that hold them together, resulting in extremely fragile skin—even minor mechanical friction (like rubbing or pressure) or trauma will separate the layers of the skin and form blisters and painful sores.[17] EB individuals manifest unremitting skin blistering that evolves into chronic wounds, inflammation, and fibrosis.[18] People with EB have compared the sores with third-degree burns. Furthermore, as a complication of the chronic skin damage, people with EB have an increased risk of malignancies (cancers) of the skin.[19] Virtually any organ lined or covered by epithelium may be injured in inherited EB. External eye, esophagus, upper airway, and genitourinary tract are the epithelial surfaced tissues that are at particular risk.[20]
Diagnosis
[edit]EB can be diagnosed either by a skin (punch) biopsy at the edge of a wound with immunofluorescent mapping, or via blood sample and genetic testing.[citation needed]
Treatment
[edit]
Research has focused on changing the mixture of keratins produced in the skin. There are 54 known keratin genes—of which 28 belong to the type I intermediate filament genes and 26 to type II—which work as heterodimers. Many of these genes share substantial structural and functional similarity, but they are specialized to cell type and/or conditions under which they are normally produced. If the balance of production could be shifted away from the mutated, dysfunctional keratin gene toward an intact keratin gene, symptoms could be reduced. For example, sulforaphane, a compound found in broccoli, was found to reduce blistering in a mouse model to the point where affected pups could not be identified visually, when injected into pregnant mice (5 μmol/day = 0.9 mg) and applied topically to newborns (1 μmol/day = 0.2 mg in jojoba oil).[21]
As of 2008, clinical research at the University of Minnesota has explored allogeneic bone marrow transplantation for RD and junctional EB, treating a two-year-old child who is one of two brothers with EB. A second transplant has also been performed on the child's older brother. A Missouri boy has also successfully undergone the transplant, as well as a 5 year old boy from Alabama. So far there have been 12 successful transplants.[22] Another transplant is scheduled for a California baby. A clinical trial is planned for 30 subjects.[23] However, the immune suppression that bone marrow transplantation requires causes a risk of serious infections with large scale blisters and skin erosion.[24] Indeed, at least four people have died in the course of either preparation for or institution of bone marrow transplantation for EB, out of only a small group of patients treated so far.[24] The mechanism of action of this therapy is unclear as hematopoietic stem cells are not thought to contribute to epithelial lineages. Rather, it is speculated that cross-correction from tissue-resident graft-derived immune cells contributes to the observed clinical benefit.[25]
A pilot study performed in 2015 suggests that systemic granulocyte-colony stimulating factor (G-CSF) may promote increased wound healing in people with dystrophic EB.[26] Transplanting skin derived from genetically modified stem cells onto the wound surfaces has been studied with a report of improvements in one person.[27]
A 2017 clinical trial with male RDEB (recessive dystrophic EB) patients conducted successful grafting of type VII gene corrected keratinocytes (COL7A1 gene correction using retrovirus transduction), without any serious adverse effects. Type VII collage formation was observed at the dermis-epidermis junction in significant amounts.[28]
A 2020 study demonstrated the safe allogenic grafting of acellular dermal matrix/scaffolds in EB patients without any observed infection or necrosis and instead noted fewer required dressing changes, promoted wound healing, pain reduction, and an overall improvement in the quality of life of the patients.[29]
In 2022, a pharmaceutical gel made out of birch bark extract from Betula pendula and Betula pubescens was approved by the European Union as a treatment for epidermolysis bullosa.[30][31]
Birch triterpenes
[edit]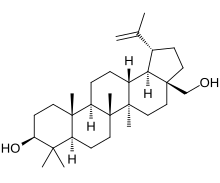
Birch triterpenes, sold under the brand name Filsuvez, is an extract of birch bark used as a topical medication for the treatment of epidermolysis bullosa.[32][33] The active ingredients are triterpenes extracted from the outer bark of silver birch (Betula pendula) and downy birch (Betula pubescens).[34]
The most common side effects include wound complications such as skin reactions at the application site, infections, pruritus (itching), and hypersensitivity.[33]
Birch triterpenes was approved for medical use in the European Union in June 2022,[33] and in the United States in December 2023.[35][36]Monitoring
[edit]The Epidermolysis Bullosa Disease Activity and Scarring index (EBDASI) is a scoring system that objectively quantifies the severity of EB. The EBDASI is a tool for clinicians and patients to monitor the severity of the disease. It has also been designed to evaluate the response to new therapies for the treatment of EB. The EBDASI was developed and validated by Professor Dedee Murrell and her team of students and fellows at the St George Hospital, University of New South Wales, in Sydney, Australia. It was presented at the International Investigative Dermatology congress in Edinburgh in 2013 and a paper-based version was published in the Journal of the American Academy of Dermatology in 2014.[37]
Prognosis
[edit]A 2014 study classified cases into three types—EBS, JEB and DEB—and reviewed their times of death. The first two types tended to die in infancy and the last in early adulthood.[38] In a survey of 11 families affected by the disease, lack of awareness of the disease by both the public and health care providers raised concerns about the care provided.[5]
Epidemiology
[edit]An estimated 20 per million live births are diagnosed with EB,[39] and 9 per million people in the general population have the condition. Of these cases, approximately 92% are EBS, 5% are DEB, 1% are JEB, and 2% are unclassified. Carrier frequency ranges from 1 in 333 for JEB, to 1 in 450 for DEB; the carrier frequency for EBS is presumed to be much higher than JEB or DEB.[citation needed]
The disorder occurs in every racial and ethnic group and affects both sexes.[40][41]
Society and culture
[edit]In 2010, Emma Fogarty, a campaigner for DEBRA Ireland (the EB charity), was awarded a People of the Year Award.[42] Actor Colin Farrell has campaigned with Fogarty on behalf of affected people.[43]
In 2014, Pearl Jam lead vocalist Eddie Vedder together with his wife Jill McCormick co-founded the EB Research Partnership,[44] a non-profit organization dedicated to finding a cure for EB.[45] McCormick is childhood friends with Ryan Fullmer, whose son, Michael, was born with EB. Vedder, McCormick, Ryan Fullmer, and his wife Heather founded Heal EB. In 2014, they merged Heal EB with the Jackson Gabriel Research Foundation to create the EB Research Partnership. The EBRP hosts several annual fundraising events. To date, they have raised $12 million to fund research to find a cure.[46]
On 1 March 2019, heavyweight boxer Luis Ortiz was named an honorary ambassador for the EB community by the EB Research Partnership. Ortiz's daughter, Lismercedes, was born with EB.[47]
Television
[edit]The condition was brought to public attention in 2004 in the UK through the Channel 4 documentary The Boy Whose Skin Fell Off, chronicling the life and death of Jonny Kennedy, an Englishman with EB.[48] In the United States, HBO ran a documentary, My Flesh and Blood, in 2003.[citation needed] Additionally, the film Butterfly Girl follows Abigail Evans with the disease.[49] In Canada, The Sports Network's award-winning documentary on Jonathan Pitre led to extensive coverage on the boy's disease, treatment, and death.[50][51]
Other names
[edit]Other terms used to describe those affected include "butterfly children" as the skin is fragile as a butterfly's wings,[52] "cotton wool babies",[53][54] or "crystal skin children".[55]
References
[edit]- ^ Fine JD, Hintner H (2009). Life with Epidermolysis Bullosa (EB): Etiology, Diagnosis, Multidisciplinary Care and Therapy. Springer Science & Business Media. p. 242. ISBN 9783211792711. Archived from the original on 3 November 2021. Retrieved 21 November 2020.
- ^ a b c d e "Epidermolysis bullosa". rarediseases.info.nih.gov. Archived from the original on 16 May 2018. Retrieved 16 May 2018.
- ^ "Epidermolysis Bullosa". National Institute of Arthritis and Musculoskeletal and Skin Diseases. 11 April 2017. Archived from the original on 4 October 2017. Retrieved 16 May 2018.
- ^ "Epidermolysis Bullosa". National Institute of Arthritis and Musculoskeletal and Skin Diseases. 11 April 2017. Archived from the original on 4 October 2017. Retrieved 16 May 2018.
- ^ a b c d e f g Tabor A, Pergolizzi JV J, Marti G, Harmon J, Cohen B, Lequang JA (May 2017). "Raising Awareness Among Healthcare Providers about Epidermolysis Bullosa and Advancing Toward a Cure". The Journal of Clinical and Aesthetic Dermatology. 10 (5): 36–48. PMC 5479476. PMID 28670357.
- ^ "Epidermolysis Bullosa". National Institute of Arthritis and Musculoskeletal and Skin Diseases. 11 April 2017. Archived from the original on 4 October 2017. Retrieved 16 May 2018.
- ^ a b Bardhan A, Bruckner-Tuderman L, Chapple IL, Fine JD, Harper N, Has C, et al. (24 September 2020). "Epidermolysis bullosa". Nature Reviews Disease Primers. 6 (1): 78. doi:10.1038/s41572-020-0210-0. ISSN 2056-676X. PMID 32973163. S2CID 221861310. Archived from the original on 18 November 2020. Retrieved 26 September 2020.
- ^ FINE JD, JOHNSON LB, WEINER M, STEIN A, CASH S, DeLEOZ J, et al. (November 2004). "Genitourinary Complications of Inherited Epidermolysis Bullosa: Experience of the National Epidermylosis Bullosa Registry and Review of the Literature". Journal of Urology. 172 (5): 2040–2044. doi:10.1097/01.ju.0000143200.86683.2c. PMID 15540785.
- ^ Vanden Oever M, Twaroski K, Osborn MJ, Wagner JE, Tolar J (1 November 2017). "Inside out: regenerative medicine for recessive dystrophic epidermolysis bullosa". Pediatric Research. 83 (1–2): 318–324. doi:10.1038/pr.2017.244. ISSN 0031-3998. PMID 29593249. S2CID 4447720.
- ^ "Epidermolysis Bullosa". National Institute of Arthritis and Musculoskeletal and Skin Diseases. 11 April 2017. Archived from the original on 4 October 2017. Retrieved 16 May 2018.
- ^ Koshida S, Tsukamura A, Yanagi T, Nakahara S, Takeuchi Y, Kato T, et al. (2013). "Hallopeau-Siemens dystrophic epidermolysis bullosa due to homozygous 5818delC mutation in the COL7A gene". Pediatr Int. 55 (2): 234–7. doi:10.1111/j.1442-200X.2012.03638.x. PMID 23679163. S2CID 24238328.
- ^ James, William; Berger, Timothy; Elston, Dirk (2005). Andrews' Diseases of the Skin: Clinical Dermatology. (10th ed.). Saunders. ISBN 0-7216-2921-0.
- ^ a b Freedberg, et al. (2003). Fitzpatrick's Dermatology in General Medicine. (6th ed.). McGraw-Hill. ISBN 0-07-138076-0.
- ^ "Junctional epidermolysis bullosa". Genetics Home Reference. NIH. Archived from the original on 12 October 2013. Retrieved 11 October 2013.
- ^ Varki R, Sadowski S, Uitto J, Pfendner E (1 March 2007). "Epidermolysis bullosa. II. Type VII collagen mutations and phenotype–genotype correlations in the dystrophic subtypes". Journal of Medical Genetics. 44 (3): 181–192. doi:10.1136/jmg.2006.045302. ISSN 0022-2593. PMC 2598021. PMID 16971478.
- ^ McGRATH J, Schofield O, Eady R (1 May 1994). "Epidermolysis bullosa pruriginosa: dystrophic epidermolysis bullosa with distinctive clinicopathological features". British Journal of Dermatology. 130 (5): 617–625. doi:10.1111/j.1365-2133.1994.tb13109.x. ISSN 1365-2133. PMID 8204470. S2CID 5958915.
- ^ "Epidermolysis Bullosa". NORD (National Organization for Rare Disorders). Archived from the original on 8 March 2022. Retrieved 8 March 2022.
- ^ Cianfarani F, Zambruno G, Castiglia D, Odorisio T (July 2017). "Pathomechanisms of Altered Wound Healing in Recessive Dystrophic Epidermolysis Bullosa". The American Journal of Pathology. 187 (7): 1445–1453. doi:10.1016/j.ajpath.2017.03.003. ISSN 0002-9440. PMID 28460207.
- ^ Mallipeddi R (November 2002). "Epidermolysis bullosa and cancer". Clinical and Experimental Dermatology. 27 (8): 616–623. doi:10.1046/j.1365-2230.2002.01130.x. ISSN 0307-6938. PMID 12472531. S2CID 40006559. Archived from the original on 8 March 2022. Retrieved 8 March 2022.
- ^ Anderson TR, Slotkin TA (15 August 1975). "Maturation of the adrenal medulla--IV. Effects of morphine". Biochemical Pharmacology. 24 (16): 1469–1474. doi:10.1016/0006-2952(75)90020-9. ISSN 1873-2968. PMID 7.
- ^ Kerns ML, DePianto D, Dinkova-Kostova AT, Talalay P, Coulombe PA (4 September 2007). "Reprogramming of keratin biosynthesis by sulforaphane restores skin integrity in epidermolysis bullosa simplex". Proceedings of the National Academy of Sciences. 104 (36): 14460–14465. Bibcode:2007PNAS..10414460K. doi:10.1073/pnas.0706486104. ISSN 0027-8424. PMC 1964870. PMID 17724334.
- ^ "My Skin is Killing Me - Epidermolysis Bullosa | Extraordinary People Documentary | Reel Truth". YouTube. 29 June 2018.
- ^ Josephine Marcotty (3 July 2008). "Long-shot stem-cell treatment gives two brothers a future". Star Tribune. Archived from the original on 11 February 2009. Retrieved 22 July 2008.
- ^ a b Souillet G, Guffon N, Maire I, Pujol M, Taylor P, Sevin F, et al. (10 June 2003). "Outcome of 27 patients with Hurler's syndrome transplanted from either related or unrelated haematopoietic stem cell sources". Bone Marrow Transplantation. 31 (12): 1105–17. doi:10.1038/sj.bmt.1704105. PMID 12796790. S2CID 30326472.
- ^ Wagner JE, Ishida-Yamamoto A, McGrath JA, Hordinsky M, Keene DR, Riddle MJ, et al. (12 August 2010). "Bone Marrow Transplantation for Recessive Dystrophic Epidermolysis Bullosa". The New England Journal of Medicine. 363 (7): 629–639. doi:10.1056/NEJMoa0910501. ISSN 0028-4793. PMC 2967187. PMID 20818854.
- ^ Fine JD, Manes B, Frangoul H (July 2015). "Systemic granulocyte colony-stimulating factor (G-CSF) enhances wound healing in dystrophic epidermolysis bullosa (DEB): Results of a pilot trial". Journal of the American Academy of Dermatology. 73 (1): 56–61. doi:10.1016/j.jaad.2015.04.015. ISSN 0190-9622. PMID 25956659.
- ^ Hirsch T, Rothoeft T, Teig N, Bauer JW, Pellegrini G, De Rosa L, et al. (16 November 2017). "Regeneration of the entire human epidermis using transgenic stem cells". Nature. 551 (7680): 327–332. Bibcode:2017Natur.551..327H. doi:10.1038/nature24487. PMC 6283270. PMID 29144448.
- ^ Siprashvili Z, Nguyen NT, Gorell ES, Loutit K, Khuu P, Furukawa LK, et al. (1 November 2016). "Safety and Wound Outcomes Following Genetically Corrected Autologous Epidermal Grafts in Patients With Recessive Dystrophic Epidermolysis Bullosa". JAMA. 316 (17): 1808–1817. doi:10.1001/jama.2016.15588. ISSN 1538-3598. PMID 27802546. Archived from the original on 8 March 2022. Retrieved 8 March 2022.
- ^ Pliszczyński J, Nita M, Kowalewski C, Woźniak K, Eljaszewicz A, Moniuszko M, et al. (September 2020). "Transplantation of a New Biological Product in Rare Diseases, Such as Epidermolysis Bullosa: Response and Clinical Outcome". Transplantation Proceedings. 52 (7): 2239–2243. doi:10.1016/j.transproceed.2020.02.119. ISSN 1873-2623. PMID 32334796. S2CID 216555379. Archived from the original on 8 March 2022. Retrieved 8 March 2022.
- ^ "Filsuvez EPAR". European Medicines Agency (EMA). 13 April 2022. Archived from the original on 6 July 2022. Retrieved 6 July 2022. Text was copied from this source which is copyright European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ^ "European Commission Approves Filsuvez for the treatment of Dystrophic and Junctional EB" (Press release). Amryt Pharma plc. 23 June 2022. Archived from the original on 23 June 2022. Retrieved 6 July 2022.
- ^ "Filsuvez- birch triterpenes gel". DailyMed. 14 February 2024. Retrieved 3 March 2024.
- ^ a b c "Filsuvez EPAR". European Medicines Agency (EMA). 13 April 2022. Archived from the original on 6 July 2022. Retrieved 6 July 2022. Text was copied from this source which is copyright European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ^ "Filsuvez, common birch bark extract" (PDF). European Medicines Agency (EMA). Archived (PDF) from the original on 15 July 2024. Retrieved 1 February 2024.
- ^ "Novel Drug Approvals for 2023". U.S. Food and Drug Administration (FDA). 19 December 2023. Archived from the original on 21 January 2023. Retrieved 22 December 2023.
- ^ "Drug Trials Snapshots: Filsuvez". U.S. Food and Drug Administration (FDA). 18 December 2023. Archived from the original on 15 July 2024. Retrieved 14 July 2024.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ Development, reliability, and validity of a novel Epidermolysis Bullosa Disease Activity and Scarring index (EBDASI). 2014. Loh CH, Kim J, Su JC, Daniel BS, Venugopal SS, Rhodes LM, Intong LR, Law MG, Murrell DF. January 2014. JAAD, 70, 1pp.
- ^ Hon KL, Li JJ, Cheng BL, Luk DC, Murrell DF, Choi PC, et al. (4 March 2015). "Age and etiology of childhood epidermolysis bullosa mortality". Journal of Dermatological Treatment. 26 (2): 178–182. doi:10.3109/09546634.2014.915002. ISSN 0954-6634. PMID 24724596. S2CID 33722635.
- ^ "Epidermolysis Bullosa Clinic Frequently Asked Questions". Stanford Medicine — Dermatology. Archived from the original on 8 March 2018. Retrieved 13 April 2018.
- ^ Marinkovich MP, Wells MJ, Perry V, James WD, Ortonne JP (3 December 2007). "Epidermolysis Bullosa". Bullous Diseases. emedicine.com. Archived from the original on 25 October 2008. Retrieved 22 July 2008.
- ^ Pfendner E, Uitto J, Fine JD (7 November 2000). "Epidermolysis Bullosa Carrier Frequencies in the US Population". Journal of Investigative Dermatology. 116 (3): 483–484. doi:10.1046/j.1523-1747.2001.127911.x. PMID 11231335.
- ^ Kiernan L (21 December 2018). "A brave Laois woman is among the guests for tonight's Late Late Show". Leinster Express. Archived from the original on 21 December 2018. Retrieved 21 December 2018.
- ^ Townsend M (21 December 2018). "Late Late Show viewers praise Colin Farrell and EB sufferer Emma Fogarty for honest interview". RSVP live. Archived from the original on 22 December 2018.
- ^ "Board of Directors - EB Research Partnership". ebresearch.org. Archived from the original on 27 March 2019. Retrieved 22 March 2019.
- ^ Reed R (10 October 2014). "Eddie Vedder Supports Research for Curing Rare Skin Disease EB". Rolling Stone. Archived from the original on 22 March 2019. Retrieved 22 March 2019.
- ^ Lee K (11 November 2016). "Eddie Vedder and the Chicago Cubs Team Up to Raise $50,000 to Help Kids with EB". Medium. Archived from the original on 22 March 2019. Retrieved 22 March 2019.
- ^ "Luis Ortiz named ambassador for Epidermolysis Bullosa Research Partnership". World Boxing News. 1 March 2009. Archived from the original on 22 March 2019. Retrieved 22 March 2019.
- ^ "Series 1 - The Boy Whose Skin Fell Off". Channel 4. 2004. Archived from the original on 28 April 2016. Retrieved 28 February 2009.
- ^ "Butterfly Girl: Remembering Abigail Evans". The Austinot. 12 January 2015. Archived from the original on 13 July 2017.
- ^ Andrew Duffy, "TSN documentary on Jonathan Pitre wins screen award". Ottawa Citizen. 9 March 2016. Archived from the original on 6 April 2018. Retrieved 6 April 2018.
- ^ "Ottawa boy Jonathan Pitre dead at 17 from rare skin disease". CBC News. 6 April 2018. Archived from the original on 8 April 2018.
- ^ Roddy Isles, Head of Press (12 May 2005). "Dundee Scientists on road to cure for "Butterfly Children" condition". University of Dundee. Archived from the original on 4 January 2014. Retrieved 22 July 2008.
- ^ Suellen Hinde, Health reporter (26 November 2006). "Little girl's life of pain". HeraldSun.com.au. Archived from the original on 22 September 2008. Retrieved 22 July 2008.
- ^ Robyn Gobert, Past President of DEBRA Australia Inc. (May 2002). "Times change - A family's story about living with EB". e-bility.com. Archived from the original on 3 July 2008. Retrieved 22 July 2008.
- ^ Gena Brumitt Gruschovnik, DEBRA International Executive Committee. "DEBRA Chile website". Archived from the original on 20 December 2008. Retrieved 19 December 2008.
External links
[edit]- GeneReviews/NCBI/UW/NIH entry on Epidermolysis Bullosa Simplex
- Questions and Answers about Epidermolysis Bullosa - US National Institute of Arthritis and Musculoskeletal and Skin Diseases
