Respirator
| Respirator | |
|---|---|
 White, disposable cup N95 filtering facepiece respirator | |
| Other name(s) | mask |
| Regulated by | National Institute for Occupational Safety and Health, National Fire Protection Association, American National Standards Institute, Food and Drug Administration |
| Regulation | 42 CFR 84, NFPA 1981, ANSI Z88.7-2001, 21 CFR 878.4040, EN 143, EN 149, EN 137, EN 14387 |
A respirator is a device designed to protect the wearer from inhaling hazardous atmospheres including lead fumes, vapors, gases and particulate matter such as dusts and airborne pathogens such as viruses. There are two main categories of respirators: the air-purifying respirator, in which respirable air is obtained by filtering a contaminated atmosphere, and the air-supplied respirator, in which an alternate supply of breathable air is delivered. Within each category, different techniques are employed to reduce or eliminate noxious airborne contaminants.

Air-purifying respirators range from relatively inexpensive, single-use, disposable face masks, known as filtering facepiece respirators, reusable models with replaceable cartridges called elastomeric respirators, to powered air-purifying respirators (PAPR), which use a pump or fan to constantly move air through a filter and supply purified air into a mask, helmet or hood.
History
[edit]Earliest records to 19th century
[edit]
The history of protective respiratory equipment can be traced back as far as the first century, when Pliny the Elder (c. 23 AD–79) described using animal bladder skins to protect workers in Roman mines from red lead oxide dust.[1] In the 16th century, Leonardo da Vinci suggested that a finely woven cloth dipped in water could protect sailors from a toxic weapon made of powder that he had designed.[2]
Alexander von Humboldt introduced a primitive respirator in 1799 when he worked as a mining engineer in Prussia.[3]
Julius Jeffreys first used the word "respirator" as a mask in 1836.[4]

In 1848, the first US patent for an air-purifying respirator was granted to Lewis P. Haslett[5] for his 'Haslett's Lung Protector,' which filtered dust from the air using one-way clapper valves and a filter made of moistened wool or a similar porous substance.[6] Hutson Hurd patented a cup-shaped mask in 1879 which became widespread in industrial use.[7]
Inventors in Europe included John Stenhouse, a Scottish chemist, who investigated the power of charcoal in its various forms, to capture and hold large volumes of gas. He built one of the first respirators able to remove toxic gases from the air, paving the way for activated charcoal to become the most widely used filter for respirators.[8] Irish physicist John Tyndall took Stenhouse's mask, added a filter of cotton wool saturated with lime, glycerin, and charcoal, and in 1871 invented a 'fireman's respirator', a hood that filtered smoke and gas from air, which he exhibited at a meeting of the Royal Society in London in 1874.[9] Also in 1874, Samuel Barton patented a device that 'permitted respiration in places where the atmosphere is charged with noxious gases, or vapors, smoke, or other impurities.'[10][11]
In the late 19th century, Miles Philips began using a "mundebinde" ("mouth bandage") of sterilized cloth which he refined by adapting a chloroform mask with two layers of cotton mull.[12]
20th century
[edit]
In the winter of 1910, Wu was given instructions from the Foreign Office of the Imperial Qing court[13] in Peking, to travel to Harbin to investigate an unknown disease that killed 99.9% of its victims.[14] This was the beginning of the large pneumonic plague epidemic of Manchuria and Mongolia, which ultimately claimed 60,000 lives.[15]
Wu was able to conduct a postmortem (usually not accepted in China at the time) on a Japanese woman who had died of the plague.[16][17] Having ascertained via the autopsy that the plague was spreading by air, Wu developed surgical masks into more substantial masks with layers of gauze and cotton to filter the air.[18][19] Gérald Mesny, a prominent French doctor who had come to replace Wu, refused to wear a mask and died days later of the plague.[17][18][16] The mask was widely produced, with Wu overseeing the production and distribution of 60,000 masks in a later epidemic, and it featured in many press images.[20][18]World War I
[edit]The First World War brought about the first need for mass-produced gas masks on both sides because of extensive use of chemical weapons. The German army successfully used poison gas for the first time against Allied troops at the Second Battle of Ypres, Belgium on April 22, 1915.[21] An immediate response was cotton wool wrapped in muslin, issued to the troops by May 1. This was followed by the Black Veil Respirator, invented by John Scott Haldane, which was a cotton pad soaked in an absorbent solution which was secured over the mouth using black cotton veiling.[22]
Seeking to improve on the Black Veil respirator, Cluny Macpherson created a mask made of chemical-absorbing fabric which fitted over the entire head: a 50.5 cm × 48 cm (19.9 in × 18.9 in) canvas hood treated with chlorine-absorbing chemicals, and fitted with a transparent mica eyepiece.[23][24] Macpherson presented his idea to the British War Office Anti-Gas Department on May 10, 1915; prototypes were developed soon after.[25] The design was adopted by the British Army and introduced as the British Smoke Hood in June 1915; Macpherson was appointed to the War Office Committee for Protection against Poisonous Gases.[26] More elaborate sorbent compounds were added later to further iterations of his helmet (PH helmet), to defeat other respiratory poison gases used such as phosgene, diphosgene and chloropicrin. In summer and autumn 1915, Edward Harrison, Bertram Lambert and John Sadd developed the Large Box Respirator.[27] This canister gas mask had a tin can containing the absorbent materials by a hose and began to be issued in February 1916. A compact version, the Small Box Respirator, was made a universal issue from August 1916.[citation needed]United States
[edit]
Prior to the 1970s, respirator standards were under the purview of the US Bureau of Mines (USBM). An example of an early respirator standard, Type A, established in 1926, was intended to protect against mechanically generated dusts produced in mines. These standards were intended to obviate miner deaths, noted to have reached 3,243 by 1907. However, prior to the Hawks Nest Tunnel Disaster, these standards were merely advisory, as the USBM had no enforcement power at the time.[28] After the disaster, an explicit approval program was established in 1934, along with the introduction of combination Type A/B/C respirator ratings, corresponding to Dusts/Fumes/Mists respectively, with Type D blocking all three, under 30 CFR 14 Schedule 21.[29]
The Federal Coal Mine Health and Safety Act establishing MESA (later MSHA),[30] the Occupational Safety and Health Act of 1970, establishing NIOSH,[31] as well as other regulations established around the time, reshuffled regulatory authority for respirators, and moved regulations from Part 14 to Part 11 by 1972,[32] but nonetheless continued the use of USBM-era regulations.[29]In the 1970s, the successor to the United States Bureau of Mines and NIOSH developed standards for single-use respirators, and the first single-use respirator was developed by 3M and approved in 1972.[33] 3M used a melt blowing process that it had developed decades prior and used in products such as ready-made ribbon bows and bra cups; its use in a wide array of products had been pioneered by designer Sara Little Turnbull.[34]
1990s
[edit]Historically, respirators in the US had generally been approved by MESA/MSHA/NIOSH under federal regulation 30 CFR 11. On July 10, 1995, in response to respirators exhibiting "low initial efficiency levels", new 42 CFR 84 standards, including the N95 standard, were enforced under a three-year transition period,[35] ending on July 10, 1998.[32] The standard for N95 respirators includes, but is not limited to, a filtration of at least 95% under a 0.3 micrometer[36] 200 milligram test load of sodium chloride. Standards and specifications are also subject to change.[37][32]
Once 42 CFR 84 was in effect, MSHA, under a proposed rule change to 30 CFR 11, 70, and 71, would withdraw from the approval process of rated respirators (outside of respirators used for mining).[38][39]
21st century
[edit]2020
[edit]China normally makes 10 million masks per day, about half of the world production. During the COVID-19 pandemic, 2,500 factories were converted to produce 116 million daily.[40]
During the COVID-19 pandemic, people in the United States, and in a lot of countries in the world, were urged to make their own cloth masks due to the widespread shortage of commercial masks.[41]
2024
[edit]Summary of modern respirators
[edit]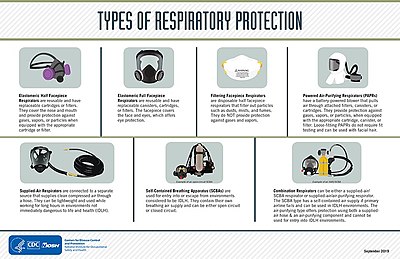
All respirators have some type of facepiece held to the wearer's head with straps, a cloth harness, or some other method. Facepieces come in many different styles and sizes to accommodate all types of face shapes.
A full facepiece covers the mouth, nose and eyes and if sealed, is sealed round the perimeter of the face. Unsealed versions may be used when air is supplied at a rate which prevents ambient gas from reaching the nose or mouth during inhalation.
Respirators can have half-face forms that cover the bottom half of the face including the nose and mouth, and full-face forms that cover the entire face. Half-face respirators are only effective in environments where the contaminants are not toxic to the eyes or facial area.
An escape respirator may have no component that would normally be described as a mask, and may use a bite-grip mouthpiece and nose clip instead. Alternatively, an escape respirator could be a time-limited self-contained breathing apparatus.
For hazardous environments, like confined spaces, atmosphere-supplying respirators, like SCBAs, should be used.
A wide range of industries use respirators including healthcare & pharmaceuticals, defense & public safety services (defense, firefighting & law enforcement), oil and gas industries, manufacturing (automotive, chemical, metal fabrication, food and beverage, wood working, paper and pulp), mining, construction, agriculture and forestry, cement production, power generation, painting, shipbuilding, and the textile industry.[45]
Respirators require user training in order to provide proper protection.
Use
[edit]User seal check
[edit]
Each time a wearer dons a respirator, they must perform a seal check to be sure that they have an airtight seal to the face so that air does not leak around the edges of the respirator. (PAPR respirators may not require this because they don't necessarily seal to the face.) This check is different than the periodic fit test that is performed by specially trained personnel using testing equipment. Filtering facepiece respirators are typically checked by cupping the hands over the facepiece while exhaling (positive pressure check) or inhaling (negative pressure check) and observing any air leakage around the facepiece. Elastomeric respirators are checked in a similar manner, except the wearer blocks the airways through the inlet valves (negative pressure check) or exhalation valves (positive pressure check) while observing the flexing of the respirator or air leakage. Manufacturers have different methods for performing seal checks and wearers should consult the specific instructions for the model of respirator they are wearing. Some models of respirators or filter cartridges have special buttons or other mechanisms built into them to facilitate seal checks.[46]
Fit testing
[edit]A respirator fit test checks whether a respirator properly fits the face of someone who wears it. The fitting characteristic of a respirator is the ability of the mask to separate a worker's respiratory system from ambient air.
This is achieved by tightly pressing the mask flush against the face (without gaps) to ensure an efficient seal on the mask perimeter. Because wearers cannot be protected if there are gaps, it is necessary to test the fit before entering into contaminated air. Multiple forms of the test exist.Contrast with surgical mask
[edit]
A surgical mask is a loosely-placed, unsealed barrier, meant to stop droplets, and other liquid-borne particles from the mouth and nose that may contain pathogens.[47]
A surgical mask may not block all particles, due to the lack of fit between the surface of the face mask and the face.[47] The filtration efficiency of a surgical mask ranges between 10% and 90% for any given manufacturer, when measured using tests required for NIOSH certification. A study found that 80–100% of subjects failed an OSHA-accepted qualitative fit test, and a quantitative test showed between 12 and 25% leakage.[48]
A CDC study found that in public indoor settings, consistently wearing a respirator was linked to a 83% lower risk of testing positive for COVID-19, as compared to a 66% reduction when using surgical masks, and 56% for cloth.[49]Surgical N95
[edit]
Respirators used in healthcare are traditionally a specific variant called a surgical respirator, which is both approved by NIOSH as a respirator and cleared by the Food and Drug Administration as a medical device similar to a surgical mask.[50] These may also be labeled "Surgical N95", "medical respirators", or "healthcare respirators".[51] The difference lies in the extra fluid-resistant layer outside, typically colored blue.[52] In addition to 42 CFR 84, surgical N95s are regulated under FDA regulation 21 CFR 878.4040.[53]
In the United States, the Occupational Safety and Health Administration (OSHA) requires healthcare workers who are expected to perform patient activities with those suspected or confirmed to be infected with COVID-19 to wear respiratory protection, such as an N95 respirator.[54] The CDC recommends the use of respirators with at least N95 certification to protect the wearer from inhalation of infectious particles including Mycobacterium tuberculosis, avian influenza, severe acute respiratory syndrome (SARS), pandemic influenza, and Ebola.[55]Respirator selection
[edit]Air-purifying respirators are respirators that draw in the surrounding air and purify it before it is breathed (unlike air-supplying respirators, which are sealed systems, with no air intake, like those used underwater). Air-purifying respirators filter particulates, gases, and vapors from the air, and may be negative-pressure respirators driven by the wearer's inhalation and exhalation, or positive-pressure units such as powered air-purifying respirators (PAPRs).
According to the NIOSH Respirator Selection Logic, air-purifying respirators are recommended for concentrations of hazardous particulates or gases that are greater than the relevant occupational exposure limit but less than the immediately dangerous to life or health level and the manufacturer's maximum use concentration, subject to the respirator having a sufficient assigned protection factor. For substances hazardous to the eyes, a respirator equipped with a full facepiece, helmet, or hood is recommended. Air-purifying respirators are not effective during firefighting, in oxygen-deficient atmosphere, or in an unknown atmosphere; in these situations a self-contained breathing apparatus is recommended instead.[56]
Types of filtration
[edit]Mechanical filter
[edit]- Main Article: Mechanical filter respirator (and regulatory ratings)
Mechanical filters remove contaminants from air in several ways: interception when particles following a line of flow in the airstream come within one radius of a fiber and adhere to it; impaction, when larger particles unable to follow the curving contours of the airstream are forced to embed in one of the fibers directly; this increases with diminishing fiber separation and higher air flow velocity; by diffusion, where gas molecules collide with the smallest particles, especially those below 100 nm in diameter, which are thereby impeded and delayed in their path through the filter, increasing the probability that particles will be stopped by either of the previous two mechanisms; and by using an electrostatic charge that attracts and holds particles on the filter surface.
There are many different filtration standards that vary by jurisdiction. In the United States, the National Institute for Occupational Safety and Health defines the categories of particulate filters according to their NIOSH air filtration rating. The most common of these are the N95 respirator, which filters at least 95% of airborne particles but is not resistant to oil.
Other categories filter 99% or 99.97% of particles, or have varying degrees of resistance to oil.[57]
In the European Union, European standard EN 143 defines the 'P' classes of particle filters that can be attached to a face mask, while European standard EN 149 defines classes of "filtering half masks" or "filtering facepieces", usually called FFP masks.[58]
According to 3M, the filtering media in respirators made according to the following standards are similar to U.S. N95 or European FFP2 respirators, however, the construction of the respirators themselves, such as providing a proper seal to the face, varies considerably. (For example, US NIOSH-approved respirators never include earloops because they don't provide enough support to establish a reliable, airtight seal.) Standards for respirator filtration the Chinese KN95, Australian / New Zealand P2, Korean 1st Class also referred to as KF94, and Japanese DS.[59]
Canister or chemical cartridge
[edit]
Chemical cartridges and gas mask canisters remove gases, volatile organic compounds (VOCs), and other vapors from breathing air by adsorption, absorption, or chemisorption. A typical organic vapor respirator cartridge is a metal or plastic case containing from 25 to 40 grams of sorption media such as activated charcoal or certain resins. The service life of the cartridge varies based, among other variables, on the carbon weight and molecular weight of the vapor and the cartridge media, the concentration of vapor in the atmosphere, the relative humidity of the atmosphere, and the breathing rate of the respirator wearer. When filter cartridges become saturated or particulate accumulation within them begins to restrict air flow, they must be changed.[60]
If the concentration of harmful gases is immediately dangerous to life or health, in workplaces covered by the Occupational Safety and Health Act the US Occupational Safety and Health Administration specifies the use of air-supplied respirators except when intended solely for escape during emergencies.[61] NIOSH also discourages their use under such conditions.[62]
Air-purifying respirators
[edit]Filtering facepiece
[edit]
Elastomeric
[edit]
Elastomeric respirators, also called reusable air-purifying respirators,[66] seal to the face with elastomeric material, which may be a natural or synthetic rubber. They are generally reusable. Full-face versions of elastomeric respirators seal better and protect the eyes.[67]
Elastomeric respirators consist of a reusable mask that seals to the face, with exchangeable filters.[68][69] Elastomeric respirators can be used with chemical cartridge filters that remove gases, mechanical filters that retain particulate matter, or both.[70] As particulate filters, they are comparable[68] (or, due to the quality and error-tolerance of the elastomeric seal, possibly superior[70]) to filtering facepiece respirators such as most disposable N95 respirators and FFP masks.[68]Powered air-purifying respirators
[edit]Atmosphere-supplying respirators
[edit]These respirators do not purify the ambient air, but supply breathing gas from another source. The three types are the self contained breathing apparatus, in which a compressed air cylinder is worn by the wearer; the supplied air respirators, where a hose supplies air from a stationary source; and combination supplied-air respirators, with an emergency backup tank.[71]
Self-contained breathing apparatus
[edit]A self-contained breathing apparatus (SCBA) is a respirator worn to provide an autonomous supply of breathable gas in an atmosphere that is immediately dangerous to life or health from a gas cylinder.[72] They are typically used in firefighting and industry. The term self-contained means that the SCBA is not dependent on a remote supply of breathing gas (e.g., through a long hose). They are sometimes called industrial breathing sets. Some types are also referred to as a compressed air breathing apparatus (CABA) or simply breathing apparatus (BA). Unofficial names include air pack, air tank, oxygen cylinder or simply pack, terms used mostly in firefighting. If designed for use under water, it is also known as a scuba set (self-contained underwater breathing apparatus).
An open circuit SCBA typically has three main components: a high-pressure gas storage cylinder, (e.g., 2,216 to 5,500 psi (15,280 to 37,920 kPa), about 150 to 374 atmospheres), a pressure regulator, and a respiratory interface, which may be a mouthpiece, half mask or full-face mask, assembled and mounted on a framed carrying harness.[73]
A self-contained breathing apparatus may fall into one of three categories: open-circuit, closed-circuit,[74] or continuous-flow.[75]Supplied air respirator
[edit]Escape respirators
[edit]
Smoke hood
[edit]Self-contained breathing apparatus
[edit]Continuous-flow
[edit]Self-rescue device
[edit]A self-contained self-rescue device, SCSR, self-contained self-rescuer, or air pack is a type of closed-circuit SCBA[87] with a portable oxygen source for providing breathable air when the surrounding atmosphere lacks oxygen or is contaminated with toxic gases, e.g. carbon monoxide.
Self-rescuers are intended for use in environments such as coal mines where there is a risk of fire or explosion, and in a location where no external rescue may be available for some time – the wearer must make their own way to safety, or to some pre-equipped underground refuge. The main hazard here is from large quantities of carbon monoxide or whitedamp, often produced by an explosion of firedamp. In some industries, the hazard may be from anoxic asphyxia, or a lack of oxygen, rather than poisoning by something toxic.
Self-rescuers are small, lightweight belt or harness-worn devices, enclosed in a rugged metal case. They are designed to have a long service life of around 10 years (longer for shelf storage) and to be worn every day by each miner. Once used, they have a working life of a few hours and are discarded after opening.Disadvantages
[edit]| This article is part of a series on |
| Respirators in the United States |
|---|
| Executive agencies involved |
| Non-government bodies |
| Respirator regulation |
| Diseases mitigated by respirators |
| Misuse |
| Related topics involving respirators |
Hierarchy of Controls point of view
[edit]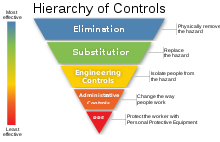
The Hierarchy of Controls, noted as part of the Prevention Through Design initiative started by NIOSH with other standards bodies, is a set of guidelines emphasizing building in safety during design, as opposed to ad-hoc solutions like PPE, with multiple entities providing guidelines on how to implement safety during development[88] outside of NIOSH-approved respirators. US Government entities currently and formerly involved in the regulation of respirators follow the Hierarchy of Controls, including OSHA[89] and MSHA.[90]
However, some HOC implementations, notably MSHA's, have been criticized for allowing mining operators to skirt engineering control noncompliance by requiring miners to wear respirators instead if the permissible exposure limit (PEL) is exceeded, without work stoppages, breaking the hierarchy of engineering controls. Another concern was fraud related to the inability to scrutinize engineering controls,[91][92] unlike NIOSH-approved respirators, like the N95, which can be fit tested by anyone, are subject to the scrutiny of NIOSH, and are trademarked and protected under US federal law.[93]
Respirator non-compliance
[edit]With regards to people complying with requirements to wear respirators, various papers note high respirator non-compliance across industries,[94][95] with a survey noting non-compliance was due in large part due to discomfort from temperature increases along the face, and a large amount of respondents also noting the social unacceptability of provided N95 respirators during the survey.[96] For reasons like mishandling, ill-fitting respirators and lack of training, the Hierarchy of Controls dictates respirators be evaluated last while other controls exist and are working. Alternative controls like hazard elimination, administrative controls, and engineering controls like ventilation are less likely to fail due to user discomfort or error.[97][98]
A U.S. Department of Labor study[99] showed that in almost 40 thousand American enterprises, the requirements for the correct use of respirators are not always met. Experts note that in practice it is difficult to achieve elimination of occupational morbidity with the help of respirators:
It is well known how ineffective ... trying to compensate the harmful workplace conditions with ... the use of respirators by employees.[100] Unfortunately, the only certain way of reducing the exceedance fraction to zero is to ensure that Co (note: Co - concentration of pollutants in the breathing zone) never exceeds the PEL value.[101]
Beards
[edit]
Certain types of facial hair can reduce fit to a significant degree. For this reason, there are facial hair guidelines for respirator users.[102] This is another example of potential respirator non-compliance.
Counterfeiting, modification, and revocation of regulated respirators
[edit]

Another disadvantage of respirators is that the onus is on the respirator user to determine if their respirator is counterfeit or has had its certification revoked.[93] Customers and employers can inadvertently purchase non-OEM parts for a NIOSH-approved respirator which void the NIOSH approval and violate OSHA laws, in addition to potentially compromising the fit of the respirator.[103] This is another example of respirator mishandling under the Hierarchy of Controls.
Issues with fit testing
[edit]If respirators must be used, under 29 CFR 1910.134, OSHA requires respirator users to conduct a respirator fit test, with a safety factor of 10 to offset lower fit during real world use.[89] However, NIOSH notes the large amount of time required for fit testing has been a point of contention for employers.[104]
Other opinions concern the change in performance of respirators in use compared to when fit testing, and compared to engineering control alternatives:
The very limited field tests of air-purifying respirator performance in the workplace show that respirators may perform far less well under actual use conditions than is indicated by laboratory fit factors. We are not yet able to predict the level of protection accurately; it will vary from person to person, and it may also vary from one use to the next for the same individual. In contrast, we can predict the effectiveness of engineering controls, and we can monitor their performance with commercially available state-of-the-art devices.[105]
Issues with respirator design
[edit]Extended use of certain negative-pressure respirators can result in higher levels of carbon dioxide from dead space and breathing resistance (pressure drop) which can impact functioning and sometimes can exceed the PEL.[106][107][108] This effect was significantly reduced with powered air purifying respirators.[109] Certain respirator designs, especially those with head straps, can also lead to headaches,[110] dermatitis and acne.[111]
Complaints have been leveled at early LANL NIOSH fit test panels (which included primarily military personnel) as being unrepresentative of the broader American populace.[112] However, later fit test panels, based on a NIOSH facial survey conducted in 2003, were able to reach 95% representation of working US population surveyed.[113] Despite these developments, 42 CFR 84, the US regulation NIOSH follows for respirator approval, allows for respirators that don't follow the NIOSH fit test panel provided that: more than one facepiece size is provided, and no chemical cartridges are made available.[114]
Issues with lack of regulation
[edit]Respirators designed to non-US standards may not be subject to as much or any scrutiny:
- In China, under GB2626-2019, which includes standards like KN95, there is no procedure for fit testing.[115]
Some jurisdictions allow for respirator filtration ratings lower than 95%, respirators which are not rated to prevent respiratory infection, asbestos, or other dangerous occupational hazards. These respirators are sometimes known as dust masks for their almost exclusive approval only against dust nuisances:
- In Europe, regulation allows for dust masks under FFP1, where 20% inward leakage is allowed, with a minimum filtration efficiency of 80%.[116]
- South Korea allows 20% filter leakage under KF80.
In the US, NIOSH noted that under standards predating the N95, 'Dust/Mist' rated respirators could not prevent the spread of TB.[117]
Regulation
[edit]The choice and use of respirators in developed countries is regulated by national legislation. To ensure that employers choose respirators correctly, and perform high-quality respiratory protection programs, various guides and textbooks have been developed:
| Textbooks and guidelines for the selection and use of respirators | ||||
|---|---|---|---|---|
| Country | Language | Year of publication | Pages | Institution (hyperlink to document) |
| US | English | 1987 | 305 | NIOSH ([118]) |
| US | English | 2005 | 32 | NIOSH ([119]) |
| US | English | 1999 | 120 | NIOSH ([120]) |
| US | English | 2017 | 48 | Pesticide Educational Resources Collaborative (PERC) ([121]) |
| US | English & Spanish | - | - | OSHA ([122]) |
| US | English | 2011 | 124 | OSHA ([123]) |
| US | English | 2015 | 96 | OSHA ([124]) |
| US | English | 2012 | 44 | OSHA ([125]) |
| US | English | 2014 | 44 | OSHA ([126]) |
| US | English | 2016 | 32 | OSHA ([127]) |
| US | English | 2014 | 38 | OSHA ([128]) |
| US | English | 2017 | 51 | OSHA ([129]) |
| US | English | 2001 | 166 | NRC ([130]) |
| US | English | 1986 | 173 | NIOSH & EPA ([131]) |
| Canada | French | 2013, 2002 | 60 | Institut de recherche Robert-Sauve en santé et en sécurité du travail (IRSST) ([132]) |
| Canada | English | 2015 | - | Institut de recherche Robert-Sauve en sante et en securite du travai (IRSST) ([133]) |
| Canada | French | 2015 | - | Institut de recherche Robert-Sauve en sante et en securite du travai (IRSST) ([134]) |
| France | French | 2017 | 68 | Institut National de Recherche et de Sécurité (INRS) ([135]) |
| Germany | German | 2011 | 174 | Spitzenverband der gewerblichen Berufsgenossenschaften und der Unfallversicherungsträger der öffentlichen Hand (DGUV) ([136]) |
| UK | English | 2013 | 59 | The Health and Safety Executive (HSE) ([137]) |
| UK | English | 2016 | 29 | The UK Nuclear Industry Good PracIndustry Radiological Protection Coordination Group (IRPCG) ([138]) |
| Ireland | English | 2010 | 19 | The Health and Safety Authority (HSA) ([139]) |
| New Zealand | English | 1999 | 51 | Occupational Safety and Health Service (OSHS) ([140]) |
| Chile | Spanish | 2009 | 40 | Instituto de Salud Publica de Chile (ISPCH) ([141]) |
| Spain | Spanish | - | 16 | Instituto Nacional de Seguridad, Salud y Bienestar en el Trabajo (INSHT) ([142]) |
For standard filter classes used in respirators, see Mechanical filter (respirator)#Filtration standards.
See also
[edit]- Cartridge (respirator) – Container that cleans pollution from air inhaled through it
- Dust mask – Pad held over the nose and mouth to protect against dust
- Face shield – Device used to protect the wearer's face from hazards
- Gas mask – Protection from inhaling airborne pollutants and toxic gases
- Open-source hardware – Hardware from the open-design movement
- Microparticle performance rating – used to measure an air filter's ability to capture small particles
- Minimum efficiency reporting value – Measurement scale for the effectiveness of air filters
- Personal protective equipment – Equipment designed to help protect an individual from hazards (PPE)
- Pocket mask – Device used to safely deliver first aid rescue breaths
- Self-contained breathing apparatus – Breathing gas supply system carried by the user
- Smoke hood – Device to protect the user from smoke inhalation in an emergency
- Surgical mask – Mouth and nose cover against bacterial aerosols
- Ventilator – Device that provides mechanical ventilation to the lungs
- Workplace respirator testing – Testing of respirators in real life conditions
References
[edit]- ^ (in Latin) – via Wikisource.
- ^ "Women in the US Military – History of Gas Masks". Chnm.gmu.edu. 11 September 2001. Archived from the original on 12 May 2011. Retrieved 18 April 2010.
- ^ Humboldt, Alexander von (1799). "Ueber die unterirdischen Gasarten und die Mittel ihren Nachtheil zu vermindern". WorldAtlas. Retrieved 27 March 2020.
- ^ David Zuck (1990). "Julius Jeffreys: Pioneer of humidification" (PDF). Proceedings of the History of Anaesthesia Society. 8b: 70–80. Archived (PDF) from the original on 4 November 2021. Retrieved 16 August 2020.
- ^ Christianson, Scott (2010). Fatal Airs: The Deadly History and Apocalyptic Future of Lethal Gases that Threaten Our World. ABC-CLIO. ISBN 9780313385520.
- ^ US patent 6529A, Lewis P. Haslett, "Lung Protector", published 1849-06-12, issued 1849-06-12 Archived 8 March 2021 at the Wayback Machine
- ^ [1], "Improvement in inhaler and respirator", issued 1879-08-26
- ^ Britain, Royal Institution of Great (1858). Notices of the Proceedings at the Meetings of the Members of the Royal Institution, with Abstracts of the Discourses. W. Nicol, Printer to the Royal Institution. p. 53.
- ^ Tyndall, John (1873). "On Some Recent Experiments with a Fireman's Respirator". Proceedings of the Royal Society of London. 22: 359–361. Bibcode:1873RSPS...22R.359T. ISSN 0370-1662. JSTOR 112853.
- ^ "Gas Mask Development (1926)". 67.225.133.110. Archived from the original on 27 February 2021. Retrieved 27 March 2020.
- ^ US patent 148868A, Samuel Barton, "Respirator", published 1874-03-24, issued 1874-03-24 Archived 8 March 2021 at the Wayback Machine
- ^ Lowry, H. C. (1947). "Some Landmarks in Surgical Technique". The Ulster Medical Journal. 16 (2): 102–113. PMC 2479244. PMID 18898288.
- ^ "The Chinese Doctor Who Beat the Plague". China Channel. 20 December 2018. Retrieved 10 March 2021.
- ^ "Obituary: WU LIEN-TEH, M.D., Sc.D., Litt.D., LL.D., M.P.H". Br Med J. 1 (5170): 429–430. 6 February 1960. doi:10.1136/bmj.1.5170.429-f. ISSN 0007-1447. PMC 1966655.
- ^ Flohr, Carsten (1996). "The Plague Fighter: Wu Lien-teh and the beginning of the Chinese public health system". Annals of Science. 53 (4): 361–380. doi:10.1080/00033799608560822. ISSN 0003-3790. PMID 11613294.
- ^ a b Lee, Kam Hing; Wong, Danny Tze-ken; Ho, Tak Ming; Ng, Kwan Hoong (2014). "Dr Wu Lien-teh: Modernising post-1911 China's public health service". Singapore Medical Journal. 55 (2): 99–102. doi:10.11622/smedj.2014025. PMC 4291938. PMID 24570319.
- ^ a b Ma, Zhongliang; Li, Yanli (2016). "Dr. Wu Lien Teh, plague fighter and father of the Chinese public health system". Protein & Cell. 7 (3): 157–158. doi:10.1007/s13238-015-0238-1. ISSN 1674-800X. PMC 4791421. PMID 26825808.
- ^ a b c Wilson, Mark (24 March 2020). "The untold origin story of the N95 mask". Fast Company. Retrieved 26 March 2020.
- ^ Wu Lien-te; World Health Organization (1926). A Treatise on Pneumonic Plague. Berger-Levrault.
- ^ Lynteris, Christos (18 August 2018). "Plague Masks: The Visual Emergence of Anti-Epidemic Personal Protection Equipment". Medical Anthropology. 37 (6): 442–457. doi:10.1080/01459740.2017.1423072. hdl:10023/16472. ISSN 0145-9740. PMID 30427733.
- ^ "First Usage of Poison Gas". National WWI Museum and Memorial. Retrieved 18 August 2024.
- ^ Wetherell & Mathers 2007, p. 157.
- ^ Victor Lefebure (1923). The Riddle of the Rhine: Chemical Strategy in Peace and War. The Chemical Foundation Inc. ISBN 0-585-23269-5.
- ^ "Macpherson Gas Hood . Accession #980.222". The Rooms Provincial Museum Archives (St. John's, NL). Retrieved 5 August 2017.
- ^ Mayer-Maguire & Baker 2015.
- ^ "Biographical entry Macpherson, Cluny (1879 - 1966)". livesonline.rcseng.ac.uk. Retrieved 22 April 2018.
- ^ "The UK". The Gas Mask Database. Archived from the original on 9 July 2008.
- ^ Howard W., Spencer. "The Historic and Cultural Importance of the HAWKS NEST TUNNEL DISASTER" (PDF). American Society of Safety Professionals.
- ^ a b Spelce, David; Rehak, Timothy R; Meltzer, Richard W; Johnson, James S (2019). "History of U.S. Respirator Approval (Continued) Particulate Respirators". J Int Soc Respir Prot. 36 (2): 37–55. PMC 7307331. PMID 32572305.
- ^ "Federal Coal Mine and Safety Act of 1969". US Department of Labor, US Mine Safety and Health Administration.
- ^ US EPA, OP (22 February 2013). "Summary of the Occupational Safety and Health Act". www.epa.gov. Retrieved 28 August 2021.
- ^ a b c NIOSH Guide to the Selection and Use of Particulate Respirators Certified Under 42 CFR 84. 1996.
- ^ "The untold origin story of the N95 mask". Fast Company and Mansueto Ventures, LLC. Archived from the original on 19 May 2020. Retrieved 9 April 2020.
- ^ Rees, Paula; Eisenbach, Larry (2020). "Ask Why: Sara Little Turnbull". Design Museum Foundation. Archived from the original on July 20, 2020. Retrieved April 1, 2020.
- ^ "DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service 42 CFR Part 84 RIN 0905–AB58 Respiratory Protective Devices" (PDF). US Federal Register. 8 June 1995. Retrieved 27 April 2024.
- ^ "42 CFR 84 Respiratory Protective Devices". NIOSH. 25 August 1995. Archived from the original on 30 December 1996.
- ^ Note: the following source cites July 1, 1998 as the end date for the transition period, contradicting official NIOSH publications. Herring Jr., Ronald N. (1997). "42 CFR Part 84: It's time to change respirators... but how?". Engineer's Digest. pp. 14–23.
- ^ "DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service 42 CFR Part 84" (PDF). US Federal Register. pp. 26850-26893. Retrieved 8 May 2024.
- ^ "CHANGES IN OCCUPATIONAL SAFETY REGS WILL PERMIT BETTER RESPIRATORS TO PROTECT AGAINST DUST AND DISEASE". NIOSH. 2 June 1995. Archived from the original on 31 December 1996.
- ^ Xie, John (19 March 2020). "World Depends on China for Face Masks But Can Country Deliver?". www.voanews.com. Voice of America. Archived from the original on 21 March 2020.
- ^ Dwyer, Colin (3 April 2020). "CDC Now Recommends Americans Consider Wearing Cloth Face Coverings In Public". NPR.
- ^ "Key Public Health Prevention Recommendations for HPAI A(H5N1)". United States CDC. 10 June 2024. Retrieved 15 June 2024.
- ^ "Protect Yourself From H5N1 When Working With Farm Animals" (PDF). United States CDC. Retrieved 15 June 2024.
- ^ Nix, Jessica; Griffin, Riley; Gale, Jason (8 May 2024). "Just One Human Is Infected by Bird Flu in the US. More Cases Are Likely". Bloomberg.
- ^ "Respirator use and practices". U.S. Bureau of Labour Statistics. Archived from the original on 17 October 2020. Retrieved 29 March 2020.
- ^ "Filtering out Confusion: Frequently Asked Questions about Respiratory Protection, User Seal Check (2018)" (PDF). NIOSH. Retrieved 8 December 2021.
- ^ a b "N95 Respirators and Surgical Masks (Face Masks)". U.S. Food and Drug Administration. March 11, 2020. Retrieved March 28, 2020.
- ^ Brosseau, Lisa; Ann, Roland Berry (October 14, 2009). "N95 Respirators and Surgical Masks". NIOSH Science Blog. Retrieved March 28, 2020.
- ^ Andrejko, Kristin L.; et al. (2022). "Effectiveness of Face Mask or Respirator Use in Indoor Public Settings for Prevention of SARS-CoV-2 Infection — California, February–December 2021". MMWR. Morbidity and Mortality Weekly Report. 71 (6): 212–216. doi:10.15585/mmwr.mm7106e1. PMC 8830622. PMID 35143470. Retrieved 30 January 2024.
- ^ "A Comparison of Surgical Masks, Surgical N95 Respirators, and Industrial N95 Respirators". Occupational Health & Safety. May 1, 2014. Retrieved April 7, 2020.
- ^ "Respirator Trusted-Source Information: Ancillary Respirator Information". U.S. National Institute for Occupational Safety and Health. January 26, 2018. Retrieved February 12, 2020.
- ^ "Surgical N95 vs. Standard N95 – Which to Consider?" (PDF). 3M Company. March 2020. Retrieved 12 June 2022.
- ^ "N95 Respirators, Surgical Masks, Face Masks, and Barrier Face Coverings". US Food and Drug Administration. 10 March 2023. Retrieved 27 April 2024.
- ^ Bach, Michael (July 6, 2017). "Understanding respiratory protection options in healthcare: the overlooked elastomeric". NIOSH Science Blog. Retrieved April 21, 2020.
- ^ 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings (PDF). U.S. Centers for Disease Control and Prevention. July 2019. pp. 55–56. Retrieved February 9, 2020.
- ^ Bollinger, Nancy (1 October 2004). "NIOSH respirator selection logic". U.S. National Institute for Occupational Safety and Health: 5–16. doi:10.26616/NIOSHPUB2005100. Archived from the original on 15 July 2020. Retrieved 20 April 2020.
- ^ Metzler, R; Szalajda, J (2011). "NIOSH Fact Sheet: NIOSH Approval Labels - Key Information to Protect Yourself" (PDF). DHHS (NIOSH) Publication No. 2011-179. ISSN 0343-6993. Archived (PDF) from the original on 20 July 2018. Retrieved 10 September 2017.
- ^ "A Guide to Respiratory Protective Equipment" (PDF). hsa.ie. Archived (PDF) from the original on 30 June 2024. Retrieved 12 July 2024.
- ^ "Technical Bulletin: Comparison of FFP2, KN95, and N95 and Other Filtering Facepiece Respirator Classes" (PDF). 3M Personal Safety Division. January 2020. Archived (PDF) from the original on 14 April 2020. Retrieved 3 April 2020.
- ^ The document describes the methods used previously and currently used to perform the timely replacement of cartridges in air purifying respirators.
- ^ OSHA standard 29 CFR 1910.134 Archived 24 September 2014 at the Wayback Machine "Respiratory Protection"
- ^ Bollinger, Nancy; et al. (2004). NIOSH Respirator Selection Logic. DHHS (NIOSH) Publication No. 2005-100. Cincinnati, Ohio: National Institute for Occupational Safety and Health. p. 32. doi:10.26616/NIOSHPUB2005100. Archived from the original on 23 June 2017. Retrieved 10 September 2017.
- ^ "STANDARD APPLICATION PROCEDURES FOR THE CERTIFICATION OF RESPIRATORS" (PDF). NIOSH. January 2001. Archived from the original (PDF) on 19 March 2003.
- ^ "Respirator Trusted-Source Information: What are they?". U.S. National Institute for Occupational Safety and Health. 29 January 2018. Archived from the original on 28 March 2020. Retrieved 27 March 2020.
- ^ "Filtering out Confusion: Frequently Asked Questions about Respiratory Protection" (PDF). NIOSH. 2018. doi:10.26616/NIOSHPUB2018128. Archived (PDF) from the original on 9 April 2023. Retrieved 29 May 2024.
- ^ "PPE Image Gallery: Respiratory Protective Equipment - Civilian - Radiation Emergency Medical Management". www.remm.nlm.gov.
- ^ "Elastomeric Respirators: Strategies During Conventional and Surge Demand Situations". U.S. Centers for Disease Control and Prevention. 11 February 2020. Archived from the original on 11 February 2023.
- ^ a b c Bach, Michael (6 July 2017). "Understanding respiratory protection options in Healthcare: The Overlooked Elastomeric". NIOSH Science Blog. CDC.
- ^ "Respirator Trusted-Source Information: What are they?". U.S. National Institute for Occupational Safety and Health. 29 January 2018. Retrieved 27 March 2020.
- ^ a b Liverman CT, Yost OC, Rogers BM, et al., eds. (6 December 2018). "Elastomeric Respirators". Reusable Elastomeric Respirators in Health Care: Considerations for Routine and Surge Use. National Academies Press.
- ^ "Respirator Selection: Air-purifying vs. Atmosphere-supplying Respirators". U.S. Occupational Safety and Health Administration. Archived from the original on 17 April 2020. Retrieved 9 April 2020.
- ^ Bollinger 1987, p. 184
- ^ IFSTA 2008, p. 190.
- ^ IFSTA 2008, p. 191.
- ^ a b Bollinger 1987, pp. 7–8
- ^ "Respirator Selection: Air-purifying vs. Atmosphere-supplying Respirators". U.S. Occupational Safety and Health Administration. Retrieved 9 April 2020.
- ^ "PPE Image Gallery: Respiratory Protective Equipment - Civilian - Radiation Emergency Medical Management". www.remm.nlm.gov.
- ^ ASTM E2952 (2023 ed.). West Conshohocken, PA: ASTM International (published June 2023). 1 May 2023.
{{cite book}}: CS1 maint: date and year (link) - ^ New Scientist. 24–31 December 1987.
- ^ April 2014, 10th. "Government Procurement April/May". American City and County. Archived from the original on 1 May 2011. Retrieved 15 August 2020.
{{cite web}}: CS1 maint: numeric names: authors list (link) - ^ "Fire Preparedness - Smoke Masks and Fire Hoods Can Save Lives". Every Life Secure!. Archived from the original on 18 September 2018. Retrieved 15 August 2020.
- ^ Bland, Karina. "10-year-old Julio is teaching his family about Black History Month". The Arizona Republic. Retrieved 1 August 2020.
- ^ Brewer, Mary Jane; Clevel, Special to; .com (12 February 2020). "Curator speaks about Medina's Little Wiz Fire Museum". cleveland. Archived from the original on 21 February 2020. Retrieved 29 July 2020.
- ^ Bollinger 1987, p. 207
- ^ Bollinger 1987, p. 65
- ^ Bollinger 1987, pp. 59–64
- ^ Bollinger, Nancy J. (1987). "NIOSH Guide to Industrial Respiratory Protection".
- ^ "The State of the National Initiative on Prevention through Design" (PDF). NIOSH. May 2014. Archived (PDF) from the original on 3 June 2024. Retrieved 3 June 2024.
- ^ a b "MAJOR REQUIREMENTS OF OSHA'S RESPIRATORY PROTECTION STANDARD 29 CFR 1910.134" (PDF). United States Department of Labor, OSHA. Archived (PDF) from the original on 27 January 2024. Retrieved 3 June 2024.
- ^ "Summary of Key MSHA Requirements for a Respiratory Protection Program" (PDF). Archived (PDF) from the original on 16 June 2024. Retrieved 3 June 2024.
- ^ "RE: Lowering Miners' Exposure to Respirable Crystalline Silica and Improving Respiratory Protection (RIN 1219-AB36)" (PDF). 11 September 2023.
- ^ "MSHA's proposed rule on silica has 'shortcomings,' lawmakers say". 21 September 2023. Archived from the original on 5 June 2024. Retrieved 3 June 2024.
- ^ a b "Counterfeit Respirators / Misrepresentation of NIOSH Approval". NIOSH. 23 May 2024.
- ^ Fukakusa, J.; Rosenblat, J.; Jang, B.; Ribeiro, M.; Kudla, I.; Tarlo, S. M. (2011). "Factors influencing respirator use at work in respiratory patients". Occupational Medicine. 61 (8): 576–582. doi:10.1093/occmed/kqr132. PMID 21968940.
- ^ Biering, Karin; Kinnerup, Martin; Cramer, Christine; Dalbøge, Annett; Toft Würtz, Else; Lund Würtz, Anne Mette; Kolstad, Henrik Albert; Schlünssen, Vivi; Meulengracht Flachs, Esben; Nielsen, Kent J. (2024). "Use, failure, and non-compliance of respiratory personal protective equipment and risk of upper respiratory tract infections—A longitudinal repeated measurement study during the COVID-19 pandemic among healthcare workers in Denmark". Annals of Work Exposures and Health. pp. 376–386. doi:10.1093/annweh/wxae008. PMID 38373246.
- ^ Baig, Aliya S.; Knapp, Caprice; Eagan, Aaron E.; Radonovich, Lewis J. (2010). "Health care workers' views about respirator use and features that should be included in the next generation of respirators". American Journal of Infection Control. 38 (1): 18–25. doi:10.1016/j.ajic.2009.09.005. PMC 7132692. PMID 20036443.
- ^ "The Hierarchy of Controls, Part Four: Personal Protective Equipment". Simplified Safety. Archived from the original on 3 June 2024. Retrieved 3 June 2024.
- ^ "Personal Protective Equipment (PPE): Protect the Worker with PPE". NIOSH. 5 May 2023. Archived from the original on 3 June 2024. Retrieved 3 June 2024.
- ^ U.S. Department of Labor, Bureau of Labor Statistics. Respirator Usage in Private Sector Firms, 2001 (PDF). Morgantown, WV: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health. p. 273. Archived (PDF) from the original on 1 November 2017. Retrieved 22 January 2019.
- ^ Letavet A.A. [in Russian] (1973). Институт гигиены труда и профессиональных заболеваний в составе АМН СССР [Research Institute of industrial hygiene and occupational diseases of AMS USSR]. Occupational medicine and industrial ecology [Гигиена труда и профессиональные заболевания] (in Russian) (9): 1–7. ISSN 1026-9428. Archived from the original on 23 January 2019. Retrieved 22 January 2019.
- ^ M. Nicas & R. Spear (1992). "A Probability Model for Assessing Exposure among Respirator Wearers: Part II - Overexposure to Chronic versus Acute Toxicants". American Industrial Hygiene Association Journal. 53 (7): 419–426. doi:10.1080/15298669291359889. PMID 1496932. Archived from the original on 7 April 2023. Retrieved 22 January 2018.
- ^ "To Beard or not to Beard? That's a good Question!". NIOSH. 2 November 2017. Archived from the original on 18 March 2020. Retrieved 27 February 2020.
- ^ "Transcript for the OSHA Training Video Entitled Counterfeit & Altered Respirators: The Importance of Checking for NIOSH Certification". US Department of Labor, OSHA. January 2012. Archived from the original on 3 June 2024. Retrieved 3 June 2024.
- ^ Zhuang, Ziqing; Bergman, Michael; Krah, Jaclyn (5 January 2016). "New NIOSH Study Supports the OSHA Annual Fit Testing Requirements for Filtering Facepiece Respirators". NIOSH.
- ^ Edwin C. Hyatt (1984). "Respirators: How well do they really protect?". Journal of the International Society for Respiratory Protection. 2 (1): 6–19. ISSN 0892-6298. Archived from the original on 22 October 2016. Retrieved 22 January 2018.
- ^ Mean values for several models. For example, IDLH for CO2 = 4% Archived 20 April 2018 at the Wayback Machine, but filtering facepiese "AOSafety Pleats Plus" provided concentration up to 5.8%. According to the paper the model was discontinued from manufacturing and had its NIOSH approval withdrawn. (It is also no longer on the CEL, TC-84A-2630 and TC-84A-4320. Former approval by the FDA Archived 17 February 2017 at the Wayback Machine, while other discontinued models are still on the CEL Archived 14 July 2016 at the Wayback Machine) Source: E.J. Sinkule, J.B. Powell, F.L. Goss (2013). "Evaluation of N95 respirator use with a surgical mask cover: effects on breathing resistance and inhaled carbon dioxide". Annals of Occupational Hygiene. 57 (3). Oxford University Press: 384–398. doi:10.1093/annhyg/mes068. ISSN 2398-7308. PMID 23108786.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ R.J. Roberge, A. Coca, W.J. Williams, J.B. Powell & A.J. Palmiero (2010). "Physiological Impact of the N95 Filtering Facepiece Respirator on Healthcare Workers". Respiratory Care. 55 (5). American Association for Respiratory Care (AARC): 569–577. ISSN 0020-1324. PMID 20420727. Archived from the original on 31 October 2020. Retrieved 28 February 2021.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Carmen L. Smith, Jane L. Whitelaw & Brian Davies (2013). "Carbon dioxide rebreathing in respiratory protective devices: influence of speech and work rate in full-face masks". Ergonomics. 56 (5). Taylor & Francis: 781–790. doi:10.1080/00140139.2013.777128. ISSN 0014-0139. PMID 23514282. S2CID 40238982. Archived from the original on 1 November 2020. Retrieved 28 February 2021.
- ^ Rhee, Michelle S. M.; Lindquist, Carin D.; Silvestrini, Matthew T.; Chan, Amanda C.; Ong, Jonathan J. Y.; Sharma, Vijay K. (2021). "Carbon dioxide increases with face masks but remains below short-term NIOSH limits". BMC Infectious Diseases. 21 (1): 354. doi:10.1186/s12879-021-06056-0. PMC 8049746. PMID 33858372.
- ^ Ong, Jonathan J. Y.; Chan, Amanda C. Y.; Bharatendu, Chandra; Teoh, Hock Luen; Chan, Yee Cheun; Sharma, Vijay K. (2021). "Headache Related to PPE Use during the COVID-19 Pandemic". Current Pain and Headache Reports. 25 (8): 53. doi:10.1007/s11916-021-00968-x. PMC 8203491. PMID 34129112.
- ^ Chris C.I. Foo, Anthony T.J. Goon, Yung-Hian Leow, Chee-Leok Goh (2006). "Adverse skin reactions to personal protective equipment against severe acute respiratory syndrome – a descriptive study in Singapore". Contact Dermatitis. 55 (5). John Wiley & Sons: 291–294. doi:10.1111/j.1600-0536.2006.00953.x. ISSN 0105-1873. PMC 7162267. PMID 17026695.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Determination of Sample Size and Passing Criteria for Fit Test Panels" (PDF). Archived (PDF) from the original on 8 August 2023. Retrieved 3 June 2024.
- ^ Zhuang, Ziqing; Bradtmiller, Bruce; Shaffer, Ronald E. (2007). "New Respirator Fit Test Panels Representing the Current U.S. Civilian Work Force". Journal of Occupational and Environmental Hygiene. 4 (9): 647–659. doi:10.1080/15459620701497538. PMID 17613722.
- ^ §135, §198, and §205. "PART 84—APPROVAL OF RESPIRATORY PROTECTIVE DEVICES". Archived from the original on 15 March 2024. Retrieved 3 June 2024.
- ^ "国家标准|Gb 2626-2019". Archived from the original on 3 June 2024. Retrieved 3 June 2024.
- ^ "Protection levels: FFP1 masks, FFP2 masks, FFP3 masks". Moldex Europe. Archived from the original on 2 June 2024. Retrieved 3 June 2024.
- ^ "DEPARTMENT OF HEALTH AND HUMAN SERVICES Centers for Disease Control and Prevention Guidelines for Preventing the Transmission of Mycobacterium Tuberculosis in Health-Care Facilities, 1994" (PDF). US Federal Register. Archived (PDF) from the original on 8 June 2024. Retrieved 8 May 2024.
- ^ Nancy J. Bollinger, Robert H. Schutz; et al. (1987). NIOSH Guide to Industrial Respiratory Protection. DHHS (NIOSH) Publication No 87-116. Cincinnati, Ohio: National Institute for Occupational Safety and Health. p. 305. doi:10.26616/NIOSHPUB87116. Archived from the original on 23 November 2017. Retrieved 10 June 2018.
- ^ Nancy Bollinger; et al. (2004). NIOSH Respirator Selection Logic. DHHS (NIOSH) Publication No 2005-100. Cincinnati, Ohio: National Institute for Occupational Safety and Health. p. 32. doi:10.26616/NIOSHPUB2005100. Archived from the original on 23 June 2017. Retrieved 10 June 2018.
- ^ Linda Rosenstock; et al. (1999). TB Respiratory Protection Program In Health Care Facilities - Administrator's Guide. DHHS (NIOSH) Publication No 99-143. Cincinnati, Ohio: National Institute for Occupational Safety and Health. p. 120. doi:10.26616/NIOSHPUB99143. Archived from the original on 2 April 2020. Retrieved 10 June 2018.
- ^ Kathleen Kincade, Garnet Cooke, Kaci Buhl; et al. (2017). Janet Fults (ed.). Respiratory Protection Guide. Requirements for Employers of Pesticide Handlers. Worker Protection Standard (WPS). California: Pesticide Educational Resources Collaborative (PERC). p. 48. Archived from the original on 22 March 2021. Retrieved 10 June 2018.
{{cite book}}: CS1 maint: multiple names: authors list (link) PDF Archived 8 June 2018 at the Wayback Machine Wiki - ^ Occupational Safety and Health Administration (1998). "Respiratory Protection eTool". OSHA (in English and Spanish). Washington, DC. Archived from the original on 22 March 2021. Retrieved 10 June 2018.
- ^ Hilda L. Solis; et al. (2011). Small Entity Compliance Guide for the Respiratory Protection Standard. OSHA 3384-09. Washington, DC: Occupational Safety and Health Administration, U.S. Department of Labor. p. 124. Archived from the original on 22 March 2021. Retrieved 10 June 2018. PDF Archived 28 April 2018 at the Wayback Machine Wiki
- ^ OSHA; et al. (2015). Hospital Respiratory Protection Program Toolkit. OSHA 3767. Resources for Respirator Program Administrators. Washington, DC: Occupational Safety and Health Administration, U.S. Department of Labor. p. 96. Archived from the original on 22 March 2021. Retrieved 10 June 2018. PDF Archived 28 April 2018 at the Wayback Machine Wiki
- ^ J. Edgar Geddie (2012). A Guide to Respiratory Protection. Industry Guide 44 (2 ed.). Raleigh, North Carolina: Occupational Safety and Health Division, N.C. Department of Labor. p. 54. Archived from the original on 22 March 2021. Retrieved 10 June 2018.
- ^ Patricia Young, Phillip Fehrenbacher & Mark Peterson (2014). Breathe Right! Oregon OSHA's guide to developing a respiratory protection program for small-business owners and managers. Publications: Guides 440-3330. Salem, Oregon: Oregon OSHA Standards and Technical Resources Section, Oregon Occupational Safety and Health. p. 44. Archived from the original on 22 March 2021. Retrieved 10 June 2018. PDF Archived 13 July 2019 at the Wayback Machine Wiki
- ^ Patricia Young & Mark Peterson (2016). Air you breathe: Oregon OSHA's respiratory protection guide for agricultural employers. Publications: Guides 440-3654. Salem, Oregon: Oregon OSHA Standards and Technical Resources Section, Oregon Occupational Safety and Health. p. 32. Archived from the original on 22 March 2021. Retrieved 10 June 2018.
- ^ Oregon OSHA (2014). "Section VIII / Chapter 2: Respiratory Protection". Oregon OSHA Technical Manual. Rules. Salem, Oregon: Oregon OSHA. p. 38. Archived from the original on 22 March 2021. Retrieved 10 June 2018. PDF Archived 8 May 2018 at the Wayback Machine Wiki
- ^ Cal/OSHA Consultation Service, Research and Education Unit, Division of Occupational Safety and Health, California Department of Industrial Relations (2017). Respiratory Protection in the Workplace. A Practical Guide for Small-Business Employers (3 ed.). Santa Ana, California: California Department of Industrial Relations. p. 51. Archived from the original on 22 March 2021. Retrieved 10 June 2018.
{{cite book}}: CS1 maint: multiple names: authors list (link) PDF Archived 19 December 2017 at the Wayback Machine - ^ K. Paul Steinmeyer; et al. (2001). Manual of Respiratory Protection Against Airborne Radioactive Material. NUREG/CR-0041, Revision 1. Washington, DC: Office of Nuclear Reactor Regulation, U.S. Nuclear Regulatory Commission. p. 166. Archived from the original on 22 March 2021. Retrieved 10 June 2018. PDF Archived 12 June 2018 at the Wayback Machine Wiki
- ^ Gary P. Noonan, Herbert L. Linn, Laurence D. Reed; et al. (1986). Susan V. Vogt (ed.). A guide to respiratory protection for the asbestos abatement industry. NIOSH IA 85-06; EPA DW 75932235-01-1. Washington, DC: Environmental Protection Agency (EPA) & National Institute for Occupational Safety and Health (NIOSH). p. 173. Archived from the original on 22 March 2021. Retrieved 10 June 2018.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Jaime Lara, Mireille Vennes (2002). Guide pratique de protection respiratoire. Projet de recherche: 0098-0660 (in French) (1 ed.). Montreal, Quebec (Canada): Institut de recherche Robert-Sauve en sante et en securite du travail (IRSST), Commission de la sante et de la securite du travail du Quebec. p. 56. ISBN 978-2-550-37465-7. Archived from the original on 12 June 2018. Retrieved 10 June 2018.; 2 edition: Jaime Lara, Mireille Vennes (26 August 2013). Guide pratique de protection respiratoire. DC 200-1635 2CORR (in French) (2 ed.). Montreal, Quebec (Canada): Institut de recherche Robert-Sauve en sante et en securite du travail (IRSST), Commission de la santé et de la sécurité du travail du Québec. p. 60. ISBN 978-2-550-40403-3. Archived from the original on 22 August 2019. Retrieved 10 June 2018.; online version: Jaime Lara, Mireille Vennes (2016). "Appareils de protection respiratoire". www.cnesst.gouv.qc.ca (in French). Quebec (Quebec, Canada): Commission des normes, de l'equite, de la sante et de la securite du travail. Archived from the original on 22 March 2021. Retrieved 10 June 2018.
- ^ Jacques Lavoie, Maximilien Debia, Eve Neesham-Grenon, Genevieve Marchand, Yves Cloutier (22 May 2015). "A support tool for choosing respiratory protection against bioaerosols". www.irsst.qc.ca. Montreal, Quebec (Canada): Institut de recherche Robert-Sauve en sante et en securite du travail (IRSST). Archived from the original on 7 May 2021. Retrieved 10 June 2018.
{{cite web}}: CS1 maint: multiple names: authors list (link) Publication no.: UT-024; Research Project: 0099-9230. - ^ Jacques Lavoie, Maximilien Debia, Eve Neesham-Grenon, Genevieve Marchand, Yves Cloutier (22 May 2015). "Un outil d'aide a la prise de decision pour choisir une protection respiratoire contre les bioaerosols". www.irsst.qc.ca (in French). Montreal, Quebec (Canada): Institut de recherche Robert-Sauve en sante et en securite du travail (IRSST). Archived from the original on 7 May 2021. Retrieved 10 June 2018.
{{cite web}}: CS1 maint: multiple names: authors list (link) N° de publication : UT-024; Projet de recherche: 0099-9230. - ^ M. Gumon (2017). Les appareils de protection respiratoire. Choix et utilisation. ED 6106 (in French) (2 ed.). Paris: Institut National de Recherche et de Securite (INRS). p. 68. ISBN 978-2-7389-2303-5. Archived from the original on 7 May 2021. Retrieved 10 June 2018.
- ^ Spitzenverband der gewerblichen Berufsgenossenschaften und der Unfallversicherungsträger der öffentlichen Hand (DGUV) (2011). BGR/GUV-R 190. Benutzung von Atemschutzgeräten (in German). Berlin: Deutsche Gesetzliche Unfallversicherung e.V. (DGUV), Medienproduktion. p. 174. Archived from the original on 7 May 2021. Retrieved 10 June 2018. PDF Archived 10 August 2015 at the Wayback Machine
- ^ The Health and Safety Executive (2013). Respiratory protective equipment at work. A practical guide. HSG53 (4 ed.). Crown. p. 59. ISBN 978-0-71766-454-2. Archived from the original on 9 August 2015. Retrieved 10 June 2018.
- ^ The UK Nuclear Industry Radiological Protection Coordination Group (2016). Respiratory Protective Equipment (PDF). Good Practice Guide. London (UK): IRPCG. p. 29. Archived (PDF) from the original on 7 May 2021. Retrieved 10 June 2018.
- ^ The Health and Safety Authority (2010). A Guide to Respiratory Protective Equipment. HSA0362. Dublin (Ireland): HSA. p. 19. ISBN 978-1-84496-144-3. Archived from the original on 7 May 2021. Retrieved 10 June 2018. PDF Archived 19 June 2018 at the Wayback Machine
- ^ Occupational Safety and Health Service (1999). A guide to respiratory protection (8 ed.). Wellington (New Zealand): NZ Department of Labour. p. 51. ISBN 978-0-477-03625-2. Archived from the original on 12 June 2018. Retrieved 10 June 2018. PDF Archived 29 January 2018 at the Wayback Machine
- ^ Christian Albornoz, Hugo Cataldo (2009). Guia para la seleccion y control de proteccion respiratoria. Guia tecnica (in Spanish). Santiago (Chile): Departamento de salud occupational, Instituto de Salud Publica de Chile. p. 40. Archived from the original on 22 August 2019. Retrieved 10 June 2018. PDF Archived 28 May 2016 at the Wayback Machine
- ^ Instituto Nacional de Seguridad, Salud y Bienestar en el Trabajo (INSSBT). Guia orientativa para la seleccion y utilizacion de protectores respiratorios. Documentos tecnicos INSHT (in Spanish). Madrid: Instituto Nacional de Seguridad, Salud y Bienestar en el Trabajo (INSHT). p. 16. Archived from the original on 24 April 2019. Retrieved 10 June 2018. PDF Archived 22 December 2018 at the Wayback Machine
Further reading
[edit]- A Sideline Mushroomed - Summary of LANL involvement in respirators
- Cheremisinoff, Nicholas (1999). Handbook of Industrial Toxicology and Hazardous Materials. Marcel Dekker. ISBN 978-0-8247-1935-7.
- NIOSH respirators main page
- NIOSH respirator fact sheet
- What's Special about Chemical, Biological, Radiological, and Nuclear (CBRN) Air-Purifying Respirators (APR)? NIOSH Fact Sheet
- NIOSH-Approved Disposable Particulate Respirators (Filtering Facepieces)
- TSI Application note ITI-041: Mechanisms of Filtration for High Efficiency Fibrous Filters Archived 29 August 2017 at the Wayback Machine
- British Standard BS EN 143:2000: Respiratory protective devices – Particle filters – Requirements, testing, marking
- British Standard BS EN 149:2001: Respiratory protective devices – Filtering half masks to protect against particles – Requirements, testing, marking
External links
[edit]- Mine Safety Appliance Company (MSA) Respirator Classification Guide MSA.com
- CDC Protective Masks Fact Sheet cdc.gov/niosh
- OSHA videos on respiratory protection Archived 4 February 2012 at the Wayback Machine osha.gov
- Occupational Safety & Health Administration, Respiratory Protection Training Video on respiratory protection

