Addison's disease
| Addison's disease | |
|---|---|
| Other names | Addison disease, primary adrenal insufficiency,[1] primary adrenocortical insufficiency, chronic adrenal insufficiency, chronic adrenocortical insufficiency, primary hypocorticalism, primary hypocortisolism, primary hypoadrenocorticism, primary hypocorticism, primary hypoadrenalism |
 | |
| Darkening of the skin seen on the legs of an otherwise fair-skinned patient | |
| Specialty | Endocrinology |
| Symptoms | Abdominal pain, weakness, weight loss, darkening of the skin[1] |
| Complications | Adrenal crisis[1] |
| Usual onset | Middle-aged females[1] |
| Causes | Problems with the adrenal gland[1] |
| Diagnostic method | Blood tests, urine tests, medical imaging[1] |
| Treatment | Synthetic corticosteroid such as hydrocortisone and fludrocortisone[1][2] |
| Frequency | 0.9–1.4 per 10,000 people (developed world)[1][3] |
| Deaths | Doubles risk of death |
| Named after | Thomas Addison |
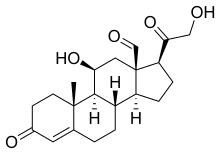
Addison's disease, also known as primary adrenal insufficiency,[4] is a rare long-term endocrine disorder characterized by inadequate production of the steroid hormones cortisol and aldosterone by the two outer layers of the cells of the adrenal glands (adrenal cortex), causing adrenal insufficiency.[5][6] Symptoms generally come on slowly and insidiously and may include abdominal pain and gastrointestinal abnormalities, weakness, and weight loss.[1] Darkening of the skin in certain areas may also occur.[1] Under certain circumstances, an adrenal crisis may occur with low blood pressure, vomiting, lower back pain, and loss of consciousness.[1] Mood changes may also occur. Rapid onset of symptoms indicates acute adrenal failure, which is a clinical emergency.[5] An adrenal crisis can be triggered by stress, such as from an injury, surgery, or infection.[1]
Addison's disease arises when the adrenal gland does not produce sufficient amounts of the steroid hormones cortisol and (sometimes) aldosterone.[1] It is an autoimmune disease which affects some genetically predisposed people in whom the body's own immune system has started to target the adrenal glands.[7] In many adult cases it is unclear what has triggered the onset of this disease, though it sometimes follows tuberculosis.[7] Causes can include certain medications, sepsis, and bleeding into both adrenal glands.[1][8] Addison's disease is generally diagnosed by blood tests, urine tests, and medical imaging.[1]
Treatment involves replacing the absent or low hormones.[1] This involves taking a synthetic corticosteroid, such as hydrocortisone or fludrocortisone.[1][2] These medications are typically taken orally.[1] Lifelong, continuous steroid replacement therapy is required, with regular follow-up treatment and monitoring for other health problems which may occur.[9] A high-salt diet may also be useful in some people.[1] If symptoms worsen, an injection of corticosteroid is recommended (people need to carry a dose with them at all times).[1] Often, large amounts of intravenous fluids with the sugar dextrose are also required.[1] With appropriate treatment, the overall outcome is generally favorable,[10] and most people are able to lead a reasonably normal life.[11] Without treatment, an adrenal crisis can result in death.[1]
Addison's disease affects about 9 to 14 per 100,000 people in the developed world.[1][3] It occurs most frequently in middle-aged females.[1] The disease is named after Thomas Addison, a graduate of the University of Edinburgh Medical School, who first described the condition in 1855.[12][13]
Signs and symptoms
[edit]
The symptoms of Addison's disease can develop over several months and resemble other medical conditions.[14] Most common symptoms are caused by low levels of hormones that would normally be produced by the adrenal glands. Low blood cortisol can cause a variety of symptoms, including fatigue, malaise, muscle and joint pain, reduced appetite, weight loss, and increased sensitivity to cold.[15][14] Gastrointestinal symptoms such as nausea, abdominal pain, and vomiting are particularly common.[16][14] Low aldosterone can cause affected people to crave salty foods, as well as develop low blood pressure that leads to dizziness upon standing.[16] In women, low dehydroepiandrosterone (DHEA) can result in dry and itchy skin, loss of armpit and pubic hair, and reduced sexual drive.[15] Young children with Addison's disease may have insufficient weight gain and recurrent infections.[15] Low cortisol also interferes with adrenocorticotropic hormone (ACTH) regulation, sometimes resulting in the darkening of the skin and mucous membranes, particularly in areas exposed to sun or regular friction.[14]
Blood tests in people with Addison's disease often reveal low blood sodium. Many also have high blood potassium and/or high thyroid-stimulating hormone (TSH).[14]
Most people with Addison's disease develop or have a preexisting autoimmune disease.[15] Particularly common comorbid conditions are autoimmune thyroid disease (40% of people with Addison's), premature ovarian failure (up to 16% of people with Addison's), type 1 diabetes (11%), pernicious anemia (10%), vitiligo (6%) and celiac disease (2%).[15] The combination of Addison's disease in addition to mucocutaneous candidiasis, hypoparathyroidism, or both, is called autoimmune polyendocrine syndrome type 1.[17] The presence of Addison's in addition to autoimmune thyroid disease, type 1 diabetes, or both, is called autoimmune polyendocrine syndrome type 2.[18]
Adrenal crisis
[edit]An "adrenal crisis" or "Addisonian crisis" is a constellation of symptoms that indicates severe adrenal insufficiency. This may be the result of either previously undiagnosed Addison's disease, a disease process suddenly affecting adrenal function (such as adrenal hemorrhage), or an intercurrent problem (e.g., infection, trauma) in someone known to have Addison's disease. It is a medical emergency and potentially life-threatening situation requiring immediate emergency treatment.[19]
Characteristic symptoms are:[20]
- Sudden penetrating pain in the legs, lower back, or abdomen
- Severe vomiting and diarrhea, resulting in dehydration
- Low blood pressure
- Syncope (loss of consciousness and ability to stand)
- Hypoglycemia (reduced level of blood glucose)
- Confusion, psychosis, slurred speech
- Severe lethargy
- Hyponatremia (low sodium level in the blood)
- Hyperkalemia (elevated potassium level in the blood)
- Hypercalcemia (elevated calcium level in the blood)
- Convulsions
- Fever
Causes
[edit]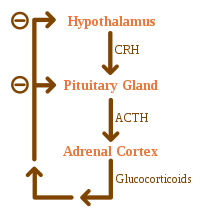
Causes of adrenal insufficiency can be categorized by the mechanism through which they cause the adrenal glands to produce insufficient cortisol. This can be due to damage or destruction of the adrenal cortex. These deficiencies include glucocorticoid and mineralocorticoid hormones as well. These are adrenal dysgenesis (the gland has not formed adequately during development), impaired steroidogenesis (the gland is present but is biochemically unable to produce cortisol), or adrenal destruction (disease processes leading to glandular damage).[12]
Darkening (hyperpigmentation) of the skin, including areas not exposed to the sun – characteristic sites of darkening are skin creases (e.g., of the hands), nipple, and the inside of the cheek (buccal mucosa); also, old scars may darken. This occurs because melanocyte-stimulating hormone (MSH) and ACTH share the same precursor molecule, pro-opiomelanocortin (POMC). After production in the anterior pituitary gland, POMC gets cleaved into gamma-MSH, ACTH, and beta-lipotropin. The subunit ACTH undergoes further cleavage to produce alpha-MSH, the most important MSH for skin pigmentation. In secondary and tertiary forms of adrenal insufficiency, skin darkening does not occur, as ACTH is not overproduced.
Adrenal destruction
[edit]Autoimmune adrenalitis is the most common cause of Addison's disease in the industrialized world as it represents between 68% and 94% of cases.[6][21][22] Autoimmune destruction of the adrenal cortex is caused by an immune reaction against the enzyme 21-hydroxylase (a phenomenon first described in 1992).[23] This may be isolated or in the context of autoimmune polyendocrine syndrome (APS type 1 or 2), in which other hormone-producing organs, such as the thyroid and pancreas, may also be affected.[24]
Adrenal destruction is also a feature of adrenoleukodystrophy, and when the adrenal glands are involved in metastasis (seeding of cancer cells from elsewhere in the body, especially lung), hemorrhage (e.g., in Waterhouse–Friderichsen syndrome or antiphospholipid syndrome), particular infections (tuberculosis, histoplasmosis, coccidioidomycosis), or the deposition of abnormal protein in amyloidosis.[25]
Adrenal dysgenesis
[edit]All causes in this category are genetic, and generally very rare. These include mutations to the SF1 transcription factor, congenital adrenal hypoplasia due to DAX-1 gene mutations and mutations to the ACTH receptor gene (or related genes, such as in the Triple-A or Allgrove syndrome). DAX-1 mutations may cluster in a syndrome with glycerol kinase deficiency with a number of other symptoms when DAX-1 is deleted together with a number of other genes.[12]
Impaired steroidogenesis
[edit]To form cortisol, the adrenal gland requires cholesterol, which is then converted biochemically into steroid hormones. Interruptions in the delivery of cholesterol include Smith–Lemli–Opitz syndrome and abetalipoproteinemia. Of the synthesis problems, congenital adrenal hyperplasia is the most common (in various forms: 21-hydroxylase, 17α-hydroxylase, 11β-hydroxylase and 3β-hydroxysteroid dehydrogenase), lipoid CAH due to deficiency of StAR and mitochondrial DNA mutations.[12] Some medications interfere with steroid synthesis enzymes (e.g., ketoconazole), while others accelerate the normal breakdown of hormones by the liver (e.g., rifampicin, phenytoin).[12]
Diagnosis
[edit]Suggestive features
[edit]Routine laboratory investigations may show:[12]
- Low blood sugar (worse in children due to loss of glucocorticoid's glucogenic effects)
- Low blood sodium, due to loss of production of the hormone aldosterone, to the kidney's inability to excrete free water in the absence of sufficient cortisol, and also the effect of corticotropin-releasing hormone to stimulate secretion of ADH.
- High blood potassium, due to loss of production of the hormone aldosterone.
- Eosinophilia and lymphocytosis (increased number of eosinophils or lymphocytes, two types of white blood cells)
- Metabolic acidosis (increased blood acidity), also is due to loss of the hormone aldosterone because sodium reabsorption in the distal tubule is linked with acid/hydrogen ion (H+) secretion. Absent or insufficient levels of aldosterone stimulation of the renal distal tubule lead to sodium wasting in the urine and H+ retention in the serum.
Testing
[edit]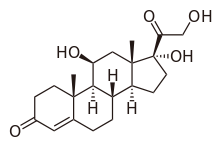
In suspected cases of Addison's disease, demonstration of low adrenal hormone levels even after appropriate stimulation (called the ACTH stimulation test or synacthen test) with synthetic pituitary ACTH hormone tetracosactide is needed for the diagnosis. Two tests are performed, the short and the long test. Dexamethasone does not cross-react with the assay and can be administered concomitantly during testing.[26][27]
The short test compares blood cortisol levels before and after 250 micrograms of tetracosactide (intramuscular or intravenous) is given. If one hour later, plasma cortisol exceeds 170 nmol/L and has risen by at least 330 nmol/L to at least 690 nmol/L, adrenal failure is excluded. If the short test is abnormal, the long test is used to differentiate between primary adrenal insufficiency and secondary adrenocortical insufficiency.[28]
The long test uses 1 mg tetracosactide (intramuscular). Blood is taken 1, 4, 8, and 24 hours later. Normal plasma cortisol level should reach 1,000 nmol/L by 4 hours. In primary Addison's disease, the cortisol level is reduced at all stages, whereas in secondary corticoadrenal insufficiency, a delayed but normal response is seen. Other tests may be performed to distinguish between various causes of hypoadrenalism, including renin and adrenocorticotropic hormone levels, as well as medical imaging – usually in the form of ultrasound, computed tomography or magnetic resonance imaging.[28]
Adrenoleukodystrophy, and the milder form, adrenomyeloneuropathy, cause adrenal insufficiency combined with neurological symptoms. These diseases are estimated to be the cause of adrenal insufficiency in about 35% of diagnosed males with idiopathic Addison's disease and should be considered in the differential diagnosis of any male with adrenal insufficiency. Diagnosis is made by a blood test to detect very long-chain fatty acids.[29]
Treatment
[edit]Maintenance
[edit]Treatment for Addison's disease involves replacing the missing cortisol, sometimes in the form of hydrocortisone tablets, or prednisone tablets in a dosing regimen that mimics the physiological concentrations of cortisol. Alternatively, one-quarter as much prednisolone may be used for equal glucocorticoid effect as hydrocortisone. Treatment is usually lifelong. In addition, many people require fludrocortisone as a replacement for the missing aldosterone.[19]
People with Addison's are often advised to carry information on them (e.g., in the form of a MedicAlert bracelet or information card) for the attention of emergency medical services personnel who might need to attend to their needs.[30][31] A needle, syringe, and injectable form of cortisol are also recommended to be carried for emergencies.[31] People with Addison's disease are advised to increase their medication during periods of illness or when undergoing surgery or dental treatment.[31] Immediate medical attention is needed when severe infections, vomiting, or diarrhea occur, as these conditions can precipitate an Addisonian crisis. A person who is vomiting may require injections of hydrocortisone, instead.[32]
Those with low aldosterone levels may also benefit from a high-sodium diet. It may also be beneficial for the people with Addison's disease to increase their dietary intake of calcium and vitamin D. High dosages of corticosteroids are linked to osteoporosis so these may be necessary for bone health.[33] Sources of calcium include dairy products, leafy greens, and fortified flours among many others.[34] Vitamin D can be obtained through the sun, oily fish, red meat, and egg yolks among many others. Though there are many sources to obtain vitamin D through diet, supplements are also an option.[35]
Crisis
[edit]Standard therapy involves intravenous injections of glucocorticoids and large volumes of intravenous saline solution with dextrose (glucose). This treatment usually brings rapid improvement. If intravenous access is not immediately available, intramuscular injection of glucocorticoids can be used. When the person is capable of swallowing fluids and medications by mouth, the amount of glucocorticoids is decreased until a maintenance dose is reached. If aldosterone is deficient, maintenance therapy also includes oral doses of fludrocortisone acetate.[36]
Prognosis
[edit]Outcomes are typically good when treated. Most people can expect to live relatively normal lives. Someone with the disease should be observant of symptoms of an "Addison's crisis" while the body is strained, as in rigorous exercise or being sick, the latter often needing emergency treatment with intravenous injections to treat the crisis.[11]
Individuals with Addison's disease have more than a doubled mortality rate.[37] Furthermore, individuals with Addison's disease and diabetes mellitus have an almost four-fold increase in mortality compared to individuals with only diabetes.[38] The risk ratio for cause mortality in males and females is 2.19 and 2.86, respectively.[37]
Death for individuals with Addison's disease often occurs due to cardiovascular disease, infectious disease, and malignant tumors, among other possibilities.[37]
Epidemiology
[edit]The frequency rate of Addison's disease in the human population is sometimes estimated at one in 100,000.[39] Some put the number closer to 40–144 cases per million population (1/25,000–1/7,000).[1][40][41] Addison's can affect persons of any age, sex, or ethnicity, but it typically presents in adults between 30 and 50 years of age.[41][42] Research has shown no significant predispositions based on ethnicity.[40] About 70% of Addison's disease diagnoses occur due to autoimmune reactions, which cause damage to the adrenal cortex.[5]
History
[edit]Addison's disease is named after Thomas Addison, the British physician who first described the condition in On the Constitutional and Local Effects of Disease of the Suprarenal Capsules (1855).[43][44] He originally described it as "melasma suprarenale", but later physicians gave it the medical eponym "Addison's disease" in recognition of Addison's discovery.[45]
While the six under Addison in 1855 all had adrenal tuberculosis,[46] the term "Addison's disease" does not imply an underlying disease process.
The condition was initially considered a form of anemia associated with the adrenal glands. Because little was known at the time about the adrenal glands (then called "Supra-Renal Capsules"), Addison's monograph describing the condition was an isolated insight. As the adrenal function became better known, Addison's monograph became known as an important medical contribution and a classic example of careful medical observation.[47] Tuberculosis used to be a major cause of Addison's disease and acute adrenal failure worldwide. It remains a leading cause in developing countries today.[5]
US president John F. Kennedy (1917–1963) suffered from complications of Addison's disease throughout his life, including during his presidency, resulting in fatigue and hyperpigmentation of the face. He is possibly the most famous known case.
Other animals
[edit]Hypoadrenocorticism is uncommon in dogs,[48] and rare in cats, with less than 40 known feline cases worldwide, since first documented in 1983.[49][50] Individual cases have been reported in a grey seal,[51] a red panda,[52] a flying fox,[53] and a sloth.[54]
In dogs, hypoadrenocorticism has been diagnosed in many breeds.[48] Vague symptoms, which wax and wane, can cause delay in recognition of the presence of the disease.[55] Female dogs appear more affected than male dogs, though this may not be the case in all breeds.[55][56] The disease is most often diagnosed in dogs that are young to middle-aged, but it can occur at any age from 4 months to 14 years.[55] Treatment of hypoadrenocorticism must replace the hormones (cortisol and aldosterone) which the dog cannot produce itself.[57] This is achieved either by daily treatment with fludrocortisone, or monthly injections with desoxycorticosterone pivalate (DOCP) and daily treatment with a glucocorticoid, such as prednisone.[57] Several follow-up blood tests are required so the dose can be adjusted until the dog is receiving the correct amount of treatment, because the medications used in the therapy of hypoadrenocorticism can cause excessive thirst and urination if not prescribed at the lowest effective dose.[57] In anticipation of stressful situations, such as staying in a boarding kennel, dogs require an increased dose of prednisone.[57] Lifelong treatment is required, but the prognosis for dogs with hypoadrenocorticism is very good.[55]
Hypoadrenocorticism can also occur in cats but is extremely rare. It is usually caused by an immune reaction, resulting in adrenal insufficiency. An ACTH stimulation test is used to diagnosis the condition.[58]
References
[edit]- ^ a b c d e f g h i j k l m n o p q r s t u v w x y "Adrenal Insufficiency and Addison's Disease". National Institute of Diabetes and Digestive and Kidney Diseases. May 2014. Archived from the original on 13 March 2016. Retrieved 13 March 2016.
- ^ a b Napier C, Pearce SH (June 2014). "Current and emerging therapies for Addison's disease". Current Opinion in Endocrinology, Diabetes, and Obesity. 21 (3). Lippincott Williams & Wilkins Ltd.: 147–153. doi:10.1097/med.0000000000000067. PMID 24755997. S2CID 13732181. Archived from the original on 2019-10-31. Retrieved 2019-10-31.
- ^ a b Brandão Neto RA, de Carvalho JF (2014). "Diagnosis and classification of Addison's disease (autoimmune adrenalitis)". Autoimmunity Reviews. 13 (4–5): 408–411. doi:10.1016/j.autrev.2014.01.025. PMID 24424183.
- ^ Oelkers W (2000). "Clinical diagnosis of hyper- and hypocortisolism". Noise & Health. 2 (7): 39–48. PMID 12689470. Archived from the original on 2022-08-10. Retrieved 2021-03-03.
- ^ a b c d "Addison's Disease". NORD (National Organization for Rare Disorders). Archived from the original on 2022-06-15. Retrieved 2020-12-01.
- ^ a b Kuo B, Koransky A, Vaz Wicks CL (2023-03-01). "Adrenal Crisis as An Adverse Reaction to Zoledronic Acid in a Patient With Primary Adrenal Insufficiency: A Case Report and Literature Review". AACE Clinical Case Reports. 9 (2): 32–34. doi:10.1016/j.aace.2022.12.003. PMC 10086596. PMID 37056413.
- ^ a b Hellesen A, Bratland E (January 2019). "The potential role for infections in the pathogenesis of autoimmune Addison's disease". Clinical and Experimental Immunology. 195 (1): 52–63. doi:10.1111/cei.13207. PMC 6300649. PMID 30144040.
- ^ Adam A (2014). Grainger & Allison's Diagnostic Radiology (6 ed.). Elsevier Health Sciences. p. 1031. ISBN 9780702061288. Archived from the original on 14 March 2016.
- ^ Napier C, Pearce SH (December 2012). "Autoimmune Addison's disease". Presse Médicale. 41 (12 P 2). Elsevier: e626–e635. doi:10.1016/j.lpm.2012.09.010. PMID 23177474.
- ^ Rajagopalan SR, Longmore M, Wilkinson IB (2006). Mini Oxford handbook of clinical medicine (6 ed.). Oxford: Oxford University Press. p. 312. ISBN 9780198570714. Archived from the original on 14 March 2016.
- ^ a b "Addison's disease – Treatment". NHS Choices. Archived from the original on 9 October 2016. Retrieved 8 October 2016.
- ^ a b c d e f Ten S, New M, Maclaren N (July 2001). "Clinical review 130: Addison's disease 2001". The Journal of Clinical Endocrinology and Metabolism. 86 (7): 2909–2922. doi:10.1210/jcem.86.7.7636. PMID 11443143.
- ^ Rose NR, Mackay IR (2014). The autoimmune diseases (5 ed.). San Diego, CA: Elsevier Science. p. 605. ISBN 9780123849304. Archived from the original on 14 March 2016.
- ^ a b c d e Øksnes M, Husebye ES (July 2023). "Approach to the patient: Diagnosis of primary adrenal insufficiency in adults". J Clin Endocrinol Metab. 109 (1): 269–278. doi:10.1210/clinem/dgad402. PMC 10735307. PMID 37450570. S2CID 259904961.
- ^ a b c d e Hahner S, Ross RJ, Arlt W, Bancos I, Burger-Stritt S, Torpy DJ, et al. (March 2021). "Adrenal insufficiency". Nat Rev Dis Primers. 7 (1): 19. doi:10.1038/s41572-021-00252-7. PMID 33707469. S2CID 232173232.
- ^ a b Younes N, Bourdeau I, Lacroix A (2021). "Latent Adrenal Insufficiency: From Concept to Diagnosis". Front Endocrinol (Lausanne). 12: 720769. doi:10.3389/fendo.2021.720769. PMC 8429826. PMID 34512551.
- ^ "Autoimmune polyglandular syndrome type 1 | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Archived from the original on 12 April 2017. Retrieved 26 June 2017.
- ^ "Autoimmune polyglandular syndrome type 2 | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Archived from the original on 13 April 2017. Retrieved 26 June 2017.
- ^ a b "Adrenal Insufficiency and Addison's Disease". The Lecturio Medical Concept Library. Archived from the original on 31 March 2022. Retrieved 27 June 2021.
- ^ "Addison's Disease". National Endocrine and Metabolic Diseases Information Service. Archived from the original on 28 October 2007. Retrieved 26 October 2007.
- ^ Bancos I, Hahner S, Tomlinson J, Arlt W (March 2015). "Diagnosis and management of adrenal insufficiency" (PDF). The Lancet. Diabetes & Endocrinology. 3 (3): 216–226. doi:10.1016/s2213-8587(14)70142-1. PMID 25098712. Archived (PDF) from the original on 2023-05-20. Retrieved 2023-05-05.
- ^ Dineen R, Thompson CJ, Sherlock M (2019-06-13). "Adrenal crisis: prevention and management in adult patients". Therapeutic Advances in Endocrinology and Metabolism. 10: 2042018819848218. doi:10.1177/2042018819848218. PMC 6566489. PMID 31223468.
- ^ Winqvist O, Karlsson FA, Kämpe O (June 1992). "21-Hydroxylase, a major autoantigen in idiopathic Addison's disease". Lancet. 339 (8809): 1559–1562. doi:10.1016/0140-6736(92)91829-W. PMID 1351548. S2CID 19666235.
- ^ Husebye ES, Perheentupa J, Rautemaa R, Kämpe O (May 2009). "Clinical manifestations and management of patients with autoimmune polyendocrine syndrome type I". Journal of Internal Medicine. 265 (5): 514–529. doi:10.1111/j.1365-2796.2009.02090.x. PMID 19382991. S2CID 205339997.
- ^ Kennedy R. "Addison's Disease". The Doctors' Medical Library. Archived from the original on 12 April 2013. Retrieved 10 April 2013.
- ^ Dorin RI, Qualls CR, Crapo LM (August 2003). "Diagnosis of adrenal insufficiency". Annals of Internal Medicine. 139 (3): 194–204. doi:10.7326/0003-4819-139-3-200308050-00017. PMID 12899587.
- ^ Holt EH (2008). "ACTH (cosyntropin) stimulation test". MedLine Plus. U.S. National Library of Medicine. Archived from the original on 2016-07-05. Retrieved 2021-06-27.
- ^ a b "Addison's Disease". wasiclinic. 2021-07-14. Retrieved 2022-05-27.[permanent dead link]
- ^ Laureti S, Casucci G, Santeusanio F, Angeletti G, Aubourg P, Brunetti P (February 1996). "X-linked adrenoleukodystrophy is a frequent cause of idiopathic Addison's disease in young adult male patients". The Journal of Clinical Endocrinology and Metabolism. 81 (2): 470–474. doi:10.1210/jcem.81.2.8636252. PMID 8636252.
- ^ Quinkler M, Dahlqvist P, Husebye ES, Kämpe O (January 2015). "A European Emergency Card for adrenal insufficiency can save lives". European Journal of Internal Medicine. 26 (1): 75–76. doi:10.1016/j.ejim.2014.11.006. PMID 25498511.
- ^ a b c Michels A, Michels N (April 2014). "Addison disease: early detection and treatment principles". American Family Physician. 89 (7): 563–568. PMID 24695602. Archived from the original on 5 September 2015.
- ^ White K (28 July 2004). "What to do in an emergency – Addisonian crisis". Addison's Disease Self Help Group. Archived from the original on 4 March 2016. Retrieved 28 January 2013.
- ^ "Eating, Diet, and Nutrition for Adrenal Insufficiency & Addison's Disease | NIDDK". National Institute of Diabetes and Digestive and Kidney Diseases. Archived from the original on 2021-01-09. Retrieved 2020-12-03.
- ^ "Office of Dietary Supplements - Calcium". ods.od.nih.gov. Archived from the original on 2018-03-17. Retrieved 2024-06-17.
- ^ "Office of Dietary Supplements - Vitamin D". ods.od.nih.gov. Archived from the original on 2021-04-09. Retrieved 2024-06-17.
- ^ "Adrenal Insufficiency and Addison's Disease". National Endocrine and Metabolic Diseases Information Service. Archived from the original on 26 April 2011. Retrieved 26 November 2010.
- ^ a b c Bergthorsdottir R, Leonsson-Zachrisson M, Odén A, Johannsson G (December 2006). "Premature mortality in patients with Addison's disease: a population-based study". The Journal of Clinical Endocrinology and Metabolism. 91 (12): 4849–4853. doi:10.1210/jc.2006-0076. PMID 16968806.
- ^ Chantzichristos D, Persson A, Eliasson B, Miftaraj M, Franzén S, Bergthorsdottir R, et al. (1 April 2016). "Patients with Diabetes Mellitus Diagnosed with Addison´s Disease Have a Markedly Increased Additional Risk of Death". Cushing Syndrome and Primary Adrenal Disorders. Meeting Abstracts. Endocrine Society. Archived from the original on 9 June 2021. Retrieved 9 June 2021.
- ^ "Addison Disease". MedicineNet. Archived from the original on 24 June 2007. Retrieved 25 July 2007.
- ^ a b Odeke S. "Addison Disease". eMedicine. Archived from the original on 7 July 2007. Retrieved 25 July 2007.
- ^ a b "Addison's disease". nhs.uk. 2018-06-22. Archived from the original on 2020-10-02. Retrieved 2020-10-14.
- ^ Volpé R (1990). Autoimmune Diseases of the Endocrine System. CRC Press. p. 299. ISBN 978-0-8493-6849-3.
- ^ Addison T (1855). On The Constitutional And Local Effects Of Disease Of The Supra-Renal Capsules. London: Samuel Highley. Archived from the original on 14 April 2005.
{{cite book}}: CS1 maint: unfit URL (link) - ^ Bancos I, Hahner S, Tomlinson J, Arlt W (2014-08-03). "Diagnosis and management of adrenal insufficiency". The Lancet Diabetes & Endocrinology. 3 (3): 216–226. doi:10.1016/s2213-8587(14)70142-1. ISSN 2213-8587. PMID 25098712. Archived from the original on 2024-07-01. Retrieved 2023-04-22.
- ^ Physician and Surgeon. Keating & Bryant. 1885. Archived from the original on 2024-07-01. Retrieved 2020-08-18.
- ^ Patnaik MM, Deshpande AK (May 2008). "Diagnosis--Addison's disease secondary to tuberculosis of the adrenal glands". Clinical Medicine & Research. 6 (1): 29. doi:10.3121/cmr.2007.754a. PMC 2442022. PMID 18591375.
- ^ Bishop PM (January 1950). "The history of the discovery of Addison's disease". Proceedings of the Royal Society of Medicine. 43 (1): 35–42. doi:10.1177/003591575004300105. PMC 2081266. PMID 15409948.
- ^ a b Klein SC, Peterson ME (January 2010). "Canine hypoadrenocorticism: part I". The Canadian Veterinary Journal. 51 (1): 63–69. PMC 2797351. PMID 20357943.
- ^ Drobatz KJ, Costello MF (2010). Feline Emergency & Critical Care Medicinem. Ames, Iowa: Blackwell Publ. pp. 422–424.
- ^ Tofte KL (2018). "Chapter 111. Hypoadrenocorticism". In Norsworthy GD (ed.). The Feline Patient. John Wiley & Sons. p. 324. ISBN 9781119269038.
- ^ Stringfield CE, Garne M, Holshuh HJ (2000). Addison's disease in a gray seal (Halichoerus grypus). International Association for Aquatic Animal Medicine Proceedings. Archived from the original on 2021-08-27. Retrieved 2018-08-25.
- ^ Sohn P (10 February 2012). "Endangered red panda dies at Chattanooga Zoo". Times Free Press. Archived from the original on 26 August 2018. Retrieved 25 August 2018.
- ^ Brock AP, Hall NH, Cooke KL, Reese DJ, Emerson JA, Wellehan JF (June 2013). "Diagnosis and management of atypical hypoadrenocorticism in a variable flying fox (Pteropus hypomelanus)". Journal of Zoo and Wildlife Medicine. 44 (2): 517–519. doi:10.1638/2012-0276R2.1. PMID 23805580. S2CID 38918707.
- ^ Kline S, Rooker L, Nobrega-Lee M, Guthrie A (March 2015). "Hypoadrenocorticism (Addison's disease) in a Hoffmann's two-toed sloth (Choloepus hoffmanni)". Journal of Zoo and Wildlife Medicine. 46 (1): 171–174. doi:10.1638/2014-0003R2.1. PMID 25831596. S2CID 20775341.
- ^ a b c d Scott-Moncrieff JC (2015). "Chapter 12: Hypoadrenocorticism". In Feldman EC, Nelson RW, Reusch CE, Scott-Moncrieff JC (eds.). Canine and Feline Endocrinology (4th ed.). Saunders Elsevier. pp. 485–520. ISBN 978-1-4557-4456-5.
- ^ Boag AM, Catchpole B (December 2014). "A review of the genetics of hypoadrenocorticism". Topics in Companion Animal Medicine. 29 (4): 96–101. doi:10.1053/j.tcam.2015.01.001. PMID 25813849. Archived from the original on 2022-09-28. Retrieved 2023-01-03.
- ^ a b c d Lathan P, Thompson AL (2018). "Management of hypoadrenocorticism (Addison's disease) in dogs". Veterinary Medicine: Research and Reports. 9: 1–10. doi:10.2147/VMRR.S125617. PMC 6055912. PMID 30050862.
- ^ https://vcahospitals.com/know-your-pet/addisons-disease-in-cats
